Explore
How is hyperosmolar hyperglycemic syndrome (HHS) treated? To treat HHS, your doctor will give you intravenous (IV) medications. These include: Fluids to hydrate you. Electrolytes (such as potassium) to balance the minerals in your body. Insulin to control your blood sugar levels.
How is hyperosmolar hyperglycemic syndrome (HHS) treated?
Treatment Hyperglycemic hyperosmolar nonketotic syndrome (HHNS) is a potentially deadly condition that can develop as a result of infection or illness in people with uncontrolled type 2 diabetes or when diabetes medications aren't taken as directed. Some also refer to this as a "diabetic coma."
What is hyperglycemic hyperosmolar nonketotic syndrome?
Treatment typically involves starting intravenous fluids (saline solution) to rehydrate the body quickly. It may also require IV insulin to bring down the blood sugar levels. Potassium replenishment may also be required depending on blood potassium levels.
What are the treatment options for hyperglycemia?
What are the symptoms of hyperosmolar hyperglycemic syndrome (HHS)? Symptoms of HHS usually come on slowly, and can take days or weeks to develop. Symptoms include: High blood sugar level (over 600 mg/dL). Confusion, hallucinations, drowsiness or passing out. Dry mouth and extreme thirst that may eventually get better. Frequent urination.
What are the symptoms of hyperosmolar hyperglycemic syndrome?

What is the immediate aim of treatment for HHNS?
Patients presenting with HHNS also have significant depletion of potassium and other electrolytes that will need to be replaced. The principal goal at the outset of therapy must be restoration of the intravascular volume to assure adequate perfusion of vital organs.
What is the initial treatment for a patient experiencing hyperosmolar hyperglycemic nonketotic coma HHNC )?
Hyperosmolar hyperglycemic state is diagnosed by severe hyperglycemia and plasma hyperosmolality and absence of significant ketosis. Treatment is IV saline solution and insulin. Complications include coma, seizures, and death.
What is the usual treatment procedure for correction of HHS?
Treatment of HHS Treatment is 0.9% (isotonic) saline solution; 1000 mL is given in the first hour. Smaller boluses (500 mL) can be given if there is risk for exacerbation of heart failure or volume overload. Additional boluses may be needed for hypotensive patients.
Do you treat HHS with insulin?
All patients with HHS require IV insulin therapy; however, immediate treatment with insulin is contraindicated in the initial management of patients with HHS. The osmotic pressure that glucose exerts within the vascular space contributes to the maintenance of circulating volume in these severely dehydrated patients.
What is the difference between DKA and HHNS?
DKA typically evolves within a few hours, whereas HHNS is much slower and occurs over days to weeks, according to 2021 research . The two conditions look similar because of the hyperglycemia component of each condition. Knowing the symptoms of each can help you seek medical care as soon as possible.
What type of insulin is used for HHS?
Insulin aspart (NovoLog)
Does HHS need insulin drip?
indications: who needs an insulin infusion? Not every patient with HHS necessarily requires an insulin infusion. In many patients, volume resuscitation plus subcutaneous insulin will be perfectly adequate to achieve glycemic control.
How do you know when HHS is resolved?
HHS is resolved when serum osmolality is < 320 mOsm/kg with a gradual recovery to mental alertness. The latter may take twice as long as to achieve blood glucose control. Ketonemia typically takes longer to clear than hyperglycemia.
Is HHS a medical emergency?
Symptoms of HHS can include extreme thirst, frequent urination, changes in your vision and confusion. HHS is an emergency and you should contact your healthcare provider immediately if you have these symptoms.
Why is dextrose given in HHS?
When the plasma glucose level reaches 300 mg/dl, insulin infusion may be reduced to 0.05-0.1 unit/kg/hour and dextrose can be added to the fluids to keep the glucose level between 250-300 mg/dl until hyperosmolality has resolved and the patient is alert.
Does HHS need ICU?
Patients with HHS are usually admitted to the hospital's intensive care unit (ICU) because they must be watched very closely as they recover. Once the patient's blood glucose levels improve and they are properly rehydrated, patients will be transitioned back to a regular diabetes treatment regimen to be taken at home.
Which IV fluid is best for hyperglycemia?
For adult patients with DKA, the American Diabetes Association recommends initial treatment with 1.0–1.5 L of 0.9% saline over 1 h, followed by continuous infusion with either 0.9% or 0.45% saline depending on serum sodium concentration [17].
What is hyperosmolar nonketotic coma?
Hyperglycaemic hyperosmolar non-ketotic coma is coma resulting from very high blood glucose levels in a patient with normal ketone levels. If very high blood glucose levels are combined with high ketone levels, the state is likely to be ketoacidosis.
