Does Enterobacter aerogenes have any medical significance?
Two of its well- known species, Enterobacter aerogenes and E. cloacae have taken on clinical significance as opportunistic bacteria and have emerged as nosocomial pathogens from intensive care patients pathogenic, especially to those who are on mechanical ventilation ( Mezzatesta et al., 2012 ).
Is Enteroccus faecalis Gram negative or Gram positive?
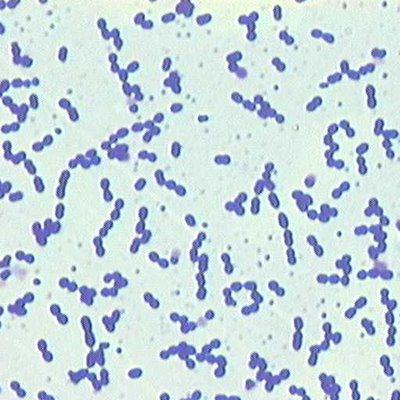
Enterococcus faecalis is a Gram-positive facultative anaerobe that naturally inhabits the human gastrointestinal tract. This organism belongs to the lactic acid bacteria (LAB) group, which are identified by a low G+C content and are able to grow in a broad range of temperatures (1).
Is Entamoeba Gram positive?
Entamoeba histolytica cysts were detected in both dysenteric and control groups. [ajtmh.org] ] a large epidemic of dysentery in Japan. [22, 37] The bacterium was also referred to more generally as the dysentery bacillus (the term “bacillus” referring to a genus of Gram - positive [about-shigella.com] Show info.
Are endotoxins only Gram negative?
Endotoxins in food are a result of bacteria called Gram-negative. type of bacteria that have a thin wall and an outer membrane, such as celiacs. A. coli and Salmonella enterica, respectively)). The opposite way around is that toxins are produced by both gram-positive and gram-negative bacteria.
See more

Is Enterobacter Gram positive or negative?
Gram-negativeMembers of the Enterobacteriaceae are bacilli (rod-shaped), facultative anaerobes, fermenting sugars to produce lactic acid and various other end products. They are typically 1-5 μm in length and they have Gram-negative stains.
Is Enterococcus aerogenes Gram positive or negative?
gram-negative bacteriaEnterobacter aerogenes and Enterobacter cloacae are gram-negative bacteria that belong to the family Enterobacteriaceae. They can be both aerobic and anaerobic.
How do you identify Enterobacter aerogenes?
The next method used was a Urea test. This test consisted of stirring the bacterial growth into a tube of phenol red and urea to test for the presence of acid. After incubation the broth was still a yellow color, giving a negative result. This confirmed that Enterobacter aerogenes was the gram-negative bacterium.
What antibiotics treat Enterobacter aerogenes?
The antimicrobials most commonly indicated in Enterobacter infections include carbapenems, fourth-generation cephalosporins, aminoglycosides, fluoroquinolones, and TMP-SMZ.
Is Enterobacter aerogenes positive?
Klebsiella aerogenes, previously known as Enterobacter aerogenes, is a Gram-negative, oxidase negative, catalase positive, citrate positive, indole negative, rod-shaped bacterium. The bacterium is approximately 1-3 microns in length, and is capable of motility via peritrichous flagella.
What are the characteristics of Enterobacter aerogenes?
Enterbacter aerogenes is a gram-negative, rod shaped bacterium that contains flagella surrounding it's outer surface. E. aerogenes as well as others in its genus are known to be resistant to antibiotics, especially E.
Where is Enterobacter aerogenes commonly found?
E. aerogenes is generally found in the human gastrointestinal tract and does not generally cause disease in healthy individuals. It has been found to live in various wastes, hygienic chemicals, and soil.
What is another name for Enterobacter aerogenes?
Klebsiella aerogenesEnterobacter aerogenes was recently renamed Klebsiella aerogenes.
How is Enterobacter aerogenes different from E coli?
