
Precautions
Atropine is commonly classified as an anticholinergic or antiparasympathetic (parasympatholytic) drug. More precisely, however, it is termed an antimuscarinic agent since it antagonizes the muscarine-like actions of acetylcholine and other choline esters.
Is atropine an antiparasympathetic drug?
Atropine may be used alone or with other medications. Atropine belongs to a class of drugs called Anticholinergic, Antispasmodic Agents. What are the possible side effects of Atropine?
Can atropine be taken with other medications?
Drugs that activate muscarinic receptors in the peripheral nervous system are called parasympathomimetic drugs because they mimic the effects of acetylcholine on the parasympathetic nervous system. An example of a parasympathomimetic drug is pilocarpine, which is a nonspecific muscarinic agonist.
What is a parasympathomimetic drug?
Mechanism of action Atropine binds to and inhibit muscarinic acetylcholine receptors, producing a wide range of anticholinergic effects.
What is the mechanism of atropine action?
See more

What is an example of parasympathomimetic drugs?
Parasympathomimetic medications are available in a variety of different formulations. For example, topical preparations of carbachol and pilocarpine are available for ophthalmic use in the treatment of glaucoma and the induction of miosis during surgical procedures.
What class of drug does atropine belong?
Atropine belongs to a class of drugs called Anticholinergic, Antispasmodic Agents.
Why is atropine a parasympatholytic?
This occurs because atropine is a competitive, reversible antagonist of the muscarinic acetylcholine receptors (acetylcholine being the main neurotransmitter used by the parasympathetic nervous system).
Are cholinergic drugs Parasympathomimetic?
A parasympathomimetic drug, sometimes called a cholinomimetic drug or cholinergic receptor stimulating agent, is a substance that stimulates the parasympathetic nervous system (PSNS). These chemicals are also called cholinergic drugs because acetylcholine (ACh) is the neurotransmitter used by the PSNS.
What is atropine also called?
C17H23NO3. Synonyms. ATROPINE. dl-Hyoscyamine. Tropine tropate.
What is the nature of atropine?
Atropine is a muscarinic cholinergic blocking agent. It competitively blocks parasympathetic, postganglionic nerve endings from the action of acetylcholine and other muscarinic agonists. Atropinic drugs have little effect at nicotinic receptor sites.
Is atropine sympathetic or parasympathetic?
Atropine is a clinically relevant anticholinergic drug, which blocks inhibitory effects of the parasympathetic neurotransmitter acetylcholine on heart rate leading to tachycardia.
What is the mechanism of action of atropine?
Mechanism of Action: Atropine inhibits the muscarinic actions of acetylcholine on structures innervated by postganglionic cholinergic nerves, and on smooth muscles, which respond to endogenous acetylcholine but are not so innervated.
What is the difference between parasympatholytic and Parasympathomimetic?
Drugs that stimulate the parasympathetic nervous system are called parasympathomimetics or cholinergics. Drugs that inhibit the parasympathetic system are called parasympatholytics or anticholinergics.
What are parasympatholytic drugs?
Parasympatholytics are drugs that oppose the effects of the parasympathetic nervous system through anticholinergic action – i.e., they prevent ACh from acting as a neurotransmitter at muscarinic receptors.
Which of the following is a parasympathomimetic agent?
Pilocarpine is a parasympathomimetic drug isolated from Pilocarpus jaborandi. It is used in ophthalmic solutions as an antiglaucoma–miotic agent.
Is atropine an anticholinergic?
Atropine acts as a competitive, reversible antagonist of muscarinic receptors: an anticholinergic drug.
Is atropine a beta blocker?
The first-line symptomatic treatment is administration of atropine and volume-expanding fluids to treat bradycardia and hypotension, respectively. However atropine is often unsuccessful in reversing beta-blocker-induced bradycardia and repeated doses can provoke atropine poisoning.
What family is atropine?
Atropine is found in many members of the Solanaceae family. The most commonly found sources are Atropa belladonna, Datura inoxia, D. metel, and D. stramonium.
What is the drug atropine used for?
Ophthalmic atropine is used before eye examinations to dilate (open) the pupil, the black part of the eye through which you see. It is also used to relieve pain caused by swelling and inflammation of the eye.
What kind of receptor blocker is atropine?
Atropine, which is on the WHO List of Essential Medicines, is a non-selective muscarinic receptor inhibitor used to treat acute sinus node dysfunction associated with bradycardia, complete atrioventricular block, and organophosphate and beta-blocker poisoning.
What is atropine used for?
Atropine is a prescription medicine used to treat the symptoms of low heart rate ( bradycardia ), reduce salivation and bronchial secretions before surgery or as an antidote for overdose of cholinergic drugs or mushroom poisoning. Atropine may be used alone or with other medications.
How to report atropine side effects?
