How the Membrane Attack Complex Damages the Bacterial Cell Envelope and Kills Gram-Negative Bacteria The human immune system can directly lyse invading micro-organisms and aberrant host cells by generating pores in the cell envelope, called membrane attack complexes (MACs).
How does the membrane attack complex kill bacteria?
How the Membrane Attack Complex Damages the Bacterial Cell Envelope and Kills Gram-Negative Bacteria The human immune system can directly lyse invading micro-organisms and aberrant host cells by generating pores in the cell envelope, called membrane attack complexes (MACs).
How does the membrane attack complex (MAC) work?
The membrane attack complex (MAC) punches a hole through the plasma membrane of the target cell, killing the pathogen. Found in Membrane Attack complex in Wikipedia. A rare but interesting human disease is associated with a malfunction of the MAC.
What can the membrane attack complex lyse?
The Membrane Attack Complex Can Lyse a Broad Spectrum of Cells. The membrane-attack complex formed by complement activation can lyse gram-negative bacteria, parasites, viruses, erythrocytes, and nucleated cells.
What is the pathophysiology of membrane attack complex?
The membrane attack complex is initiated when the complement protein C5 convertase cleaves C5 into C5a and C5b. All three pathways of the complement system ( classical, lectin and alternative pathways) initiate the formation of MAC.

How does membrane attack complex works?
In response to complement activation, the membrane attack complex (MAC) assembles from fluid-phase proteins to form pores in lipid bilayers. MAC directly lyses pathogens by a 'multi-hit' mechanism; however, sublytic MAC pores on host cells activate signalling pathways.
How does the membrane attack complex or MAC kill Gram-negative bacteria?
Gram-negative bacteria are refractory to the action of many antibiotics due to their impermeable outer membrane. An important player of the immune system is the complement system, a protein network in serum that directly kills Gram-negative bacteria through pore-formation by the Membrane Attack Complexes (MAC).
Does the membrane attack complex kill viruses?
The multiprotein membrane attack complex is a bactericidal weapon of the innate immune system that also modulates inflammation and proliferation when formed on self-cells1. The MAC pore targets a wide range of pathogens, forming on and killing Gram-negative bacteria2, enveloped viruses3, and parasites4.
What effect does the membrane attack complex have on bacteria?
(a) The role of the membrane attack complex MAC can form on and directly kill Gram-negative bacteria [2,3]. It is particularly important in combatting Neisseria meningitidis, with genetic deficiencies in MAC components leading to recurrent infections [4–6].
How does MAC kill?
In conclusion, when the MAC is assembled from purified C5‐C9 by surface‐bound convertases, these pores trigger inner membrane damage and subsequent bacterial killing.