The ability to produce a large amount of acid is used to differentiate E. coli from Enterobacter aerogenes. Both organisms initially produce organic acids.
What disease does Enterobacter aerogenes cause?
Enterobacter species are responsible for causing many nosocomial infections, and less commonly community-acquired infections, including urinary tract infections (UTI), respiratory infections, soft tissue infections, osteomyelitis, and endocarditis, among many others.
How do you get Enterobacter infection?
The source of infection may be endogenous (via colonization of the skin, gastrointestinal tract, or urinary tract) or exogenous, resulting from the ubiquitous nature of Enterobacter species.
How common is Enterobacter aerogenes?
Enterobacter is the eighth most common pathogen in healthcare-associated infections in the United States (Hidron et al. 2008) and constitutes 2.9 % of healthcare-associated bloodstream infections in Korea (Son et al.
Is enterococci gram neg?
Enterococci are ubiquitous gram-positive cocci, calatase-negative, non-spore-forming, facultative anaerobic organisms, that belong to the Lancefield group D streptococci.
Is enterococcus a Gram-negative rod?
Enterococci are gram-positive, facultatively anaerobic cocci that form short- to medium-length chains. In the 1930s, Lancefield devised a serologic typing system that classified enterococci as group D streptococci, along with some organisms (eg, Streptococcus gallolyticus, formerly S.
Is Gram-negative bacilli a UTI?
Gram-negative rods (GNR) are the most common pathogens associated with urinary tract infections (UTI). The resistance of these gram-negative rods to various antibiotics is increasing with time. The study aimed to determine the pattern of resistance to antibiotics in GNR causing urinary tract infection in adults.
Is VRE Gram-positive or negative?
In particular, vancomycin-resistant Enterococcus (VRE) is challenging to manage. Enterococci are facultative anaerobic gram-positive cocci that are normally commensal organisms of the human gastrointestinal tract. However, they can cause a variety of infections.
Which Enterobacter aerogenes cause sepsis?
Enterobacter species. Among the Enterobacter aerogenes (i.e., Aerobacter aerogenes) species, Enterobacter cloacae, Enterobacter sakazakii, and Enterobacter hormaechei have caused sepsis and a severe form of necrotizing meningitis in neonates [ 129–134 ]. In 2008, the taxonomy of E. sakazakii was revised, resulting in identification ...
What is the resistance of Enterobacter?
Strains belonging to the genus Enterobacter are notorious for antimicrobial resistance, earning them acronymal notoriety in the ESKAPE mnemonic. 327 E. cloacae, E. aerogenes, and most strains of E. sakazakii are intrinsically resistant to ampicillin and first- and second-generation cephalosporins as a result of an inducible ampC chromosomal β-lactamase that is controlled by both positive and negative regulators. 328 Furthermore, mutants that constitutively produce high levels of β-lactamase, conferring resistance to third-generation cephalosporins, arise at frequencies of 10 −4 to 10 −7, usually as a result of mutations in the regulatory loci, such that resistant mutants are already present in most patients with Enterobacter infections before initiation of therapy. In addition, like other members of the Enterobacteriaceae, Enterobacter spp. may carry plasmids encoding resistance to multiple antimicrobial agents. Therapy for Enterobacter infections must therefore be tailored to individual isolates and based on antimicrobial susceptibility testing. However, clinicians must be aware that emergence of stably derepressed resistant mutants may lead to treatment failure when third-generation cephalosporins are chosen, even if the isolates appear susceptible on initial testing. 329 Therefore, fourth-generation cephalosporins, carbapenems, or other agents may be better choices than other β-lactam antibiotics for serious infections involving high bacterial burden.
What is the most common nosocomial infection in neonates?
