Peritoneum
The peritoneum is the serous membrane forming the lining of the abdominal cavity or coelom in amniotes and some invertebrates, such as annelids. It covers most of the intra-abdominal organs, and is composed of a layer of mesothelium supported by a thin layer of connective tissue. This peritoneal lining of the cavity supports many of the abdominal organs and serves as a conduit for their blood ves…
How is peritoneal fluid collected for ascites?
For ascites, a sample of the peritoneal fluid can be taken through a procedure called paracentesis. The sample is collected in sterile tubes to perform different studies, including cytochemical analysis, Gram, BK, culture and biopsy.
What causes fluid in the peritoneum?
A variety of conditions and diseases can cause inflammation of the peritoneum (peritonitis) and/or excessive accumulation of peritoneal fluid (peritoneal effusion or ascites). Peritoneal fluid analysis is a group of tests that evaluate this liquid to determine the cause of the increased fluid.
How is the peritoneal fluid sample prepared for a blood culture?
The rest of the peritoneal fluid sample is deposited in several sterile tubes to perform Gram and BK, cytochemical, etc. The blood culture bottles are incubated for 24-48 hours. The contents of the bottle should be seeded in enriched culture media, such as: blood agar and chocolate agar, where most microorganisms grow.
Can red blood cells be collected from peritoneal fluid?
If the peritoneal fluid is normal, on centrifugation a small pellet of red blood cells will collect, leaving fluid with a normal appearance.19 It is also possible to insert the needle into the spleen, resulting in the collection of a sample with a PCV similar to blood.

How is peritoneal fluid generated?
Peritoneal fluid is produced by transudation from submesothelial vessels across the peritoneal membrane.
How is peritoneal fluid drained?
Having a tube to drain the fluid (paracentesis) Your doctor can put a small tube into the abdomen to drain off the fluid. This reduces the swelling and makes you feel more comfortable. It's called abdominal paracentesis (pronounced para-sen-tee-sis) or an ascitic tap (pronounced ass-it-ic tap).
How do you get peritoneal fluid for culture?
A sample of peritoneal fluid is needed. This sample is obtained using a procedure called an abdominal tap (paracentesis). A sample of fluid is sent to the laboratory for Gram stain and culture. The sample is checked to see if bacteria grows.
What is the difference between ascitic fluid and peritoneal fluid?
The peritoneal cavity normally contains approximately 50–75 mls of fluid that serves to lubricate the tissues that line the abdominal wall and viscera. The term ascites is reserved to denote an abnormal accumulation of this fluid. Ascites is traditionally divided into transudate or exudate based on the protein content.
Is it painful to have ascites drained?
A paracentesis, or an abdominal tap, is a procedure that removes ascites (build-up of fluid) from your abdomen (belly). The fluid buildup can be painful.
How do doctors remove fluid from your body?
Treatment options may include: Diuretics — medicines that help you get rid of extra fluid. Dialysis — a treatment that filters your blood through a machine. Paracentesis — a procedure that uses a small tube to drain fluid from your abdomen.
What Colour is peritoneal fluid?
Under normal conditions, peritoneal fluid is clear to pale yellow. Bloody ascites is a characteristic of benign or malignant tumors, hemorrhagic pancreatitis, or perforated ulcer,23 whereas clear or straw colored ascites is often associated with cirrhosis.
Where is peritoneal fluid found?
A liquid that is made in the abdominal cavity to lubricate the surface of the tissue that lines the abdominal wall and pelvic cavity and covers most of the organs in the abdomen.
What is peritoneal collection?
A peritoneal culture is a procedure where peritoneal fluid is withdrawn with a needle from the peritoneal cavity. The peritoneal cavity is the space between the two membranes lining the abdominal cavity. The test is done to determine the cause of ascites, fluid accumulation in the peritoneal space.
What does peritoneal fluid look like?
Physical characteristics – the normal appearance of a peritoneal fluid sample is usually straw-colored and clear. Abnormal appearances may give clues to conditions or diseases present and may include: Yellow with liver disease, milky from obstruction of the lymphatic system, and greenish from bile.
Can you feel ascites fluid?
Ascites is a common symptom of cirrhosis, which is scarring on the liver. As fluid accumulates in the abdomen, a person can feel bloated and uncomfortable. The fluid can also press on the lungs, causing shortness of breath.