How does the membrane attack complex MAC help cause this?
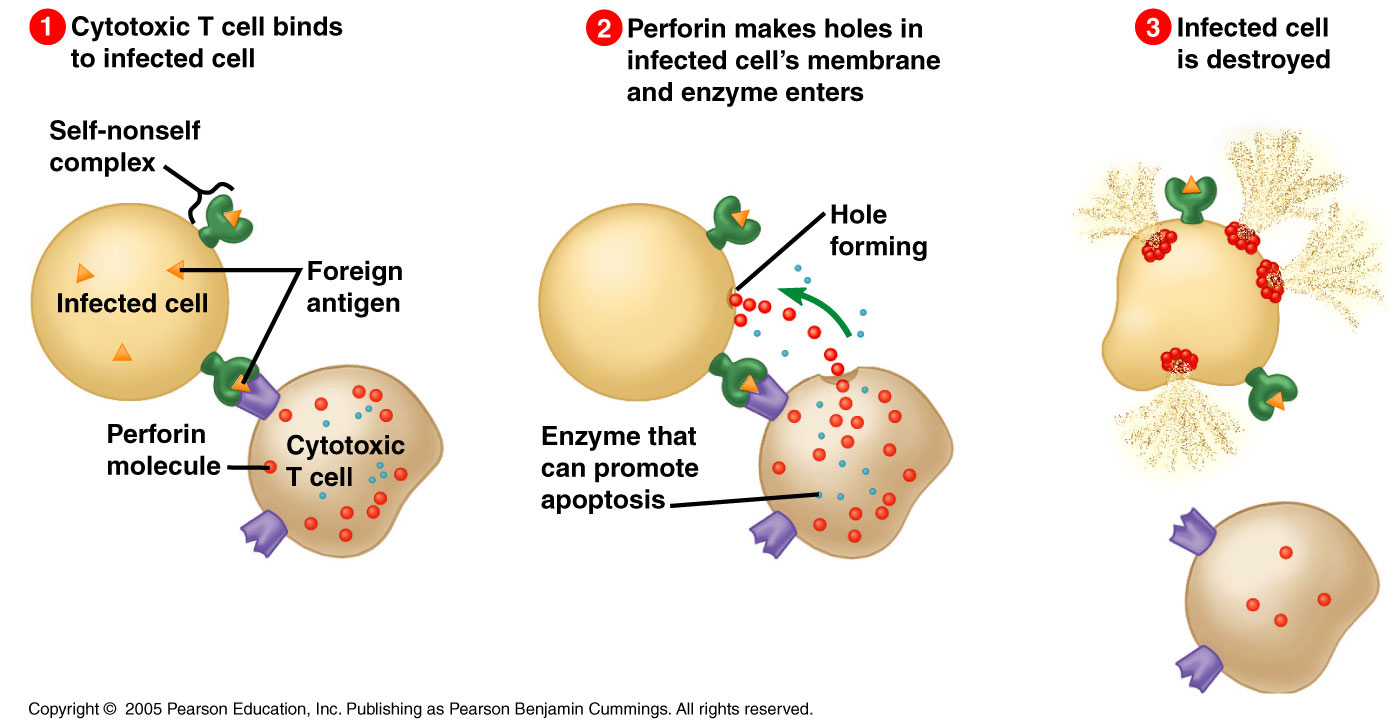
Antibody-mediated complement activation leads to MAC deposition on the surface of infected cells. Assembly of the MAC leads to pores that disrupt the cell membrane of target cells, leading to cell lysis and death.
What is the membrane attack complex made of?
Membrane attack complex (MAC) is an important immune effector of the complement terminal pathway that is composed of complement components C5b, C6, C7, C8, and C9.
What forms the membrane attack complex?
The soluble membrane attack complex (sMAC, a.k.a., sC5b-9 or TCC) is generated on activation of complement and contains the complement proteins C5b, C6, C7, C8, C9 together with the regulatory proteins clusterin and/or vitronectin.
Does complement kill viruses?
Being a major first line of immune defense, the complement system keeps a constant vigil against viruses. Its ability to recognize large panoply of viruses and virus-infected cells, and trigger the effector pathways, results in neutralization of viruses and killing of the infected cells.
What is the end result of the formation of the membrane attack complex by complement proteins?
These comprise a sequence of polymerization reactions in which the terminal complement components interact to form a membrane-attack complex, which creates a pore in the cell membranes of some pathogens that can lead to their death.
How is complement involved in bacterial killing?
Complement is a complex protein network of plasma, and an integral part of the innate immune system. Complement activation results in the rapid clearance of bacteria by immune cells, and direct bacterial killing via large pore-forming complexes.
What membrane component makes it difficult to destroy ecoli?
The inner membrane of E. coli contains several multidrug efflux pumps which differ in their structures and mechanisms. The major efflux pump responsible for the intrinsic resistance of E. coli to antibiotics is AcrAB-TolC (7).
Why are gram positive bacteria less susceptible to membrane attack complexes?
Concomitant generation of C5b triggers the assembly of the MAC (C5b-9) (Fig. 1a); this specifically kills Gram-negative bacteria. Gram-positive bacteria are protected from MAC-dependent killing, likely because their thick peptidoglycan outer layer prevents insertion of the MAC into the cell membrane [16].
What are the 3 functions of the complement system?
At the basic level the broad functions of the complement system can be split into three areas: (1) the activation of inflammation; (2) the opsonization (labeling) of pathogens and cells for clearance/destruction; (3) the direct killing of target cells/microbes by lysis.
What membrane component makes it difficult to destroy ecoli?
The inner membrane of E. coli contains several multidrug efflux pumps which differ in their structures and mechanisms. The major efflux pump responsible for the intrinsic resistance of E. coli to antibiotics is AcrAB-TolC (7).