Enterobacter septicemia was the most common nosocomial infection in neonates at the Ondokuz Mayis University Hospital in Samsun, Turkey, from 1988-1992 [ 136 ]. Willis and Robinson [ 130] reviewed 17 cases of neonatal meningitis caused by E. sakazakii; cerebral abscess or cyst formation developed in 77% of the infants, and 50% of the infants died. Bonadio and colleagues [ 131] reviewed 30 cases of E. cloacae bacteremia in children, including 10 infants younger than 2 months. The high frequency of multidrug resistance among isolates from patients in the NICUs was attributed to routine extended-spectrum cephalosporin usage [ 137 ]. An outbreak of E. sakazakii in a French NICU in 1994 involved 17 cases including 7 neonates with necrotizing enterocolitis, 1 case of sepsis, and 1 case of meningitis; 8 infants were colonized, but asymptomatic; there were 3 deaths. Four separable pulse types of E. sakazakii were identified, but the deaths were attributable to only one [ 138 ]. In a review of Enterobacter sepsis in 28 neonates from Taiwan, thrombocytopenia (66%) and increased band-form neutrophils (41%) were common laboratory features, with a reported clinical outcome of 11% mortality, 14% meningitis, and 7% brain abscess [ 139 ].
What is the name of the bacterium that is found in human faeces?
Classification. The name Klebsiella aerogenes was originally used for the non-motile, capsulate, gas-producing strains commonly found in human faeces and in water; certain biochemically atypical Klebsiella strains isolated from the respiratory tract of man and animals were designated K. pneumoniae.
How does glycogen contribute to dental caries?
The synthesis and later degradation of glycogen by some oral bacteria may be an important factor in the development of dental caries. Consistent with this postulate are the findings that these organisms are capable of synthesizing glycogen, produce more acid when exogenous carbohydrate is present, and can produce acid in the absence of exogenous carbohydrate, when compared with oral bacteria that are unable to synthesize glycogen. The acid formed from polysaccharide catabolism may be of significance in the development of dental caries. It is formed over a considerable period of time and may consequently be responsible for the lower resting pH observed in dental plaque sampled from individuals with active caries.
What are the sources of Enterobacter infection in neonates?
In addition to the gastrointestinal tracts of hospitalized infants and hands of health care personnel, sources and modes of transmission of Enterobacter infections in the neonate include contaminated infant formula [ 140–143 ] , contaminated total parenteral nutrition fluid [ 144, 145 ] , bladder catheterization devices [ 144 ] , and contaminated saline [ 146 ]. Effective infection control measures require reinforcement of procedures including proper hand hygiene, aseptic technique, isolation protocols, and disinfection of environmental surfaces.
Which bacteria are found in milk?
Coliforms. These belong to the Enterobacteriaceae family that is widespread in the digestive tract of animals. Escherichia coli and Klebsiella aerogenes are also part of this family that often grow rapidly in milk, particularly above 20 °C.
How does Enterobacter aerogenes cause disease?
Pathology. Enterobacter aerogenes causes disease in humans through inadvertent bacteria transfer in hospital settings. A selection of enteric bacteria like E. aerogenes are opportunistic and only infect those who already have suppressed host immunity defenses.
Where are Enterobacter aerogenes found?
Enterobacter are found in the soil, water, dairy products, and in the intestines of animals as well as humans. They are most frequently found in the gastrointestinal tract and are studied in clinical sites in stool samples. The minimum, optimum and maximum pH for E. aerogenes replication is 4.4, 6.0-7.0, and 9.0 (6).
What media is E. aerogenes positive?
Enterobacter aerogenes has been plated on several different medias and have been observed under several types of testing. The results are as follows- E. aerogenes tested negative when treated with/for: Indol, Methyl red, Hydrogen sulfide (by way of TSI), Urease, Arginine dihydrolase, Phenylalanine deaminase, and Dulcitol. E. aerogenes tested positive when treated with/for: Voges-Proskauer, Simmons' citrate, KCN, Motility, Lysine decarboxylase, Ornithine decarboxylase, Gas from glucose, Lactose, Sucrose, Manntiol, Salicin, Adonitol, Inositol, Sorbitol, Arabinose, Raffinose, and Rhamnose. Delayed positive results were obtained from: Gelatin (22°C) and Malonate (11). In other words, E. aerogenes resembles E. cloacae but the leusine decarboxylase test is positive and gelatin liquification is late. E. aerogenes is also, often times confused with Klebsiella aerogenes. However, E. aerogenes is motile and urease negative while K. aerogenes is nonmotile and urease positive (5). In actuality, research shows that "E. aerogenes is more related to Klebsiella aerogenes (47-64%) than it is to E. cloacae (44%) (9).
