What is a health insurance claim form?
Health insurance companies distribute Health Insurance Claim Forms to inform the patient of the original payment from the health care provider, the services the insurance company has already paid for, and any remaining balance the patient needs to pay.
What is a medical claim?
What is a medical claim? A medical claim is a bill that healthcare providers submit to a patient’s insurance provider. This bill contains unique medical codes detailing the care administered during a patient visit. The medical codes describe any service that a provider used to render care, including:
What happens after the health insurance claim form has been sent?
Once the health insurance claim form has been sent, the patient waits for any updates from the health insurance company.
What information is included in a medical claim file?
In a medical claims file, this information is in two parts: the claim header and the claim detail. The claim header summarizes the most essential information in the claim. This includes confidential patient information like date of birth, gender, and zip code.
How are healthcare claims sent?
Claims transmission In most cases, claims are first transmitted to a clearinghouse. The clearinghouse reviews and reformats medical claims before sending them to the payor. In some cases, healthcare providers send medical claims directly to a payor.
In what format are health care claims sent quizlet?
Most health care claims are submitted electronically, not on paper. Claim that is accepted by a health plan for adjudication. HIPAA-mandated electronic transaction for claims. The electronic HIPAA claim form, or the 837P claim, is based on the CMS-1500 claim, which is a paper claim form.
Is CMS-1500 paper or electronic?
The Form CMS-1500 is the standard paper claim form to bill Medicare Fee-For-Service (FFS) Contractors when a paper claim is allowed.
What two claim forms are the most common in healthcare?
The two most common claim forms are the CMS-1500 and the UB-04. The UB-04 (CMS 1450) is a claim form used by hospitals, nursing facilities, in-patient, and other facility providers.
What is the most common type of electronic claim formatting used in the United States?
The 837P is the National Standard Format for electronic claims submission by physicians, which replaces the paper CMS-1500 form.
Which of the following is an electronic claim format?
An 837 file is an electronic file that contains patient claim information. This file is submitted to an insurance company or to a clearinghouse instead of printing and mailing a paper claim.
What is the difference between HCFA 1500 and CMS 1500?
The HCFA 1500 claim form, also known as CMS-1500, enables medical physicians to submit health insurance claims for reimbursement from various government insurance plans including Medicare, Medicaid and Tricare.
What is the difference between CMS 1500 and ub04 forms?
But healthcare professionals or physicians use this form to get their payments done on time. So, CMS 1500 is used only by the physicians and not hospitals. Whereas UB-04 or CMS 1450 form is used by hospitals with 81 field locators to enter all the required details like HCPCS codes, NPI, Tax ID, etc.
Can I print my own CMS 1500 forms?
In SimplePractice, you can generate CMS 1500 claim forms to submit electronically through the system, or download and print to submit outside the system.
What is a ub04 document?
The UB-04 uniform medical billing form is the standard claim form that any institutional provider can use for the billing of inpatient or outpatient medical and mental health claims. It is a paper claim form printed with red ink on white standard paper.
What is the claim submission process?
The claim submission is defined as the process of determining the amount of reimbursement that the healthcare provider will receive after the insurance firm clears all the dues. If you submit clean claims, it means the claim spends minimum time in accounts receivable on the payer's side, resulting in faster payments.
What is a HCFA?
Health Care Financing Administration, the agency that administers the Medicare, Medicaid, and Child Health Insurance programs.
What is known as the standard format used by healthcare professionals?
CMS-1500 form. Standard insurance form used by all government and most commercial insurance payers. paper form. EOB.
What is a CMS-1500 form quizlet?
CMS-1500. Claim form used to submit paper claims fo services and procedures rendered by physicians and other health care professional on an outpatient basis. Continuity of care. Coordinating treatment and health services between patients' health care providers.
Who uses the paper CMS-1500 form quizlet?
Standard paper claim form used by health care proffesional and suppliers to bill insurance carriers for servises provided to patients.
What is the standard claim form used for billing in medical offices?
The most common claim form used in the medical office is the: a. CMS-1450.
What information does a medical claims file contain?
Every medical claims file contains details specific to each patient and patient encounter. In a medical claims file, this information is in two parts: the claim header and the claim detail.
What is claim detail?
The claim detail includes information about secondary diagnoses or procedures administered during an inpatient hospital stay. Each new claim detail, or service record, contains the following information:
What does the medical billing process look like?
These steps trace the entire claims journey from the moment a patient checks in at a healthcare facility, to the moment they receive a bill from their insurance provider.
What is the first step in the medical billing process?
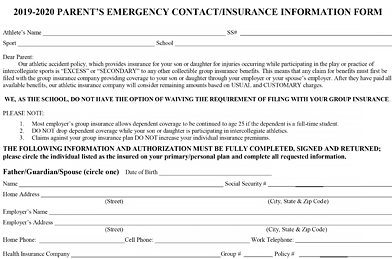
Patient registration is the very first step in the medical billing process. Registration occurs when a patient gives their provider personal details and insurance information.
Why are medical claims important?
All-payer claims contain detailed diagnosis and procedure information for any billable patient visit. Healthcare organizations can use this claims information to: Trace referral patterns. Improve population health.
Why do providers use medical codes?
Care providers use these codes to describe which medical diagnoses, procedures , prescriptions, and supplies they administered and why. The specificity of medical codes also helps providers describe the patient’s condition.
What is medical coding?
Medical coding is a critical step that occurs after care has been administered. Care providers transcribe their notes and other clinical documentation into standardized medical codes. Some of the most common medical coding systems include:
What Is a Health Care Claim?
A health care claim is a type of invoice with a detailed descriptions of the services and treatments rendered by the patient. This invoice is produced by the patient’s health care provider and is sent to the patient’s chosen health insurance company. Once the insurance company receives the invoice, they process it in correspondence to the patient’s formulated health care plan.
What is the purpose of health insurance claim forms?
Health insurance companies distribute Health Insurance Claim Forms to inform the patient of the original payment from the health care provider, the services the insurance company has already paid for, and any remaining balance the patient needs to pay.
What happens when a patient reviews a claim?
Once the patient reviews their claim form, they contact their health insurance company that they filed a claim form and will send it to them for an assessment of benefits. Once the health insurance claim form has been sent, the patient waits for any updates from the health insurance company.
Why is it important to submit documents to health insurance?
Submitting the right documents can make the whole process smoother and more systematic. Receiving benefits for health services can ease a patient’s financial situation and give them less stress. To receive said benefits, the patient must make a health insurance claim.
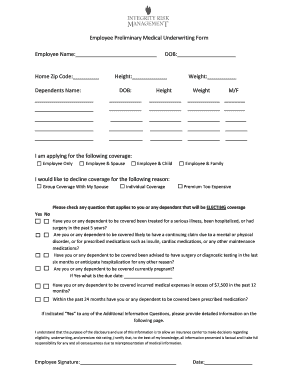
How to collect medical bills?
Patients first collect and organize receipts of their medical bills which they can obtain from their doctor. These receipts encompass the medical services and treatments you have rendered or acquired. The next step involves completing a claim form. A claim form would ask for the patient’s personal information, insurance details, description of the condition, information on the doctor, and any prior payments.
Do you need to fill out a health claim form?
The usual process of health insurance would require the health provider to fill in a patient’s Health Care Claim Forms in order for the patient to receive benefits. There is another aspect of healthcare that can further aid those in need called continuing healthcare.