What does MAC do to bacteria?
These convertase-generated MAC pores can subsequently efficiently damage the bacterial inner membrane (IM), which is essential for bacterial killing. This review summarizes these recent insights of MAC assembly and discusses how MAC pores kill Gram-negative bacteria.
How does MAC protect against infection?
The MAC plays a role in host defense processes through its ability to kill certain microorganisms and to promote inflammation. The function of the MAC in protection against infections is best demonstrated in individuals with homozygous deficiency of a MAC protein. These individuals have increased susceptibility to develop disseminated disease when infected with the gram-negative organism Neisseria gonorrhoeae or N. meningitidis. Thus killing by the MAC must be essential to maintain localization and prevent dissemination of neisserial infections. Other gram-negative bacteria, but not gram-positive bacteria, may be killed by the MAC; however, susceptibility is variable. In general smooth strains, but not rough strains, are resistant to killing because they are protected from the MAC by long-chain lipopolysaccharides. For bactericidal activity the deposits of MAC on the bacterial surface must contain at least three molecules of C9 per C5b–8. Enveloped viruses and parasites may also be susceptible to the cytotoxic effect of the MAC. The poor susceptibility to MAC-mediated killing of many microorganisms is due to their defense mechanisms against complement, including certain surface proteins that are homologous to human complement inhibitors.
What is smac in human disease?
sMAC is known to activate the caspase pathway and apoptosis, as wells as transendothelial migration of polymorphonuclear leucocytes that most likely contribute s to the glomerular injury. From: Pathobiology of Human Disease, 2014. Download as PDF. About this page.
What is the role of MAC in cellular responses?
The MAC is endowed with the potential to inflict damage on cell membranes that may result in cell death and to induce cellular responses that are generally proinflammatory . These activities may participate significantly in varied physiologic and pathologic processes. Induction of cell damage is a consequence of the ability of the MAC to generate ion-permeable channels in the cell membrane. Membrane-bound C5b–8 can lyse red cells at a low rate but this process is enhanced by C9. Because of the strong affinity of C5b–8 for phospholipids, the membrane bilayer is disrupted, causing increased permeability, which is further enhanced by larger channels formed by addition of C9. Addition of one C9 molecule per C5b–8 is sufficient for rapid lysis of red cells. The permeability changes may cause osmotic swelling and lysis of red cells. Red cells are able to offer some resistance to osmotic swelling by means of a Ca2+ -activated K + channel and may repair lesions through a Ca 2+ -dependent vesiculation process. Killing of nucleated cells by the MAC is independent of permeability changes and is associated with an increase in cellular Ca 2+ and intracellular lipid metabolism, mitochondrial swelling, and hydrolysis of membrane lipids. Nucleated cells are capable of defending themselves from the cytotoxic effect of the MAC and, consequently, lysis is achieved only when large numbers of MAC with multiple C9 are deposited on the plasma membrane. Sublytic amounts of MAC induce activation of the target cell, which, among other effects, results in energy-dependent elimination of membrane-bound MAC by endocytosis or exocytosis. This process requires extracellular Ca2+, with participation of protein kinase C (PKC) and cAMP. Cells with increased levels of cAMP are resistant to MAC-mediated killing. Conversely, inhibition of protein synthesis or lipid metabolism increases susceptibility to MAC-mediated killing.
What is the MAC inhibitor?
MAC synthesis is inhibited by CD59 (also known as MAC-inhibitory protein, or protectin) found on the surface of normal human cells. CD59 is an example of a glycosyl phosphatidylinositol (GPI)–linked protein (see Chapter 6 ).
What is the MAC in bacteria?
The MAC forms trans–plasma membrane channels on the surface of pathogenic bacteria, causing cell lysis and death [34]. The bacteria are first identified and tagged by antibodies that attach to specific bacteria-surface carbohydrates. This response stimulates the complement cascade leading to generation of the MAC.
What are the effects of MAC on inflammation?
