What does an elevated ST segment indicate?
The "ST-segment" refers to a part of the test that shows the heart's activity in a wave pattern. When a person has the most severe type of heart attack, this segment will appear abnormally elevated, instead of flat. This indicates a total blockage.
What does an elevated ST segment Mean on an ECG?
What does an elevated ST segment mean on an ECG? The ST Segment represents the interval between ventricular depolarization and repolarization. The most important cause of ST segment abnormality (elevation or depression) is myocardial ischaemia or infarction. Click to see full answer.
What is a depressed ST segment?
ST depression refers to a finding on an electrocardiogram, wherein the trace in the ST segment is abnormally low below the baseline. Simply so, why does ST segment depression occur? ST segment depression occurs because when the ventricle is at rest and therefore repolarized, the depolarized ischemic subendocardium generates electrical currents ...
What is the normal ST segment?
The normal ST segment is usually isoelectric (i.e., flat on the baseline, neither positive nor negative), but it may be slightly elevated or depressed normally (usually by less than 1 mm). Some pathologic conditions such as myocardial infarction (MI) produce characteristic abnormal deviations of the ST segment.

What is a normal ST segment measurement?
The typical ST segment duration is usually around 0.08 sec (80 ms). It should be essentially level with the PR and TP segments. The ST segment represents the isoelectric period when the ventricles are in between depolarization and repolarization.
What indicates ST elevation?
ST-segment elevation usually indicates a total blockage of the involved coronary artery and that the heart muscle is currently dying. Non-STEMI heart attacks usually involve an artery with partial blockage, which usually does not cause as much heart muscle damage.
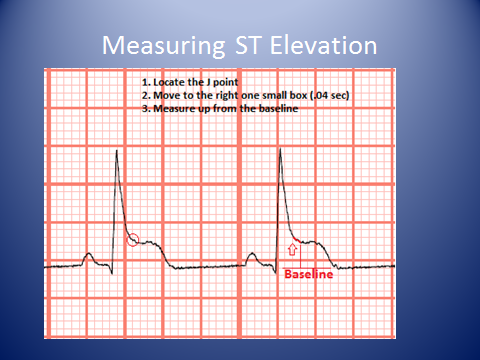
How many mm of ST elevation is significant?
An ST elevation is considered significant if the vertical distance inside the ECG trace and the baseline at a point 0.04 seconds after the J-point is at least 0.1 mV (usually representing 1 mm or 1 small square) in a limb lead or 0.2 mV (2 mm or 2 small squares) in a precordial lead.
How much ST segment elevation is significant?
A threshold value of 0.25 mV for males less than 40 years old should be considered significant ST elevation in leads V and V. For males 40 years old and older, this value is 0.2 mV. For adult females, the value is 0.15 mV.
What causes ST elevation on ECG?
An acute ST-elevation myocardial infarction occurs due to occlusion of one or more coronary arteries, causing transmural myocardial ischemia which in turn results in myocardial injury or necrosis.
What does the ST segment indicate?
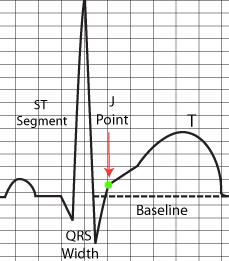
The ST segment is that portion of the ECG cycle from the end of the QRS complex to the beginning of the T wave (Fig. 2-10). It represents the beginning of ventricular repolarization.
What causes ST elevation in all leads?
The most important cause of ST segment elevation is acute Ischemia. Other causes are [4][6]: Early repolarization. Acute pericarditis: ST elevation in all leads except aVR.
What does ST changes mean on ECG?
Nonspecific ST-T-wave changes are very common and may be seen in any lead of the electrocardiogram. The changes may be seen in all or most of the leads (diffuse changes), or they may be present contiguous leads, such as the inferior, lateral, or anterior leads.
What causes ST segment elevation?