Which of the following causes of hyperglycaemic hyperosmolar non Ketotic syndrome HHNS is most common?
Hyperosmolar hyperglycemic syndrome (HHS) is a clinical condition that arises from a complication of diabetes mellitus. Type 2 diabetes accounts for about 90% to 95% of diabetes cases. It is most commonly seen in patients with obesity.
Which of the following patient is most likely experiencing hyperglycemic hyperosmolar nonketotic syndrome based on their symptoms?
HHNS occurs mainly in type 2 diabetics. This condition presents without ketones in the urine.
What is diabetic hyperglycemic hyperosmolar syndrome?
Diabetic hyperglycemic hyperosmolar syndrome (HHS) is a complication of type 2 diabetes. It involves extremely high blood sugar (glucose) level without the presence of ketones.
How to reduce risk of HHS?
You can reduce your risk of developing HHS again by controlling your diabetes and managing your diet and lifestyle.
How to prevent HHS?
The best way to prevent HHS is by following a healthy lifestyle and managing your diabetes. You should:
What is the term for a person who has high blood sugar?
Hyperosmolar hyperglycemic syndrome ( HHS) is a serious complication of diabetes mellitus. HHS occurs when a person’s blood glucose (sugar) levels are too high for a long period, leading to severe dehydration (extreme thirst) and confusion.
What is the name of the condition where blood sugar levels are high for a long period of time?
Hyperosmolar Hyperglycemic Syndrome. A serious complication of diabetes mellitus, hyperosmolar hyperglycemic syndrome (HHS) happens when blood sugar levels are very high for a long period of time. Symptoms of HHS can include extreme thirst, frequent urination, changes in your vision and confusion.
What to do if you have symptoms of HHS?
If you have symptoms of HHS, you should drink plenty of water and call 911 or go to the emergency room immediately . You will receive an IV with fluids and insulin to relieve your symptoms.
Which type of diabetes is most affected by HHS?
HHS most often affects people who have type 2 diabetes who are:
How high is the blood sugar level for HHS?
Your doctor will examine you, ask about your symptoms, and order a blood test to check your blood sugar level. A very high blood sugar level (over 600 mg/dL) with low ketone levels (acids in blood and urine) will help the doctor make a diagnosis of HHS.
What are the symptoms of hyperglycemia?
Weakness or paralysis on one side of the body. Loss of vision. Hallucinations. If you have symptoms of extreme thirst, frequent urination, confusion, and blurry vision, it's important that you seek medical care immediately, as you could be experiencing symptoms of hyperglycemia, which may be life-threatening.
How to prevent HHNS?
The best way to prevent HHNS is by keeping your blood sugar levels under control. Test them regularly using a glucometer, work with your doctor to make sure you're taking any diabetes medications as prescribed, and learn the warning signs of elevated glucose levels and dehydration, such as extreme thirst and frequent urination, so you know to seek treatment when you need it. Educate your loved ones and coworkers to also recognize the early signs of blood sugar imbalance, so they can send for help, too.
What is HHNS in diabetes?
Hyperglycemic hyperosmolar nonketotic syndrome (HHNS) is a potentially deadly condition that can develop as a result of infection or illness in people with uncontrolled type 2 diabetes or when diabetes medications aren't taken as directed. Some also refer to this as a "diabetic coma.".
How to diagnose HHNS?
HHNS is diagnosed based on symptoms and by measuring blood glucose levels, which can be performed with a finger stick. A blood glucose level of 600 mg/dL and low ketone levels are the main factors for diagnosis of HHNS. Serum osmolality, a test that measures the body's water/electrolyte balance , also is used to diagnose HHNS.
Is HHNS a complication of diabetes?
HHNS is a relatively rare complication of diabetes, accounting for just 1% of hospital admissions among people with diabetes. 1
Can a 65 year old have HHNS?
Most people who experience HHNS are 65 and have type 2 diabetes. Young people with type 1 diabetes and children can be affected by HHNS as well, especially if they're obese, although this is uncommon.
Can you stay in hospital overnight with HHNS?
If you are hospitalized due to HHNS, you may be kept overnight for observation . The main goal of treatment of this condition is to identify the underlying factors, whether that's an infection, a certain medication, or poor blood sugar management.
What is Hyperosmolar Hyperglycemic Nonketotic Syndrome
The hyperosmolar hyperglycemic nonketotic syndrome is a life-threatening condition that occurs when blood sugar levels are extremely high. High glucose causes the blood to become hyperosmolar, meaning it has a higher than normal amount of solutes such as sodium and glucose.
Diabetes and HHNS
HHNS can affect both type 1 and type 2 diabetics, although it is most common among persons with type 2 diabetes. HHNS is generally by an illness or infection.