These are not all the possible side effects of Atropine. For more information, ask your doctor or pharmacist. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088 .
How many autoinjectors are there for atropine?
Three (3) Atropine autoinjectors should be available for use in each patient at risk for nerve agent or organophosphate insecticide poisoning; one (1) for mild symptoms plus two (2) more for severe symptoms [see Dosage Information ].
How much atropine is in a single dose?
Each single-dose prefilled autoinjector provides a 1.67 mg dose of atropine base (equivalent to 2 mg atropine sulfate) in a self-contained unit designed for self or caregiver administration.
How is atropine absorbed?
Atropine is well absorbed after intramuscular administration. Atropine is distributed throughout the various body tissues and fluids. Much of the drug is metabolized by enzymatic hydrolysis, particularly in the liver; from 13 to 50% is excreted unchanged in the urine. Atropine has been reported to be excreted in human milk [see Use In Specific Populations ]. Atropine readily crosses the placental barrier and enters the fetal circulation.
How long does it take for atropine to take effect?
Wait 10 to 15 minutes for Atropine to take effect. If, after 10 to 15 minutes , the patient does not develop any of the severe symptoms listed in Table 1, no additional Atropine injections are recommended. If possible, a person other than the patient should administer the second and third 2 mg Atropine autoinjectors.
What is the best treatment for atropine overdose?
Ice bags, alcohol sponges, or a hypothermia blanket may be required to reduce fever, especially in pediatric patients. Catheterization may be necessary if urinary retention occurs. Since atropine elimination takes place through the kidney, urinary output must be maintained and increased if possible; however, dialysis has not been shown to be helpful in overdose situations. Intravenous fluids may be indicated. Because of atropine-induced photophobia, the room should be darkened.
How do parasympathomimetic drugs work?
These drugs work by mimicking or modifying the effects of acetylcholine (ACh), the primary neurotransmitter of the parasympathetic nervous system. Parasympathomimetic medications are classified into two main categories based on whether they are direct agonists or indirect agonists of ACh. Direct agonists directly bind and activate muscarinic ACh receptors, while indirect agonists increase synaptic levels of ACh by inhibiting the enzyme acetylcholinesterase. Listed below are the major indications for various parasympathomimetic drugs:
What are the effects of parasympathomimetic agents?
Toxicity associated with parasympathomimetic agents is the result of cholinergic excess. Muscarinic effects of cholinergic toxidrome include diarrhea, urination, miosis, bronchospasm, bradycardia, emesis, lacrimation, sweating, and salivation (commonly remembered using the mnemonic “DUMBBELSS”). In the case of overdosage of direct-acting agents, parenteral administration of atropine, a muscarinic antagonist, is used to reverse symptoms via competitive inhibition. Cholinergic toxicity can result from the ingestion of some varieties of mushrooms containing muscarine, particularly those in the genera Inocybeand Clitocybe. [12]
How does indirect acting agent affect parasympathomimetic effects?
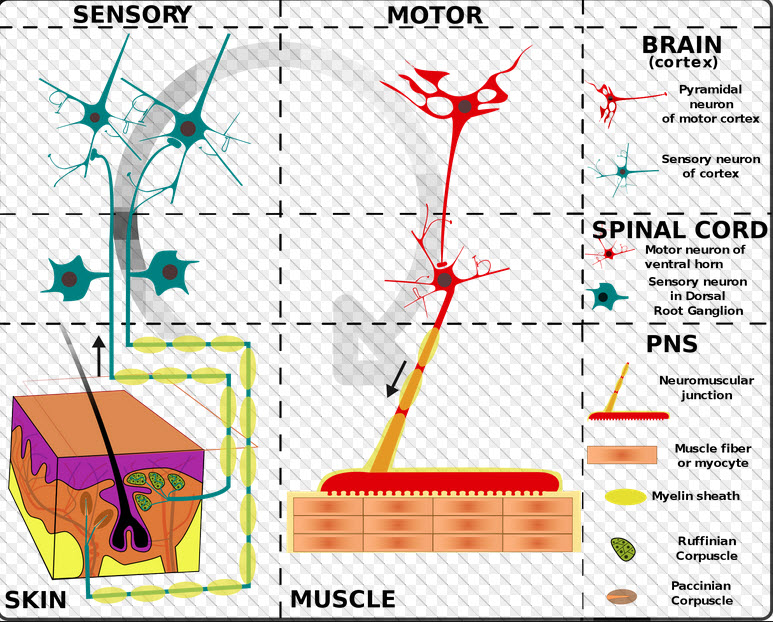
The parasympathomimetic effects of indirect-acting agents are mediated by their inhibitory effect on the hydrolysis of endogenous ACh at cholinergic synapses by acetylcholinesterase. Increased synaptic concentrations of ACh result in prolonged stimulation of cholinergic receptors throughout the central and peripheral nervous systems. [10]
What is the name of the drug that activates the parasympathetic nervous system?