Ischemia typically causes ST segment elevations with straight or convex ST segments ( Figure 16, panel A ). The straight ST segment can be either upsloping, horizontal or (rarely) downsloping. Non-ischemic ST segment elevations are typically concave ( Figure 16, panel B ). Concave ST segment elevations are extremely common in any population; e.g ST segment elevation in leads V2–V3 occur in 70% of all men under the age of 70. There is no definite way to rule out myocardial ischemia by judging the appearance of the ST segment, which is why North American and European guidelines assert that the appearance of the ST segment cannot be used to rule out ischemia. ECG changes in ischemia are discussed in detail in section 3 ( Acute & Chronic Myocardial Ischemia & Infarction ) and a specific chapter discusses ST elevation in detail.
Why is ST segment elevation important?
Displacement of the ST segment is of fundamental importance, particularly in acute myocardial ischemia. Because myocardial ischemia affects a limited area and disturbs the cells’ membrane potential (during phase 2), it engenders electrical potential difference in the myocardium.
What is ischemia ST segment?
Ischemic ST depressions display a horizontal or downsloping ST segment (this is a requirement according to North American and European guidelines). The horizontal ST segment depression is most typical of ischemia ( Figure 15 C ). ST segment depressions with upsloping ST segments are rarely caused by myocardial ischemia. However there is one notable exception, when an upsloping ST segment is actually caused by ischemia and the condition is actually alarming. Upsloping ST segment depressions which are accompanied by prominent T-waves in the majority of the precordial leads may be caused by an acute occlusion of the left anterior descending coronary artery (LAD). This constellation – with upsloping ST depression and prominent T-waves in the precordial leads during chest discomfort – is referred to as de Winters sign ( Figure 15 C ).
Why is the J point suboptimal for measuring ST segment deviation?
It must also be noted that the J point is occasionally suboptimal for measuring ST segment deviation. This is explained by the fact that the J point is not always isoelectric; this occurs if there are electrical potential differences in the myocardium by the end of the QRS complex (it typically causes J point depression). The reason for such electrical potential difference is that not all ventricular myocardial cells will finish their action potential simultaneously. Myocardial cells which depolarized at the beginning of the QRS complex will not be in the exact same phase as cells which depolarized during the end of the QRS complex. Due to this it is sometimes recommended that ST segment deviation be measured in the J-60 point, or J-80 point, which is located 60 and 80 milliseconds, respectively, after the J point ( Comprehensive Electrocardiology, MacFarlane et al, Springer, 2010; Chou’s Electrocardiologi, Surawicz, Elsevier 2010 ). At the time of J-60 and J-80, there is minimal chance that there are any electrical potential differences in the myocardium. Current guidelines, however, still recommend the use of the J point for assessing acute ischemia ( Third Universal Definition of Myocardial Infarction, Thygesen et al, Circulation ). A notable exception to this rule is the exercise stress test, in which the J-60 or J-80 is always used (because exercise frequently causes J point depression).
What is secondary ST-T?
Secondary ST-T changes occur when abnormal depolarization causes abnormal repolarization. This is seen in bundle branch blocks (left and right bundle branch block), pre-excitation, ventricular hypertrophy, premature ventricular complexes, pacemaker stimulated beats etc. In each of these conditions the depolarization is abnormal and this affects the repolarization so that it cannot be carried out normally.
What is ST elevation?
In the setting of chest discomfort (or other symptoms suggestive of myocardial ischemia) ST segment elevation is an alarming finding as it indicates that the ischemia is extensive and the risk of malignant arrhythmias is high. However, there are many other causes of ST segment elevations and for obvious reasons one must be able to differentiate these. Figure 16 displays characteristics of ischemic and non-ischemic ST segment elevations. This figure must also be studied in detail.
What causes depression in ST segment?
Digoxin causes generalized ST segment depressions with a curved ST segment (generalized implies that the depression can be seen in most ECG leads). Figure 15 B.
What is ST segment?
The ST segment on an electrocardiogram (ECG) normally represents an electrically neutral area of the complex between ventricular depolarization (QRS complex) and repolarization (T wave). However, it can take on various waveform morphologies that may indicate benign or clinically significant injury or insult to the myocardium. Understanding the differential diagnosis for variations in the ST segment is critical for clinical management as it can influence treatment. This article summarizes ST segment, including how it is defined, measured, and how it varies. This article also examines and summarizes ST-segment morphologies unique to various conditions that present with ST elevation or depression. [1][2][3]
Which reference point is used to determine if the ST segment is elevated or depressed?
