
Precautions
One of the most popular treatments is a prescription blood thinner called Lovenox, also known as enoxaparin. If you are at high risk for blood clots in pregnancy, or if you are currently experiencing a blood clot during pregnancy, you are probably wondering if Lovenox is a good choice for you.
Is Lovenox (enoxaparin) safe during pregnancy?
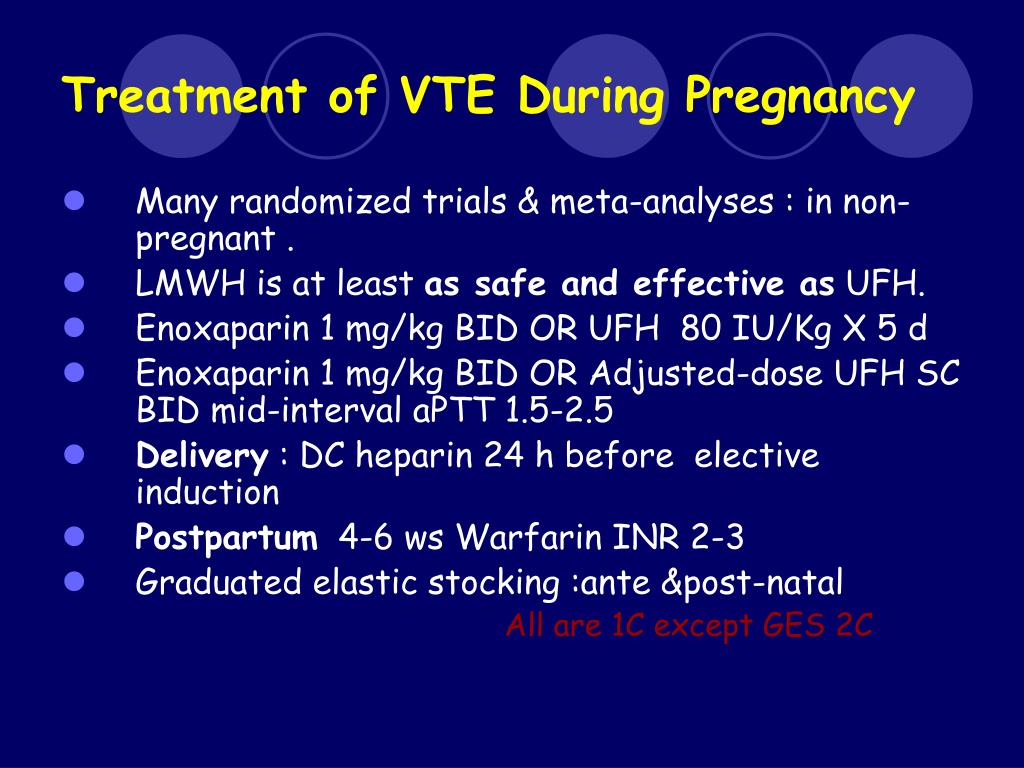
Enoxaparin has been increasingly used over the past 20 years in pregnant women at risk of thrombosis and pregnancy complications. The main indications are prophylaxis of venous thromboembolism and prevention of pregnancy loss in thrombophilic women.
What is enoxaparin used to treat?
The main indications are prophylaxis of venous thromboembolism and prevention of pregnancy loss … Enoxaparin use in pregnancy: state of the art Womens Health (Lond). 2007 Jan;3(1):9-14.doi: 10.2217/17455057.3.1.9. Author Benjamin Brenner 1 Affiliation
What are the indications for enoxaparin in pregnancy?
Conclusion: Literature on the efficacy and safety of enoxaparin for thromboembolism and thromboprophylaxis remains scanty, and therefore efficacy was not assessed; in terms of safety, when including other indications for enoxaparin in pregnancy, we found that enoxaparin was associated with significantly lower complications than aspirin.
Is enoxaparin effective and safe for thromboembolism and thromboprophylaxis?
Can you use enoxaparin during pregnancy?
Enoxaparin does not cross the placenta and is safe for the fetus. Maternal side effects are uncommon and include mild localized allergic reactions in 2% and increased bleeding in 2%, which is dose dependent.
When should enoxaparin be stopped during pregnancy?