How does Enterobacter cloacae work?
We found an interesting article on the bacteria Enterobacter cloacae. This article talks about Enterobacter cloacae and how it is resistant to third generation cephalosporins. Cephalosporins are under the class of B-Lactam antibiotics and these type of antibiotics work by inhibiting bacterial cell wall synthesis. B-Lactams covalently binds to and inactivates transpeptidase enzymes (which are responsible for cross-linking the amino acid that form the peptidoglycan layer of the cell wall). Since the the transpeptidase enzyme is now inactivated by the antibiotic, and the cell wall can no longer form crosslinkages, the cell will eventually burst and lyse, thus killing the bacteria. However, bacteria have developed different types of resistance to antibiotics. For example, the enzyme B-lactamase serves to hydrolyze and break the B-Lactam rings of antibiotics and therefore nullifies the antibiotics effects. This article shows that research shows that the B-Lactamase of Enterobacter cloacae play a different role. They do not hydrolyze the B-Lactam rings. Instead Enterobacter cloacae’s resistance to cephalosporins arises from mutation due to constitutive production of B-Lactamases. The article concludes that after many experiments done, the resistance mechanism for Enterobacter cloacae is still yet to be determined but it is a fact that there is no hydrolysis of the B-Lactam ring and that some sort of mutation is causing the prevention of the binding of the drug to the enzyme or that there is some sort of permeation barrier that is responsible for the resistance.
What is aerogenes in bacteria?
E. aerogenes are smaller, rod-shaped cells that are motile and encapsulated compared to others in the same family of Enterobacteriaceae. The complete genomic information (88% is coded) has not been entirely sequenced as of yet, however, there is some research that shows studies on mutations as well as show evidence of replication through plasmids. E. cloacae and E. aerogenes stain samples had no extrachromosomal elements (9). Plasmid analysis remains as one of the most utilized laboratory techniques used, but PFGE, RAPD, ribotyping, enterobacterial repetitive intergenic consensus (ERIC), PCR, and amplified fragment length polymorphism is also used. The replicon name is R751. The bacteria consists of DNA and is circular. Its length is recorded as 53,435 basepairs long and contains no structural RNAs. The G + C content is 64% and no psuedo genes are recorded for E. aerogenes (9).
How to treat E. aerogenes?
Preventative measures can be taken to reduce infection of E. aerogenes by monitoring careful, aseptic surgical techniques (3). Catheters should be removed and venous needles and tubing should be taken out and put in new locations. Treatment for E. aerogenes is difficult due to the highly resistant nature of the species. Enterobacter strains are resistant to penicillins and other cephalosporins because of the production of chromosomal beta-lactamase with cepholosprinase activity. Additionally, many are resistant to tetracycline, chloramphenicol and to streptomycin, as well as other aminoglycosides (such as gentamicin and fluoroquinolones). Most strains may appear to be susceptible to cefotaxime on primary testing, however, they often possess an inducible chromosomal cephalosporinase, allowing for the rapid development of resistance during treatment or therapy (7).
Where can I find Enterobacter cloacae?
Different species of Enterobacter like E. cloacae are known to be found on a number of seeds and plants while E. sakazakii is commonly seen in infants who were given infant milk-based powder formulas (9).
How to diagnose enterobacter infection?