What are the two types of ascites?
There are two different types of ascites: uncomplicated and refractory ascites. Uncomplicated ascites is the most common type and responds well to treatment; refractory ascites, on the other hand, is less common and very difficult to treat, leading to a high mortality rate.
What happens after ascites is drained?
Sometimes, ascites builds up again over the following weeks and months after an ascitic drainage. Your doctor or nurse might recommend starting or continuing diuretic (water) tablets to try to help the fluid stay away for longer. Sometimes people need to have another ascitic drainage.
What happens when ascites is not drained?
Ascites can lead to: Abdominal problems: The fluid buildup may lead to pain, discomfort and difficulty breathing. These symptoms can interfere with your ability to eat, walk and do daily activities. Infection: The fluids can become infected, called spontaneous bacterial peritonitis.
How long does it take to drain fluid from abdomen?
Draining the fluid It usually takes between 5 and 15 minutes. When the fluid stops draining you remove the bottle and put a cap over the end of the tube. You also put a clean dressing on.
How many times can you have ascites drained?
The frequency of these visits will depend on the participant's ascites-related symptoms, but work in ascites due to malignancy [12, 27] indicates that two to three visits each week are most commonly required, with approximately 1–2 L of ascites being drained each time.
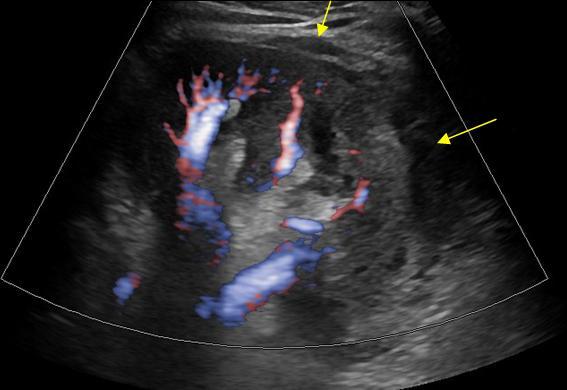
How much fluid is detected in an ultrasound?
Ultrasonography detects as little as 10 mL of fluid. It is of help in assessing patency and flow pattern of portal or hepatic veins and in guiding paracentesis ( Table 81-3 ). Peritoneal fluid is seen in the pelvic cul-de-sac in normal females in all phases of the menstrual cycle. Features that differentiate simple from complicated ascites on imaging studies are shown in Table 81-4 and illustrated in Figure 81-1 . The findings of simple ascites does not exclude infection or tumor. Gallbladder wall thickening is seen in 82% of cases of benign ascites, whereas only 5% of malignant ascites show this finding. Ascites may cause artifacts as a result of reflection of the ultrasonic sound waves at the liver/fluid interface. Pericolonic epiploic appendages may simulate peritoneal metastases.
How much ascites can be detected in a syringe?
Can detect as little as 10 mL of ascites
How to tell if you have ascites?
Plain films are insensitive to ascites until at least 500 mL of fluid has accumulated. Indirect and nonspecific signs are abdominal haziness, bulging of the flanks, indistinct psoas margin, and increased separation of bowel loops. More specific signs include separation of lateral liver contour from the thoracoabdominal wall (Hellmer’s sign), separation of the ascending and descending colon from the properitoneal fat line, and symmetric density on either side of the urinary bladder (the “Mickey Mouse” sign).
What is the normal blood count for hemorrhagic ascites?
Persons with hemorrhagic ascites have a red blood cell count greater than 50,000/mm 3 . The normal red blood cell count of peritoneal fluid is less than 1000/mm 3 . There are several causes of hemorrhagic ascites. Bloody ascites occurs in approximately 5% of patients with cirrhosis.
What percentage of cirrhotic patients have chylous ascites?
Approximately 0.5% to 1% of cirrhotic patients with ascites have chylous instead of serous fluid. Trauma, surgery, or radiotherapy to the abdomen may damage lymphatic channels and lead to chylous ascites.
What is the triglyceride level of paracentesis?
Paracentesis typically shows a cloudy milky aspirate. Triglyceride content of more than 0.1 g/L is diagnostic of chylous ascites. When the cause of chylous ascites is unclear, computed tomography (CT) of the abdomen and pelvis may be useful to evaluate for lymphadenopathy.