Women should be advised to stop their LMWH when contractions begin. For a planned delivery, most guidelines recommend stopping enoxaparin within 24 hours, and this is especially important if an epidural is desired.
Where do you inject enoxaparin when pregnant?
The best places for you to inject into are: • The U-shape area around your belly button. It is safe to inject LMWH into the abdomen while pregnant. The upper outer side of the thigh. The upper outer part of the buttock.
What blood thinners are safe during pregnancy?
Standard or “unfractionated” heparin and low-molecular-weight heparin (LMWH) are safe in pregnancy because they do not cross the placenta and, therefore, do not enter the blood stream of unborn babies.
Is enoxaparin high risk?
Extra care is needed because enoxaparin is a high-alert medicine. High-alert medicines have been proven to be safe and effective. But these medicines can cause serious injury if a mistake happens while taking them. This means that it is very important for you to know about this medicine and take it exactly as directed.
What is the major side effect of enoxaparin?
The most common adverse reactions were bleeding, anemia, thrombocytopenia, elevation of serum aminotransferase, diarrhea, and nausea.
Can enoxaparin cause miscarriage?
During the study, 30.4% of women enrolled in the enoxaparin group vs 23.7% in the placebo group had a subsequent miscarriage (relative risk, 1.28; 95% CI, 0.85-1.93). Most of the losses (84.3%) occurred before 10 weeks' gestation.
What time should enoxaparin be given?
Timing of dose Enoxaparin should be administered at approximately the same time each day. 6pm has been traditional, but if anti-factor Xa levels are required (very infrequently required and normally only on the advice of a specialist), 8am is preferred as blood samples are required 4 hours post dose.
What time should I inject enoxaparin?
Adults—40 milligrams (mg) injected under the skin once a day for 7 to 10 days. The first dose should be given 2 hours before the surgery.
Can blood thinning injections harm baby?
The injections commonly used are a type of heparin. Heparin injections are safe to use in pregnancy and cause no harm to your developing baby. The heparin injections do not pass into breastmilk, so you are able to breastfeed whilst on the heparin injections.
Can blood thinners hurt baby?
While oral anticoagulants, or blood thinners, such as warfarin, dabigatran, rivaroxaban and apixaban are most commonly prescribed, they are not considered safe for unborn babies. Women who take blood thinners should contact their doctor immediately upon finding out they are pregnant.
Do blood thinners affect baby?
Blood thinning is generally safe but there are a number of important precautions to take in pregnancy. One of the blood thinning medications (Warfarin) can sometimes cause problems in the baby – it is important to stop warfarin before getting pregnant or at least to stop warfarin as soon as you become pregnant.
How long should enoxaparin be given?
Most people need shots for 5 to 10 days, but in some cases it can be longer. Your doctor will tell you how long you need to have the shots. Enoxaparin is used to: Treat deep vein thrombosis (DVT), which is a blood clot in the legs, pelvis, or arms.
How long do you give enoxaparin?
Enoxaparin comes as an injection in a syringe to be injected just under the skin (subcutaneously) but not into your muscle. It is usually given twice a day. You will probably begin using the drug while you are in the hospital and then use it for a total of 10 to 14 days.
What happens when you stop enoxaparin?
If you stop taking the drug suddenly or don't take it at all: You'll have a higher risk for a blood clot. This could lead to serious problems, such as a stroke or death. Take this drug on the schedule set by your doctor. Don't stop taking it without speaking with your doctor first.
How long can you be on enoxaparin?
The usual duration of administration is 7 to 10 days [see Clinical Studies]. A dose of Lovenox of 40 mg once a day subcutaneously may be considered for hip replacement surgery for up to 3 weeks.
Is heparin an anticoagulant?
Low-molecular-weight heparin is the anticoagulant of choice in pregnancy. Enoxaparin has been increasingly used over the past 20 years in pregnant women at risk of thrombosis and pregnancy complications. The main indications are prophylaxis of venous thromboembolism and prevention of pregnancy loss in thrombophilic women.
Is enoxaparin safe for pregnancy?
Enoxaparin use in pregnancy: state of the art. Low-molecular-weight heparin is the anticoagulant of choice in pregnancy. Enoxaparin has been increasingly used over the past 20 years in pregnant women at risk of thrombosis and pregnancy complications.