Parasympathomimetics are a class of medications that activate the parasympathetic nervous system by mimicking or modifying the effects of acetylcholine. These drugs include muscarinic receptor agonists (direct-acting parasympathomimetics) and acetylcholinesterase inhibitors (indirect-acting parasympathomimetics ). This activity reviews the indications, contraindications, activity, adverse events, and other key elements of parasympathomimet ic therapy in the clinical setting pertinent to interprofessional team members managing the care of patients receiving these medications.
Why should health care providers monitor parasympathomimetic medications?
Health care providers should monitor patients taking parasympathomimetic medications to ensure that treatment achieves the intended therapeutic effect. Providers must also observe patients closely for possible adverse effects. Overdosage may result in a cholinergic crisis due to the overstimulation of ACh receptors, which can potentially be life-threatening.
Where are muscarinic ACh receptors found?
The five subtypes of muscarinic ACh receptors have varying distributions throughout the central nervous system and periphery. For example, M1 receptors are mainly found in cortical regions of the brain, autonomic ganglia, glands (gastric and salivary), and enteric nerves. M2 receptors are predominantly expressed in cardiac and smooth muscle. M3 receptors are abundant in exocrine glands, smooth muscle, and vascular endothelium. [9]
What is edrophonium used for?
Edrophonium: Historically used in the diagnosis of myasthenia gravis[4]
Where does atropine come from?
Atropine occurs naturally in a number of plants of the nightshade family, including deadly nightshade (belladonna), Jimson weed, and mandrake. It was first isolated in 1833, and is on the World Health Organization's List of Essential Medicines. It is available as a generic medication.
What is the function of atropine?
In general, atropine counters the "rest and digest" activity of glands regulated by the parasympathetic nervous system. This occurs because atropine is a competitive, reversible antagonist of the muscarinic acetylcholine receptors ( acetylcholine being the main neurotransmitter used by the parasympathetic nervous system).
How does atropine affect bradycardia?
One proposed mechanism for atropine's paradoxical bradycardia effect at low doses involves blockade of inhibitory presynaptic muscarinic autoreceptors, thereby blocking a system that inhibits the parasympathetic response. Atropine is incapacitating at doses of 10 to 20 mg per person.
What are the symptoms of atropine overdose?
These associations reflect the specific changes of warm, dry skin from decreased sweating, blurry vision, decreased lacrimation, vasodilation, and central nervous system effects on muscarinic receptors, type 4 and 5. This set of symptoms is known as anticholinergic toxidrome, and may also be caused by other drugs with anticholinergic effects, such as hyoscine hydrobromide (scopolamine), diphenhydramine, phenothiazine antipsychotics and benztropine.
How does pralidoxime help with organophosphate poisoning?
Pralidoxime (2-PAM) can be effective against organophosphate poisoning because it can re-cleave this phosphorylation. Atropine can be used to reduce the effect of the poisoning by blocking muscarinic acetylcholine receptors, which would otherwise be overstimulated, by excessive acetylcholine accumulation.
Why is atropine used in intubation?
Atropine has also been used in an effort to prevent a low heart rate during intubation of children ; however, evidence does not support this use.
How long does atropine last?
Eye drops are also available which are used to treat uveitis and early amblyopia. The intravenous solution usually begins working within a minute and lasts half an hour to an hour. Large doses may be required to treat some poisonings.
What is atropine used for?
Atropine is a muscarinic antagonist used to treat poisoning by muscarinic agents, including organophosphates and other drugs.
What class is tropane alkaloids?
This compound belongs to the class of organic compounds known as tropane alkaloids. These are organic compounds containing the nitrogenous bicyclic alkaloid parent N-Methyl-8-azabicyclo [3.2.1]octane.
What is the role of muscarinic acetylcholine receptor?
The muscarinic acetylcholine receptor mediates various cellular responses, including inhibition of adenylate cyclase, breakdown of phosphoinositides and modulation of potassium channels through the...
What happens after binding acetylcholine?
After binding acetylcholine, the AChR responds by an extensive change in conformation that affects all subunits and leads to opening of an ion-conducting channel across the plasma membrane permeabl...
What is the glycine receptor?
The glycine receptor is a neurotransmitter-gated ion channel. Binding of glycine to its receptor increases the chloride conductance and thus produces hyperpolarization (inhibition of neuronal firing).
How much of a drug is destroyed by enzymatic hydrolysis?
Much of the drug is destroyed by enzymatic hydrolysis, particularly in the liver; from 13 to 50% is excreted unchanged in the urine.
How many drugs can you compare with our drug interaction checker?
Easily compare up to 40 drugs with our drug interaction checker.
What is a parasympathomimetic drug?