What is the classification of ascites?
The term ascites does not specify the type of fluid accumulated within the peritoneal cavity. Ascites may be further classified as in Table 81-2 into infected, chylous, hemorrhagic, and neoplastic fluid.
How to collect peritoneal fluid?
Peritoneal fluid can be collected by clipping and aseptically preparing the most dependent part of the abdomen, on or slightly to the right of midline to avoid the spleen, and inserting an 18-gauge needle. Alternatively, following local anesthesia, a small incision can be made using a No. 15 scalpel blade and inserting a teat cannula. Care must be taken during the collection of fluid to avoid enterocentesis, particularly in horses with distended viscera, or to avoid amniocentesis in the pregnant mare. Where fluid is not easily obtained, abdominal ultrasonography can be performed to identify an area of fluid accumulation for collection. The abdominal fluid should be collected in a plain tube for the measurement of protein concentration and in an ethylenediaminetetraacetic acid (EDTA) tube for a cell count and hematology.
How is peritoneal fluid produced?
Peritoneal fluid is produced by transudation from submesothelial vessels across the peritoneal membrane. The amount of fluid is normally small (less than 50 mL in humans) and contains neutrophils, mononuclear cells, eosinophils, macrophages, lymphocytes, desquamated mesothelial cells, and an average of 3.0 g/mL of protein.
What factors are considered to be important in peritoneal fluid?
Clinical biochemistry may be performed on peritoneal fluid to determine other factors, including fibrinogen, lactate, phosphate, glucose, and pH. A high peritoneal lactate has been shown to be a more sensitive indicator of a strangulating obstruction of the intestine than plasma lactate. 15 In those horses with suspected septic peritonitis, the serum and peritoneal fluid glucose levels can be compared. A difference of greater than 50 mg/dL between the serum and peritoneal fluid glucose level, a low peritoneal fluid glucose level (less than 30 mg/dL), and pH of less than 7.3 are indicators of septic peritonitis.20
How many peritoneal cavities are there in birds?
No single potential coelomic pocket exists in birds. Rather, there are five peritoneal cavities—intestinal, right and left ventral hepatic, and right and left dorsal hepatic.
Why should abdominocentesis not be performed in the field?
Practice Tip: If physical examination reveals other findings consistent with a surgical lesion and referral for surgery is considered, abdominocentesis should not be performed in the field because of the risk to the patient and the examiner.
Where is the second site of a peritoneal stent?
The second site is located just above the udder on the right side under the fold of the flank. The site is clipped and prepared for an aseptic procedure. A tail-jack is used for restraint and an 18-gauge, 1½ needle is inserted through the skin and slowly advanced into the peritoneal cavity.
Where are ascites located?
Fluid that accumulates with disease of the female reproductive tract (e.g., egg yolk peritonitis) is generally located in the intestinal peritoneal cavity. View chapter Purchase book. Read full chapter.
Composition
Normal peritoneal fluid is a transudate. It is characterized by a low protein concentration, glucose similar to that of plasma, few leukocytes, no fibrin clots and red blood cells are scarce or absent.
Features
The peritoneal fluid is located in the peritoneal cavity and is delimited between the visceral peritoneal membrane and the parietal peritoneal membrane.
Where is it produced?
The peritoneal membrane lines the abdominal cavity. This has a visceral and a parietal leaf.
Transudate
Transudate is simply the accumulation of fluid, without inflammation and / or infection. That is, there are no significant changes in its composition. There is also no involvement of the peritoneum. Example of ascites with a characteristic of transudate: cardiac ascites, ascites due to nephrotic syndrome and ascites due to cirrhosis.
Exudate
In the exudates there is not only accumulation of fluid, but also other factors that drastically modify the composition of the peritoneal fluid participate.
What is it studied for?
Peritoneal fluid must be studied to determine the etiology of excess fluid in the peritoneal cavity. Sampling is done through a procedure called paracentesis.
Sampling
20-50 ml of sample are taken depending on the number of analyzes indicated. 10 ml should be inoculated in a blood culture bottle for aerobic microorganisms, and 10 ml in a blood culture bottle for anaerobes.
Why does fluid collect in the anterior bowel?