Does enoxaparin cross the placenta?
Enoxaparin does not cross the placenta and is safe for the fetus. Maternal side effects are uncommon and include mild localized allergic reactions in 2% and increased bleeding in 2%, which is dose dependent. Heparin-induced thrombocytopenia is very rare and bone resorption is not clinically relevant. The mechanisms of action of enoxaparin in ...
What is enoxaparin used for?
It has approval for the following clinical conditions - acute coronary syndromes, deep venous thrombosis (DVT) treatment and prophylaxis, treatment for pulmonary embolism (PE), venous thromboembolism (VTE) treatment and prophylaxis in a variety of scenarios, percutaneous coronary intervention (PCI), and periprocedural anticoagulation, among others. This activity will highlight the mechanism of action, adverse event profile, pharmacology, monitoring, and relevant interactions of enoxaparin, pertinent for members of the interprofessional team in the treatment of patients with conditions where this agent is indicated.
What is the management of enoxaparin?
The management of bleeding complica tions of enoxaparin is challenging, and it requires the inclusion of interprofessional health care team members such as the physician, nurses, laboratory technician, and the pharmacist. The management should not be delayed, and intervention should take place as soon as possible. A blood bank should be contacted for possible need of an urgent transfusion. As discussed above, protamine sulfate is the drug of choice in this situation. A conservative approach is necessary for the consideration of acute bleeding. Anticoagulation should be stopped with the reversal of anticoagulation. Fluid resuscitation is also important if the patient is hemodynamically unstable.
What is the most common complication of enoxaparin?
As with most anticoagulants, bleeding is the most major complication with low molecular weight heparin-like enoxaparin. The incidence rate is reported to be less than 3%. Given the subcutaneous form of administration of LMWH, there is a high risk of minor bruising at the injection site. The subcutaneous injection has a bioavailability of around 100%. In the event of significant bleeding, protamine sulfate can be used to reverse the anticoagulant effects of LMWH partially. Protamine neutralizes about 60% of LMWH anticoagulant activity. For LMWH administered within the previous 8 hours, the recommended dose is 1mg protamine sulfate per 1mg of enoxaparin or 100 anti-factor-Xa units of dalteparin. [7]
What is the lowest molecular weight heparin?
There are two low molecular heparins available in the market: dalteparin and enoxaparin. Enoxaparin is low molecular weight heparin (LMWH) and was first approved for medical use in 1993 and is derived from heparin. It has approval for the following clinical conditions[1][2][3]:
How much creatinine clearance is required for enoxaparin?
Enoxaparin dose requires adjustment with a creatinine clearance of less than 30 mL/minute. [8]
How much enoxaparin should I take?
One mg of enoxaparin is equal to 100 units of anti-Xa activity. The usual dose is 1 milligram/kilogram every 12 hours. However, dosing can be variable depending on the clinical situation. For example, in acute coronary syndrome, 1 milligram/kg every 12 hours is indicated if the patient is less than 75 years of age. But 0.75 milligrams/kg every 12 hr is the dose if the patient is 75 years of age or older.
What is the molecular weight of enoxaparin?
Enoxaparin is a type of low molecular weight heparin (LMWHs) with a mean molecular weight of 4000 to 5000. It has an immediate onset of action when given in the intravenous form. It binds to and potentiates antithrombin III, a serine protease inhibitor, to form a complex that irreversibly inactivates factor Xa.[4] Enoxaparin has less activity against factor IIa (thrombin) compared to unfractionated heparin.
What Is Lovenox?
The ability of our blood to clot is important and necessary (for example, after you get a cut or injury, your blood clots so that you don’t continue bleeding profusely). However, if your blood clots too much, blood clots can form in the legs and other extremities and make their way to the lungs, causing a condition called pulmonary embolism (PE), which can be life-threatening if not treated promptly.
What are the side effects of Lovenox?
The most common (but generally rare) side effects of Lovenox include: 3 1 Bleeding 2 Anemia 3 Thrombocytopenia (low platelet count) 4 Elevated levels of serum aminotransferase 5 Nausea and diarrhea 6 Ecchymosis (skin discoloration as a result of bleeding under the skin) 7 Edema 8 Fever 9 Shortness of breath 10 Disorientation 11 Pain at the injection site
What are the conditions that increase the risk of blood clots during pregnancy?