A parasympathomimetic drug, sometimes called a cholinomimetic drug or cholinergic receptor stimulating agent, is a substance that stimulates the parasympathetic nervous system (PSNS).
What is indirect acting parasympathomimetic?
Indirect acting parasympathomimetic substances may be either reversible cholinesterase inhibitors, irreversible cholinesterase inhibitors or substances that promote ACh release or anti-adrenergics. The latter inhibits the antagonistic system, the sympathetic nervous system .
What is the name of the drug that stimulates the parasympathetic nervous system?
A parasympathomimetic drug, sometimes called a cholinomimetic drug or cholinergic receptor stimulating agent, is a substance that stimulates the parasympathetic nervous system (PSNS). These chemicals are also called cholinergic drugs because acetylcholine (ACh) is the neurotransmitter used by the PSNS. Chemicals in this family can act either directly by stimulating the nicotinic or muscarinic receptors (thus mimicking acetylcholine), or indirectly by inhibiting cholinesterase, promoting acetylcholine release, or other mechanisms.
What is the name of the drug that inhibits the muscarinic receptor?
ISBN 978-0-7020-5554-6. Parasympathomimetics are a group of drugs that act either by directly stimulating the muscarinic receptor, for example pilocarpine, or by inhibiting the enzyme acetylcholinesterase, which hydrolyses the acetylcholine in the synapse.
Overview
This medication is used before eye examinations (such as refraction) and to treat certain eye conditions (such as uveitis).
May Treat: Cholinesterase inhibitors toxicity · Cycloplegia · Irritable bowel syndrome · Muscarine toxicity · Mydriasis and more
Brand Names: Isopto Atropine · AtroPen · Atropine Care · Atropisol · Atreza and more
Drug Class: GI Antispasmodic - Belladonna Alkaloids · Muscarinic Receptor Antagonists (Anticholinergic) · Ophthalmic - Anticholinergics
Availability: Prescription sometimes needed
Pregnancy: Consult a doctor before using
May Treat: Cholinesterase inhibitors toxicity · Cycloplegia · Irritable bowel syndrome · Muscarine toxicity · Mydriasis and more
Brand Names: Isopto Atropine · AtroPen · Atropine Care · Atropisol · Atreza and more
Drug Class: GI Antispasmodic - Belladonna Alkaloids · Muscarinic Receptor Antagonists (Anticholinergic) · Ophthalmic - Anticholinergics
Availability: Prescription sometimes needed
Pregnancy: Consult a doctor before using
Lactation: Consult a doctor before using
Driving: May cause drowsiness or dizziness. Use caution
Medical uses
Side effects
Atropine is a tropane alkaloid and anticholinergic medication used to treat certain types of nerve agent and pesticide poisonings as well as some types of slow heart rate, and to decrease saliva production during surgery. It is typically given intravenously or by injection into a muscle. Eye drops are also available which are used to treat uveitis and early amblyopia. The intravenous solution usually begin…
Contraindications
Topical atropine is used as a cycloplegic, to temporarily paralyze the accommodation reflex, and as a mydriatic, to dilate the pupils. Atropine degrades slowly, typically wearing off in 7 to 14 days, so it is generally used as a therapeutic mydriatic, whereas tropicamide (a shorter-acting cholinergic antagonist) or phenylephrine (an α-adrenergic agonist) is preferred as an aid to
Chemistry
Adverse reactions to atropine include ventricular fibrillation, supraventricular or ventricular tachycardia, dizziness, nausea, blurred vision, loss of balance, dilated pupils, photophobia, dry mouth and potentially extreme confusion, deliriant hallucinations, and excitation especially among the elderly. These latter effects are because atropine is able to cross the blood–brain barrier. Because of the hallucinogenic properties, some have used the drug recreationally, though this is …
Pharmacology
It is generally contraindicated in people with glaucoma, pyloric stenosis, or prostatic hypertrophy, except in doses ordinarily used for preanesthesia.
History
Atropine, a tropane alkaloid, is an enantiomeric mixture of d-hyoscyamine and l-hyoscyamine, with most of its physiological effects due to l-hyoscyamine. Its pharmacological effects are due to binding to muscarinic acetylcholine receptors. It is an antimuscarinic agent. Significant levels are achieved in the CNS within 30 minutes to 1 hour and disappears rapidly from the blood with a half-life of 2 hours. About 60% is excreted unchanged in the urine, most of the rest appears in urine …
Natural sources
In general, atropine counters the "rest and digest" activity of glands regulated by the parasympathetic nervous system. This occurs because atropine is a competitive, reversible antagonist of the muscarinic acetylcholine receptors (acetylcholine being the main neurotransmitter used by the parasympathetic nervous system).
Atropine is a competitive antagonist of the muscarinic acetylcholine receptor types M1, M2, M3, M4 a…