C5b–8 and C5b–9 in sublytic amounts can activate several transduction pathways mainly through the participation of Ca 2+ which first enters the cell through the MAC pore and then triggers the release of Ca 2+ from intracellular organelles. Transduction pathways that are Ca 2+ -independent may also be activated. The MAC can induce activation of PKC and stimulate phosphoinositide metabolism, with increased production of IP 1, IP 2 and IP 3, and increase the intracellular concentration of sn -1,2-diacylglycerol . The MAC can also interact with pertussis toxin-sensitive guanine nucleotide-binding proteins (G proteins). C5b–9 causes arachidonic acid release, which in part requires external Ca 2+, resulting in production of DAG, which may activate PKC and thus stimulate phospholipase A 2. The MAC may induce cell cycle in oligodendrocytes, which involves c- jun activation, and can also cause hydrolysis of myelin basic protein.
What is the role of C5B-9 in the cell cycle?
C5b–9 causes arachidonic acid release , which in part requires external Ca2+, resulting in production of DAG, which may activate PKC and thus stimulate phospholipase A 2. The MAC may induce cell cycle in oligodendrocytes, which involves c-jun activation, and can also cause hydrolysis of myelin basic protein.
What is the membrane attack complex?
The membrane attack complex is initiated when the complement protein C5 convertase cleaves C5 into C5a and C5b. All three pathways of the complement system ( classical, lectin and alternative pathways) initiate the formation of MAC.
What happens if C5B-7 does not insert into the cell membrane?
If the pre-MAC complexes of C5b-7, C5b-8 or C5b-9 do not insert into a membrane, they can form inactive complexes with Protein S (sC5b-7, sC5b-8 and sC5b-9). These fluid phase complexes do not bind to cell membranes and are ultimately scavenged by clusterin and vitronectin, two regulators of complement.
What is the C5B-6-7-8 complex?
The C5b-6-7 complex binds to C8, which is composed of three chains (alpha, beta, and gamma), thus forming the C5b-6-7-8 complex. C5b-6-7-8 subsequently binds to C9 and acts as a catalyst in the polymerization of C9.
Which complex is bound by C7?
The C5bC6 complex is bound by C7 .
Which molecule has a hydrophobic external face?
C8 alpha-gamma has the hydrophobic area that inserts into the bilayer. C8 alpha-gamma induces the polymerization of 10-16 molecules of C9 into a pore-forming structure known as the membrane attack complex. MAC has a hydrophobic external face allowing it to associate with the lipid bilayer.
Does C5 to C9 cause Neisseria?
Deficiencies of C5 to C9 components do not lead to a generalized susceptibility to infections but only to an increased susceptibility to Neisseria infections, since Neisseria have a thin cell wall and little to no glycocalyx.
Why are complex systems of regulation necessary?
Complex systems of regulation are necessary to protect host cells from the activated complement complexes generated to lyse intruders. all—enveloped viruses are susceptible to complement-mediated lysis. The viral envelope is largely derived from the plasma membrane of infected host cells and is therefore susceptible to pore formation by ...
Which anchors are attached to amino acid residues in proteins?
While most proteins that are expressed on the surface of cells have hydrophobic sequences that traverse the lipid bilayer in the cell membrane, some proteins are bound by glycol ipid anchors ( glycosyl phosphatidylinositol, or GPI) attached to amino acid residues in the protein.
What is the function of DAF and Mirl?
DAF and MIRL are cell-surface proteins that function as inhibitors of com plement-mediated cell lysis, but act at different stages of the process. DAF inhibits cell lysis by causing dissociation and inactivation of the C3 convertases of the classical, lectin, and alternative pathways (see Figure 13-9b). MIRL acts later in the pathway by binding ...
What is the clinical consequence of deficiency in DAF and MIRL?
PNH, the clinical consequence of deficiency in DAF and MIRL, is a chronic disease with a mean survival time between ...
Why are Gram positive bacteria resistant to complement mediated lysis?
Gram-positive bacteria are generally resistant to complement-mediated lysis because the thick peptidoglycan layer in their cell wall prevents insertion of the MAC into the inner membrane. Although complement activation can occur on the cell membrane of encapsulated bacteria such as Streptococcus pneumoniae, the capsule prevents interaction between ...
How is MAC prevented?
Insertion of MAC into bacterial membrane is prevented by thick layer of peptidoglycan
Which pathogens are susceptible to complement mediated lysis?
Among the pathogenic viruses susceptible to lysis by complement-mediated lysis are herpesviruses, orthomyxoviruses, paramyxoviruses, and retroviruses.