Conditions that may increase your risk of blood clots during pregnancy include: Family or personal history of blood clots. History of a blood clotting disorder. A C-section delivery. Periods of prolonged immobility, including bed rest during pregnancy or after delivery. Complications during pregnancy or childbirth.
What happens if you have too much blood clots?
However, if your blood clots too much, blood clots can form in the legs and other extremities and make their way to the lungs, causing a condition called pulmonary embolism (PE), which can be life-threatening if not treated promptly.
Why do pregnant women have more clots?
Pregnant people are more prone to blood clots during pregnancy because a pregnant person’s blood naturally clots more easily to prevent blood loss during and after giving birth. Additionally, blood may not flow as easily to the legs during pregnancy as a result of the growing fetus putting pressure on pelvic blood vessels. 4.
Where is Lovenox given?
Lovenox may be given via IV when you are in the hospital, but it’s most frequently given by injection. Lovenox is injected into the fatty layer just below the skin, and is most often injected into the stomach or abdominal area.
What are the risks of blood clots during pregnancy?
1 If untreated, blood clotting during pregnancy can lead to serious conditions like pulmonary embolism (PE), which can be fatal. 2.
A Word About Antibiotics
So many patients call asking for antibiotics for a cold,usually when theyve had symptoms for several days. There are a few times whenantibiotics are appropriate, for instance, strep throat or sinus infectionscaused by bacteria. But antibiotics simply dont work against viruses thatcause the common cold.
Variations In Risk Factors
A report by Philipp et al indicated that risk factors for thrombosis in women who have had adverse pregnancy outcomes differ significantly between white and black women. In the study, involving 409 patients who had adverse outcomes in pregnancy, the investigators determined the following:
After Your Baby Is Born
After your baby is born, you will need to take heparin for at least 6 weeks.
Anticoagulation In Pregnant Patients With Valvular Heart Disease
Warfarin is more efficacious than unfractionated heparin for thromboembolic prophylaxis of pregnant women with mechanical valves.
Blood Thinners During Pregnancy And Breastfeeding
Generic Name: LMW Heparins FDA Drug Category: B Summary Recommendations: LMW blood thinners like Heparin are prescribed for the treatment of blood clotting disorders in women with a history of blood clots and to prevent other pregnancy complications.
Is There Anything Else I Can Do
It is important that the heparin injections are monitored when you are pregnant so your blood thinning is at the right level. This will make sure your blood is not too thin which can cause bleeding or not thin enough which can cause blood clots.
Prevent Pregnancy Blood Clots
By virtue of being pregnant or in the postpartum period, expectant women and new moms are at an increased risk of DVT, so you cant eliminate the risk completely. But there are some steps you can take to reduce your risk of blood clots.
How long does it take to inject Lovenox?
I’m a dental hygienist and am used to giving shots in the mouth, and while they were teaching us how to give shots, they said, the slower the better. They recommended taking 1 minute to inject the whole thing. Which is probably pretty long for lovenox, but I have found it to be the least painful. Good luck!!
What is a group leader?
A Group Leader is a volunteer community member that is nominated by peers to have admin privileges of their assigned groups. They are a friendly voice in the group and have a direct line to What to Expect moderator staff. Group Leaders are chosen to uphold the core values of the brand and help remove content that violates the community guidelines.
Is Lovenox painful?
Dec 7, 2020 at 4:53 PM. I have the same meds as you! Lovenox can be painful, but it is better to be as comfortable and relaxed as you can, pinch your skin, insert the needle slowly and inject very slowly. This helps to avoid so much burning.
What are the views expressed in community?
The views expressed in community are solely the opinions of participants, and do not reflect those of What to Expect. Learn more about our guidelines
Is Lovenox good for a pregnancies?
There is a group on here call Lovenox Ladies that is super helpful and supportive. Many have had successful pregnancies on Lovenox after multiple losses. I am on it for previous blood clot, but you get used to the shots and I recommend icing it before and after because it helps with bruising and stinging. You've got this!
Is it scary to get injections?
the injections can be scary id just recommend a glass of water and to be seated when you do it! good luck!