Fluid may collect anteriorly, as a result of the capillary effect of the narrow space between bowel loops and viscera. In a study of patients with ascites from liver disease, 92% had ascites around the liver, 77% in the pelvis, 69% in the paracolic gutters, and 63% in Morison’s pouch.
How long does it take for peripancreatic fluid to clear?
Virtually all patients with clinically significant pancreatitis have peripancreatic fluid collections, most of which resolve within 6 weeks (see Chapter 96 ). These collections most often occur in the lesser sac and anterior pararenal space. Fluid accumulation in the greater peritoneal sac usually occurs in the setting of severe pancreatitis “burning” the peritoneum, in trauma, or after surgical resection. The cause of pancreatic ascites in all cases is disruption of the pancreatic duct. Endoscopic retrograde pancreatography is diagnostic in these cases. Pancreatic ascites should be part of the differential diagnosis of every patient with chronic ascites who has a history of pancreatitis, alcoholism, or abdominal trauma.
What is a paracentesis?
Diagnostic paracentesis is indicated for any patient who develops ascites for the first time and for patients with chronic ascites who develop fever, encephalopathy, or abdominal pain. Paracentesis for small volumes should be performed under sonographic guidance with an 18- or 20-gauge, plastic-sheathed catheter to avoid injury to the liver, spleen, or gut. With massive ascites, a blind tap can be performed 2 to 3 cm beneath the umbilicus in the midline to reduce the chance of bleeding along the linea alba or at a left-sided McBurney point to avoid injuring an enlarged liver or spleen. Fluid should be analyzed for protein, lactate dehydrogenase, amylase, blood cell count with differential, bacteriologic and cytologic tests, pH, and triglycerides.
What causes ascites in the peritoneum?
The causes of ascites are protean and are listed in Box 110-1 . The imaging features that can help differentiate the various causes are listed in Table 110-1 . Although ascites may merely reflect generalized third-space fluid loss in conditions such as congestive heart failure, chronic renal disease, and massive fluid overload, it is more commonly related to intra-abdominal factors that produce peritoneal fluid more rapidly than it can be absorbed. Cirrhosis and neoplasm are the two most common causes of ascites in the Western world. Tuberculosis and cirrhosis are the predominant causes worldwide.
What is ascites in a patient?
Ascites is the pathologic accumulation of fluid in the peritoneal cavity. It is a common clinical finding that can be associated with a large number of diseases. In some disorders, peritoneal fluid represents a complication or late manifestation of disease, whereas in others, it is the first clinical expression of the disease process. For this reason, early detection and characterization of ascites and other peritoneal fluid collections are important.
Why do ascites occur?
Although ascites may merely reflect generalized third-space fluid loss in conditions such as congestive heart failure, chronic renal disease, and massive fluid overload, it is more commonly related to intra-abdominal factors that produce peritoneal fluid more rapidly than it can be absorbed.
How to tell if you have ascites?
Physical examination reveals abdominal distention , with bulging flanks that are dull to percussion or a fluid wave. As little as 300 to 400 mL of fluid can be demonstrated by placing the patient on hands and knees and producing a dull sound by percussion over the dependent abdomen (i.e., the puddle sign). Umbilical hernias, penile or scrotal edema, and pleural effusion are indirect signs of ascites. Flank dullness is the most sensitive sign, and a fluid wave is the most specific sign of ascites on physical examination.
Why is peritoneal lavage used?
Diagnostic peritoneal lavage is used in unstable patients who have suffered severe physical trauma (unstable means unconscious with abnormal heart rate, blood pressure, and respiratory rate). It is an emergency diagnostic procedure that is preferred over the CT scan in these patients because a delay encountered while performing ...
What makes you unfit for peritoneal lavage?
The conditions that make you unfit for diagnostic peritoneal lavage include: Prior abdominal surgery. Abdominal-wall infections. Coagulopathy (problems in blood clotting) Morbid obesity (having a body mass index [ BMI] of 40 or higher) Last six months of pregnancy.
What to do if there is no blood in the abdomen?
If little or no blood is detected, the doctor will perform a lavage (washing) of the abdominal cavity with a normal saline solution. A small sample of the abdominal fluid will be collected and sent to the laboratory for investigation.
Is peritoneal lavage a bedside procedure?
Being a bedside procedure, diagnostic peritoneal lavage is feasible in patients whose life is at stake— where every minute counts to save a life.