It is recommended that at least two sets of blood cultures be obtained, one aerobic and one anaerobic bottle. MacConkey agar can be used to determine if the specimen is lactose fermenting. Furthermore, indole testing can be performed to differentiate indole negative Klebsiellaand Enterobacterand indole positiveE. Coli.Enterobacterspp are motile, in contrast to Klebsiella, which is not motile.
How many species of Enterobacter are there?
Enterobacteris a genus belonging to the family of Enterobacteriaceae that is associated primarily with healthcare-related infections. There are currently 22 species of Enterobacter. However, not all species are known to cause human disease. Enterobacterspecies are responsible for causing many nosocomial infections, and less commonly community-acquired infections, including urinary tract infections (UTI), respiratory infections, soft tissue infections, osteomyelitis, and endocarditis, among many others. Certain species of this bacterium can be part of the microflora of the mammalian gastrointestinal tract, while other Enterobacterspecies can be present in human skin surfaces, water, certain foods, soil, and sewage.
What is the role of Enterobacter species in urinary tract infections?
This article focuses on the role of the interprofessional team in the evaluation and management of Enterobacter Infections.
What is the treatment for carbapenem resistant Enterobacter?
Possible treatment for carbapenem-resistant Enterobacter (CRE) includes polymyxins, tigecycline, fosfomycin, and carbapenems (used in a double carbapenem regimen).[6] Although it may seem paradoxical, the rationale behind a double carbapenem regimen is that one carbapenem operates as the “sacrificial” medication due to its greater affinity to the carbapenemase, so that the concomitant carbapenem with a lesser affinity can maintain a higher concentration.[7] A combination of antimicrobial agents has been shown to be more effective than monotherapy in cases of CRE in which more serious clinical characteristics are seen, such as septic shock and rapidly progressing disease. [8]
What is the mechanism of resistance in Enterobacterspp?
The presence of beta-lactamases in Enterobacterspp. is the primary mechanism of antimicrobial resistance. Beta lactamases can hydrolyze the beta-lactam ring seen in penicillin and cephalosporins. The presence of this enzyme has contributed to an increase in the number of resistant Enterobacterpathogens. [2]
What are the most common clinical manifestations of enterobacterinfection?
The most common clinical syndromes are bacteremia, lower respiratory tract infections, UTIs, surgical site infections, and intravascular device-associated infections. Less commonly occurring infections are nosocomial meningitis, sinusitis, and osteomyelitis. Enterobacterinfections can have very similar clinical presentations as other facultative anaerobic gram-negative rod bacterial infections, to the point that they can often be indistinguishable.
Can you take cephalosporin with Enterobacter?
First and second-generation cephalosporins are generally not effective against Enterobacterinfections. Although treatment with a third-generation cephalosporin may be effective in some strains of Enterobacter, treatment with third-generation cephalosporins can lead to multiresistant infection.[4] Third-generation cephalosporins are likely to induce or select derepressed Enterobactergenetic variants of AmpC beta-lactamase, leading to the overproduction of the enzyme and developed resistance. The use of third-generation cephalosporins is not recommended in severe Enterobacterinfections due to increased likelihood of resistance, particularly in Enterobacter cloacaeand Enterobacter aerogenes,two of the most clinically relevantEnterobacter species. Other mechanisms of resistance include the addition of transferable AmpC gene from plasmids and a mutation in the AmpR repressor.
What is the genus of Enterobacter?
Enterobacter, (genus Enterobacter), any of a group of rod-shaped bacteriaof the family Enterobacteriaceae. Enterobacterare gram-negative bacteria that are classified as facultative anaerobes, which means that they are able to thrive in both aerobic and anaerobic environments.
Where do enterobacteria live?
Enterobacteris named for the organisms’ predominant natural habitat, the intestines of animals (from Greek enteron, meaning “intestine”). Enterobacterare ubiquitousin nature; their presence in the intestinal tracts of animals results in their wide distribution in soil, water, and sewage. They are also found in plants.
What are some examples of antibiotic resistance?