The reference point used in determining if the ST segment is elevated or depressed has been an area of dispute. The debate tends to be between using the PQ junction which is the end of the PR segment, or the TP segment. This is because the PQ junction and TP segment may not always be at the same level. While the ventricles depolarize, the atria are repolarizing and can affect the level of the PQ junction. Hence, both the PQ junction and the PR segment cannot be the correct reference point.
What is ST depression?
ST depression occurs when the J point is displaced below baseline. Just like ST elevation, not all ST depression represents myocardial ischemia or an emergent condition. There are multiple conditions associated with ST depression. Some of these include hypokalemia, cardiac ischemia, and medications such as digitalis. T wave changes can also occur with ST depression. Concomitant T waves changes can be seen with ventricular conduction abnormalities and repolarization abnormalities as seen with left bundle branch blocks and LVH. Similar to the thresholds set for clinically significant J-point elevation, there are recommended threshold values for J-point depression. For both males and females the J-point depression threshold values are -0.05 mV in leads V and V and -0.1 mV in all other leads. These values can be used in cases of acute myocardial injury when evaluating for reciprocal ST depression.
What is the J point of a QRS complex?
The junction (J) point is where the QRS complex and ST segment meet. It marks the beginning of the ST segment. Any displacement of the ST segment above or below baseline is often measured at the J point. However, it is not always easy to discern the J point because of various ST-segment morphologies. For instance, diffuse J points can be seen with early repolarization, pericarditis, left ventricular hypertrophy (LVH) with strain, and acute myocardial infarctions (MI). Because it is often difficult to make out the J point and/or the beginning of the T wave, the ST segment is frequently an approximation or evaluated at ST, which is the ST segment at 60 ms after the J point.
What causes ST elevation in MI?
There are many conditions that can mimic the ST elevation seen in acute MI and simply represent normal variations. In fact, early repolarization, LVH, ventricular aneurysm, left bundle branch block, and other conduction defects have been shown to be more common causes of ST elevation than acute MIs.
What is the T wave in myocardial injury?
The T wave should also be considered when assessing the ST segment. In general, myocardial ischemia is represented by ST depression and symmetric T-wave inversion (TWI), while myocardial injury may be indicated by ST elevation with or without T wave changes. T waves should normally be positive in leads I, II, and V-V, and negative in lead aVR. There are many other aspects to consider when evaluating the T wave that are outside the scope of this manuscript. In the remaining sections, we will focus on variations that can be seen with ST elevation and depression and their causes.
What is the threshold for ST elevation?
When evaluating ST elevation clinically, there are threshold limits that have been generally accepted. A threshold value of 0.25 mV for males less than 40 years old should be considered significant ST elevation in leads V and V. For males 40 years old and older, this value is 0.2 mV. For adult females, the value is 0.15 mV. The upper limit of normal J-point elevation in all the other standard leads for males and females is 0.1 mV.
What is ST segment elevation?
ST segment elevation is the key parameter on which the fate of millions of infarct patients are recognised and managed. It is ironical we do not have standardised reference point for measuring the quantum of SR elevation .
What is ST elevation?
ST segment elevation is the key parameter in ACS. Quantifying it becomes important in assessing the efficacy of reperfusion strategies and risk stratification. Fresh ST elevation can represent pericarditis, reinfarction or an early dyskinetic segment . Unless we have proper reference point there is a room for error in this simple parameter.
What is the Sgarbossa criteria?
Sgarbossa criteria (described by Elena Sgarbossa) uses the above principle to objectively assess ST changes in patients with LBBB/paced rhythm, who are suspected of having a STEMI. This criteria was well validated for STEMI.
What is the specificity of a 3 or more score?
Score of 3 or more has a 90% specificity for myocardial infarction. Not sensitive.
What is a STEMI?
A STEMI is a true cardiac emergency, you must recognize a patient with a STEMI and arrange revascularization ASAP.
Is trophonin elevation required for diagnosis?
Notes. Presence of reciprocal changes supports the diagnosis. Troponin elevation is NOT required for diagnosis because STEMI is acute, cTn may be negative if you measure early enough in the course of a STEMI. Memorize the lead orientation!
Is ST elevation a STEMI?