Symptoms
Symptoms of the hyperosmolar hyperglycemic nonketotic syndrome can vary from patient to patient. Some symptoms may include but are not in the limit to:
When to Seek a Doctor
If hyperosmolar hyperglycemic nonketotic syndrome symptoms last for more than 48 hours, you should immediately contact your doctor. This is because the hyperosmolar hyperglycemic nonketotic syndrome can be a sign of diabetes and if left untreated, this could lead to diabetic ketoacidosis or even coma which needs immediate medical attention.
Causes of Hyperosmolar Hyperglycemic Nonketotic Syndrome
In some cases, the hyperosmolar hyperglycemic nonketotic syndrome may be in connection to a hyperosmolar hyperglycemic state.
Diagnosis of the Hyperosmolar Hyperglycemic Nonketotic Syndrome
HMSN is identified by examining symptoms and measuring blood sugar levels, which can be done via a finger prick.
Side Effects of Treatment
The IV electrolytes or fluids used to deal with dehydration do not cause any problems. Insulin-induced side effects include:
What is hyperosmolar hyperglycemic syndrome?
Hyperosmolar hyperglycemic syndrome (HHS) is a clinical condition that arises from a complication of diabetes mellitus. This problem is most commonly seen in type 2 diabetes. Won Frerichs and Dreschfeld first described the disorder around 1880. They described patients with diabetes mellitus with profound hyperglycemia and glycosuria without the classic Kussmaul breathing or acetone in the urine seen in diabetic ketoacidosis. This clinical condition was formerly called non-ketotic hyperglycemic coma; hyperosmolar hyperglycemic non-ketotic syndrome, and hyperosmolar non-ketotic coma (HONK).[1]
Why do people with type 2 diabetes have HHS?
As stated earlier, HHS is most commonly seen in patients with type 2 diabetes. If diabetes mellitus is well controlled, the chance of developing HHS is minimal. However, under certain conditions, some factors might initiate the development of HHS. The most frequent reason for this complication is infection. The infectious process in the respiratory, gastrointestinal, and genitourinary systems can act as the causative factor. The reason for this is the insensible water loss and the release of endogenous catecholamines. Approximately 50% to 60% of HHS is attributable to an infectious etiology. [11][12][13]
Why should glucose levels be monitored?
The glucose level should be monitored hourly to guard against a sudden and precipitous drop, during treatment with isotonic fluid and insulin. This is to prevent the development of cerebral edema which is the most dreaded complication in both DKA and HHS. The risk of cerebral edema is higher in HHS.
What is the metabolic effect of diabetes mellitus?
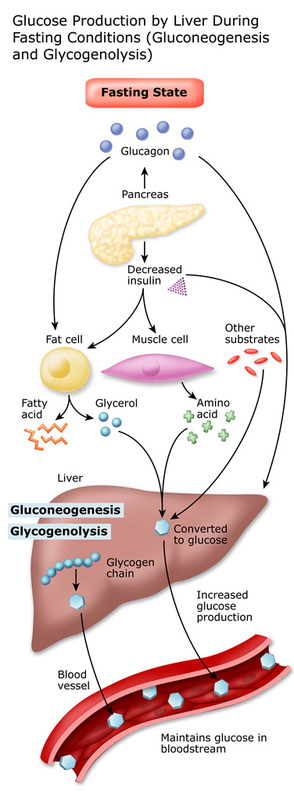
Diabetes mellitus is a clinical condition associated with hyperglycemia as the main metabolic disorder.[2] This is as a result of an absolute or relative deficiency of insulin. Insulin is an anabolic hormone produced by the beta cells of the islets of Langerhans in the pancreas. The main function of this hormone is to lower the level of glucose in the blood by promoting the uptake of glucose by the adipose tissue and skeletal muscle, known as glycogenesis. Insulin also inhibits the breakdown of fat in the adipose tissue, known as lipolysis. The metabolic effect of insulin is countered by hormones such as glucagon and catecholamines. [3]
Who developed the diagnostic criteria for HHS?
The diagnostic criteria for HHS were developed as a result of cases series reported by Gerich et al. Arieff and Carroll also contributed to this work in a separate study both of which were published in 1971. [27]
What is the clinical presentation of HHS?
The typical clinical presentation of patients with HHS is increased urination (polyuria) and increase water intake (polydipsia). This is a result of the stimulation of the thirst center in the brain from severe dehydration and increased serum osmolarity. Weakness, malaise, and lethargy can also be part of the complaints.
What to do if you have HHNS?
If you start to have symptoms of HHNS or DKA, call 911 or go to your local emergency room immediately. These are serious medical events that can lead to life threatening complications if left untreated.
What to do if you have symptoms of either condition?
If you have symptoms of either condition, seek emergency care immediately.
What is HHNS in medical terms?