Resistance of Enterobacterto non-beta-lactam antibiotics, including fluoroquinolones such as ciprofloxacin , involves distinct cellular and genetic mechanisms. Examples of bacteria utilizing such mechanisms include ciprofloxacin-resistant E. aerogenesand multidrug-resistant E. aerogenes, which in many instances is resistant to ciprofloxacin and imipenem. In Enterobacterorganisms resistant to aminoglycosides, resistance has been associated with a bacterial genetic element known as an integron. Integrons contain genesthat confer antibiotic resistancecapabilities and are incorporated into bacterial genomes via genetic recombination. They are efficiently exchanged and disseminatedamong circulating bacterial populations, such as those occurring in nosocomial environments. In E. cloacaeresistance to the aminoglycoside gentamicin has been attributed to the presence of integrons in the organism’s genome.
What is the treatment for enterobacteria?
Traditional approaches to treating Enterobacterinfections involve single-agent antimicrobial therapy, typically with an aminoglycoside, a fluoroquinolone, a cephalosporin, or imipenem. In some instances, however, subpopulations of Enterobacterare capable of producing enzymes known as beta-lactamases, which cleavethe central ring structure responsible for the activity of beta-lactam antibiotics, a group that includes imipenem (a type of carbapenem) and cephalosporins. Repeated exposure to these drugs selects for beta-lactamase-synthesizing Enterobacter, thereby giving rise to drug resistance, including against carbapenems, which were once highly effective against multidrug-resistant organisms. Newer approaches to Enterobacterinfections have adopted combination-therapy regimens employing multiple antibiotics with different core structures, such as an aminoglycoside or a fluoroquinolone in combination with a beta-lactam agent. Despite the promise of this more diversestrategy, however, it has been associated with the selection of multidrug-resistant organisms.
What antibiotics are used for enterobacteria?
Newer approaches to Enterobacterinfections have adopted combination-therapy regimens employing multiple antibiotics with different core structures, such as an aminoglycoside or a fluoroquinolone in combination with a beta-lactam agent.
Which enzymes are responsible for the activity of beta-lactamases?
In some instances, however, subpopulations of Enterobacterare capable of producing enzymes known as beta-lactamases, which cleavethe central ring structure responsible for the activity of beta-lactam antibiotics, a group that includes imipenem (a type of carbapenem) and cephalosporins.
Who is Kara Rogers?
Kara Rogers is the senior editor of biomedical sciences at Encyclopædia Britannica, where she oversees a range of content from medicine and genetics to microorganisms. She joined Britannica in 2006 and...
Which test gave negative results and conformed that the unknown gram positive bacteria was Enterococcus f?
And the rate determining test for gram positive was urea and the nitrate test which gave negative results and conformed that the unknown gram positive bacteria was Enterococcus faecalis. This was too conformed by the instructor that it was the right bacteria found.
How to isolate Gram negative bacteria?
The first procedure carried out was the isolation of the unknown mixtures by carrying out the quadrant steak procedure on an agar medium. Then it was incubated at 37 degree Celsius for 2 days, the result obtained was colonies grown of one kind only, when gram stained found out to be pink color rod shaped microbes, this proofed that it was a gram negative bacteria, but failed to obtain the gram positive colonies to grow on the agar plate. Once the gram negative was obtained, the original sample was re-streaked on agar plate to completely isolate it, once isolated the following test were carried out, to find the gram negative bacteria.
Why was the original sample re-streaked on a mannitol salt agar plate?
In order for the gram positive bacteria to grow, original sample was streaked on a mannitol salt agar plate, because it favors the growth ...
Why is identification of unknown bacteria important?
Identification of an unknown bacterium plays an important role in medical laboratories, in order to figure out the pathogenic bacteria, and also the structure of a bacterium plays a role because specific antibiotics target specific structures of the bacteria in order to destroy it, by using a specific antibiotic. MATERIALS AND METHODS:
Why is it important to know what bacteria cause diseases?