Not all ST elevation is a STEMI!#N#ST segment on an ECG can be elevated for a number of reasons:#N#Any wide QRS (generally > 120ms) or a large-amplitude QRS (such as LVH) produces a repolarization abnormality, which results in the shifting of the ST segment in the opposite direction of the main QRS vector, which is known as “discordant ST change”. (See Figure: “Normal ST Changes in LBBB or Pacing” Below)#N#Wide QRS or large-amplitude QRS patterns that can cause discordant ST changes include: RBBB, LBBB, LVH, RVH, Pacing, Metabolic QRS widening, Pre-excitation, etc.#N#Significant transmural ischemia due to supply/demand mismatch can also produce ST elevation.#N#ALWAYS rule out:#N#Aortic Dissection (can present as Inferior STEMI – look for 1. Tearing Pain, 2. Maximal intensity at onset, 3. involving the back.#N#PE – Calculate the wells score#N#Pericarditis – Pleuritic? positional? pericardial rub? effusion?#N#Mechanical complication: (VSD, papillary muscle rupture) look for new murmur, or sudden flash pulmonary edema.
How long does it take for ST segment elevation to resolve?
Resolution of ST segment elevation is quite variable. It is usually complete within 2 weeks of inferior MI, but it can be delayed further after anterior MI. Persistent ST segment elevation, often seen with a large anterior MI, is indicative of a large area of akinesis, dyskinesis, or ventricular aneurysm. Symmetrical T wave inversions can resolve over weeks to months or can persist for an indefinite period; hence, the age of an MI in the presence of T wave inversions is often termed indeterminate. Q waves usually do not resolve after anterior MI but often disappear after inferior wall MI.
Why is my minipig's ST segment elevated?
ST-segment elevation often occurs with either pericarditis or myocardial infarction; however, in minipigs, it is frequently due to stress and, therefore transient myocardial hypoxia. ST segment depression, depolarization of the QT interval, and slow heart rate are compatible with hypocalcemia; however, this is a very rare occurrence in minipigs.
What is ST elevation in right precordial leads?
Grand et al. [20] found that ST-segment elevation in the right precordial leads is a transient ECG manifestation of moderate to severe acute pulmonary embolism. This phenomenon indicates transmural ischemia in the right ventricle due to hypotension, hypoxemia, right ventricular strain, and catecholamine surge [14,15]. Although ST-segment elevation in the right precordial leads (<2 mm) is not a rare phenomenon, prominent ST-segment elevation (≥0.2 mV) and confined to leads V1–V3 are not seen so frequently. The majority of the patients presenting prominent ST-segment elevation in the right precordial presented with hypotension or cardiogenic shock [6,21–23]. Negative T-waves in the right precordial leads are a frequent ECG manifestation of acute pulmonary embolism and may represent an evolutionary “post-ischemic” stage following ST-segment elevation [14,15]. In case of a new episode of transmural right ventricular ischemia, usually in the context of hypotension or cardiogenic shock, the deep negative T-waves will reduce or disappear or even pseudonormalize and the ST-segment elevation may reappear. Mohsen [21] and Wilson [22] respectively reported similar ECG findings to ours. The “coved” ST-segment elevations in leads V1–V4 [21,22] were identical to type-1 Brugada ECG pattern during cardiogenic shock. At baseline during hemodynamic stability before the Brugada ECG pattern, both cases presented with deep negative T-waves in leads V1–V4.
What is the T wave inversion in the left precordial leads?
T wave inversion combined with ST segment depression in the left lateral precordial leads suggests LVH and is described as a “strain pattern” (see Figure 29-6 ). As previously mentioned, upright T waves in the right precordial leads between the ages of 7 days and 7 years suggest RVH.
How long does it take for a ST segment to resolve after recanalization?
Indeed, failure of ST segment elevation to resolve by more than 50 to 70% within 1 to 2 hours suggests failure of fibrinolysis and should prompt urgent angiography for “rescue angioplasty.”
What causes ST segment depression?
Pseudodepression due to prominent T a waves (atrial repolarization) caused by atrial disease or tachycardia also causes ST segment depression.
Can ST elevation be treated with IV fibrinolytics?
The gold standard of treatment is reperfusion by percutaneous coronary intervention (coronary catheterization) within 90 minutes. In areas where this is not available, IV fibrinolytics should be administered. If these are not available, acetylsalicylic acid and clopidogrel (and perhaps beta blockers) should be administered.