Hyperglycemic hyperosmolar nonketotic syndrome (HHNS) is also known as hyperglycemic hyperosmolar syndrome (HHS). It involves very high blood sugar levels and can be life threatening.
Is DKA the same as HHNS?
Your treatment for DKA is similar to that of HHNS. The medical professional will:
Can you prevent HHNS?
While you might not always be able to prevent some causes of HHNS or DKA, like an illness or infection, there are steps you can take to reduce the risk of these conditions occurring. These include:
Is HHNS a life threatening condition?
While HHNS and D KA are serious medical conditions that can lead to life threatening complications, they are preventable and treatable, especially if you identify them early.
What is the most serious hyperglycemic emergency in patients with type 2 diabetes?
The hyperosmolar hyperglycemic state (HHS) is the most serious acute hyperglycemic emergency in patients with type 2 diabetes. von Frerichs and Dreschfeld described the first cases of HHS in the 1880s in patients with an “unusual diabetic coma” characterized by severe hyperglycemia and glycosuria in the absence of Kussmaul breathing, with a fruity breath odor or positive acetone test in the urine. Current diagnostic HHS criteria include a plasma glucose level >600 mg/dL and increased effective plasma osmolality >320 mOsm/kg in the absence of ketoacidosis. The incidence of HHS is estimated to be <1% of hospital admissions of patients with diabetes. The reported mortality is between 10 and 20%, which is about 10 times higher than the mortality rate in patients with diabetic ketoacidosis (DKA). Despite the severity of this condition, no prospective, randomized studies have determined best treatment strategies in patients with HHS, and its management has largely been extrapolated from studies of patients with DKA. There are many unresolved questions that need to be addressed in prospective clinical trials regarding the pathogenesis and treatment of pediatric and adult patients with HHS.
Why is HHNK replaced with hyperosmolar state?
The term HHNK was replaced with “hyperglycemic hyperosmolar state” to reflect the fact that many patients present without significant decline in the level of consciousness (less than one-third of patients present with coma) and because many patients can present with mild to moderate degrees of ketosis (32,60).
When was insulin first used in diabetic coma?
In 1973 , Alberti et al. (69) were the first to report the successful treatment of patients with diabetic coma using small intramuscular doses of regular insulin. They treated 14 patients with ketoacidosis, one patient with hyperosmolar nonketotic coma, and two cases of hyperglycemic nonketotic state with an initial mean dose of 16 ± 2 units followed by 5 or 10 units i.v. or i.m. every hour. The patients’ plasma glucose rates fell at a regular rate of 90 mg/h (69). The authors reported a cumulative insulin dose of <100 units per day, which was a significant reduction from previous reports that used 400–500 units per day. These studies were later confirmed by two randomized, controlled trials conducted by Kitabchi and colleagues (70,71), who compared treatment using low-dose intramuscular with treatment using large-dose intravenous and subcutaneous regular insulin (Table 3). Unfortunately, no prospective, randomized studies have been conducted in patients with HHS, and those patients are treated following the protocols designed to treat DKA. Low-dose insulin infusion protocols have been shown to be effective, with resolution of hyperglycemia in ∼9 ± 2 h and resolution of HHS in 11 ± 1 h (7).
What causes T1DM in children?
In children, most common precipitating causes are diseases of the circulatory, nervous, and genitourinary systems (52). In addition, some children with T1DM may present with features of HHS (severe hyperglycemia) if high-carbohydrate–containing beverages have been used to quench thirst and replace urinary losses prior to diagnosis (53).
What was Kussmaul's diagnosis of a diabetic coma?
In 1874, Kussmaul reported several fatal cases of diabetic coma preceded and accompanied by severe dyspnea (15,16). Kussmaul breathing, as this condition came to be known, quickly became one of the hallmarks in the diagnosis of diabetic coma, along with the presence of positive urine ketones (14,17).
What is the inflammatory state of hyperglycemia?
Severe hyperglycemia is associated with a severe inflammatory state characterized by an elevation of proinflammatory cytokines (tumor necrosis factor-α, interleukin (IL)β, IL6, and IL8) and reactive oxygen species, with insulin secretion and action.
Who first reported the diagnostic criteria of HHS?
Diagnostic criteria of HHS first reported by Arieff and Carroll and current ADA criteria
Which type of diabetics have HHNS?
A.)HHNS occurs mainly in type 2 diabetics.
What is the blood glucose level of a 69 year old diabetic?
C.) A 69 year old admitted with an infection of the right foot with a health history of diabetes that reports missing several doses of Metformin and has a blood glucose of 600 mg/dL.
Can you give insulin intravenously?
A.)Regular insulin cannot be given intravenously; therefore, the nurse needs to clarify the doctor's order.