It is very important for the physicians to know what bacteria cause diseases so that they are able to prescribe a narrow spectrum antibiotic, rather than prescribing a broad spectrum antibiotic.
Where is E. aerogenes found?
E.aerogenes is generally found in the human gastrointestinal tract and does not generally cause disease in healthy individuals. It has been found to live in various wastes, soil, water, dairy products and hygienic chemicals.
Can a bacterium be identified as a new species?
Sometimes trying to figure out the identity of an unknown bacterium, can also led to discovery of new species, for example, if test are performed to identify the bacterium, and the bacterium does not match any previous single species test, then it is possible that a new species has been discovered. Identification of an unknown bacterium plays an ...

Classification
Description and Significance
- The Enterobacteriaceae family includes genera of Escherichia, Shilgella, Salmonella, Enterobacter, Klebsiella, Serratia, Proteus, amongst others. The gram-negative bacteria resides in soil, water, dairy products and inhabits a natural flora in the gastrointestinal tract of animals as well as humans. The rod shaped Enterobacteriaceae exists in a variety of sizes; are not spore forming; a…
Genome Structure
- E. aerogenes are smaller, rod-shaped cells that are motile and encapsulated compared to others in the same family of Enterobacteriaceae. The complete genomic information (88% is coded) has not been entirely sequenced as of yet, however, there is some research that shows studies on mutations as well as show evidence of replication through plasmids. E. cloacae and E. aerogene…
Cell Structure and Metabolism
- Enterbacter aerogenes is a gram-negative, rod shaped bacterium that contains flagella surrounding it's outer surface. E. aerogenes as well as others in its genus are known to be resistant to antibiotics, especially E. aerogenes and E. cloacae. Research shows that two clinical strains of E. aerogenesexhibited phenotypes of multiresistance to β-lacta...
Ecology
- Enterobacter are found in the soil, water, dairy products, and in the intestines of animals as well as humans. They are most frequently found in the gastrointestinal tract and are studied in clinical sites in stool samples. The minimum, optimum and maximum pH for E. aerogenesreplication is 4.4, 6.0-7.0, and 9.0 (6). Enterobacter aerogenes has been plated on several different medias an…
Pathology
- Enterobacter aerogenes causes disease in humans through inadvertent bacteria transfer in hospital settings. A selection of enteric bacteria like E. aerogenesare opportunistic and only infect those who already have suppressed host immunity defenses. Infants, the elderly, and those who are in the terminal stages of other disease or are immunosuppressed are prime candidates for s…
Application to Biotechnology
- Studies show that E. aerogenes has an increasing drug resistance rate. High levels of drug resistance in enterobacteria were found in accordance to aminoglycosides and broad-spectrum and fourth generation ceftazidime (>40%) and cefepime (15%). E. aerogenes stains showed production of extended-spectrum β-lactamases (ESBLs). A resistance such as this one often ari…
Current Research
- In a case study used to determine the cause of infections in the aorta, isolation of two strains: S. pneumoniae and E. aerogenes were discovered and extracted from a 72 year old male suffering from epigastric pain, fevers, and chills. The orgin of E. aerogenes is unknown but is thought to be a result from and undiagnosed urinary tract infection or pneumonia. Research prior to this indica…
Other Members of Same Genus
- We found an interesting article on the bacteria Enterobacter cloacae. This article talks about Enterobacter cloacae and how it is resistant to third generation cephalosporins. Cephalosporins are under the class of B-Lactam antibiotics and these type of antibiotics work by inhibiting bacterial cell wall synthesis. B-Lactams covalently binds to and inactivates transpeptidase enzy…
Energy Source
- One of the bi-products of fermentation is hydrogen gas. The ability of Enterobacter aerogenes to produce hydrogen through the fermentation of a variety of sugars, including glucose, galactose, fructose, mannose, mannitol, sucrose, maltose, and lactose, has led scientists to investigate the use of this bacteria’s metabolism as a means of acquiring clean energy. Many bacteria can prod…