What is the ST segment?
The ST Segment represents the interval between ventricular depolarization and repolarization. The most important cause of ST segment abnormality (elevation or depression) is myocardial ischaemia or infarction.
What causes ST segment abnormalities?
Ventricular pacing (with a pacing wire in the right ventricle) causes ST segment abnormalities identical to that seen in LBBB. There is appropriate discordance, with the ST segment and T wave directed opposite to the main vector of the QRS complex.
What is the telltale sign on the resting ECG?
The tell-tale sign on the resting ECG is the “ Brugada sign ” — ST elevation and partial RBBB in V1-2 with a “ coved ” morphology.
What wave is most apparent in V1-3?
Note the ST elevation in leads with deep S waves — most apparent in V1-3.
Which wave is highly specific for occlusion of the LAD?
Upsloping ST depression in the precordial leads with prominent De Winter T waves is highly specific for occlusion of the LAD.
Which QRS complex produces ST elevation and upright T waves?
This produces ST elevation and upright T waves in leads with a negative QRS complex (dominant S wave), while producing ST depression and T wave inversion in leads with a positive QRS complex (dominant R wave).
Does ST depression indicate ischaemia?
This rate-related ST depression does not necessarily indicate the presence of myocardial ischaemia, provided that it resolves with treatment.
What is the medical diagnosis?
Based on his signs and symptoms and ECG, Mr. M was experiencing an inferolateral ST-elevation myocardial infarction. Recognizing what areas of the heart are affected relies on ST-segment and/or T wave changes in specific leads. Leads II, III, and aVF all view the inferior wall of the left ventricle.
Treatment options
Because Mr. M arrived at the hospital within 12 hours of symptom onset, he was a candidate for reperfusion therapy. 5 His cardiac catheterization revealed that the culprit artery was a totally occluded obtuse marginal (OM) branch of the left circumflex coronary artery.
REFERENCES
1. Prutkin JM. ECG tutorial: basic priniciples of ECG analysis. UpToDate. 2015. www.uptodate.com.
Which wave has the greater ST segment elevation?
Concave ST segment elevations in V1–V3. The deeper the S-wave, the greater the ST segment elevation.
What causes ST elevations?
Figure 8. Perimyocarditis (my ocarditis) causes generalized ST segment elevations. Note that there are no reciprocal ST segment depressions and there are no other ECG changes except from ST elevations. These features are used to differentiate STEMI from pericarditis/myocarditis.
What is the level of the J point in ste-ACS?
In STE-ACS (STEMI) the level of the J point is typically close to the level of the T-wave apex (i.e the height difference between the J point and the apex of the T-wave is typically small). Moreover, ischemic ST segment elevations are typically accompanied by reciprocal ST segment depressions. These ST segment depressions are mirror images of the ST segment elevations, and they are seen in leads with a roughly opposite angle to the leads with ST elevations. Importantly, reciprocal ST segment depressions strongly suggest transmural ischemia. This is also consistent with the vector theory; elevation in one lead should be recorded as depression in a lead with an opposite angle of observation. However, reciprocal ST segment depressions may be missing. There are three explanations as to why reciprocal ST segment depressions may be absent:
How many patients have ST elevations?
80% of patients have localized ST segment elevations (mostly in the chest leads). The morphology of the ST segment elevations cannot be differentiated from those seen in STEMI/STE-ACS.
Which leads have ST segment depressions?
ST segment depressions are seen in leads V5, V6, aVL and I.
Which segment elevations are most pronounced in the chest leads?
The ST segment elevations are concave and most pronounced in the chest leads. T-waves have high amplitude.
Which segment has a concave appearance?
The ST segment has a concave appearance.
What is ST elevation?
ST segment elevation is the key parameter in ACS. Quantifying it becomes important in assessing the efficacy of reperfusion strategies and risk stratification. Fresh ST elevation can represent pericarditis, reinfarction or an early dyskinetic segment . Unless we have proper reference point there is a room for error in this simple parameter.
What is the reference point to measure ST elevation in STEMI ?
ST segment elevation is the key parameter on which the fate of millions of infarct patients are recognised and managed. It is ironical we do not have standardised reference point for measuring the quantum of SR elevation .