Is acetaminophen really safe in pregnancy?
For years, acetaminophen (also called paracetamol) has been considered a safe medication to take for pain relief during pregnancy. Now, researchers warn that the common over-the-counter (OTC) pain reliever may interfere with fetal development, and they are advising pregnant people to be cautious about taking the drug.
Is Combiflam safe in pregnancy?
No, Combiflam is not recommended during pregnancy. It belongs to a class of drugs called - Nonsteroidal Anti-inflammatory Drugs (NSAIDs), which can be very risky for you & your unborn baby. The news of being pregnant brings immense joy and excitement to expecting mothers, but pregnancy comes with its pain & discomfort too.
Is restoralax safe to take during pregnancy?
Is Restoralax safe during pregnancy? Restoralax is considered safe for short-term use during pregnancy. Patients using Restoralax experience faster relief of clinical symptoms and shorter disease duration. Is Restoralax safe during breastfeeding? Caution is recommended. No effects on the infant are expected since systemic exposure to the ...
Can I take labetalol while pregnant?
Labetalol may cause low blood pressure, low blood sugar, slow heartbeats, or breathing problems in a newborn if the mother uses labetalol during pregnancy. Tell your doctor if you are pregnant or plan to become pregnant. Ask a doctor if it is safe to breastfeed while using this medicine. Not approved for use by anyone younger than 18 years old.

How many mg of labetalol is safe during pregnancy?
Hypertension in Pregnancy: An initial dosage of 100 mg twice daily may be increased, if necessary at weekly intervals by 100 mg twice daily.
Will labetalol affect my baby?
Because of the low levels of labetalol in breastmilk, amounts ingested by the infant are small and would not be expected to cause any adverse effects in fullterm breastfed infants. No special precautions are required in most infants.
Why is labetalol safe in pregnancy?
Use of labetalol in pregnancy is common and there is no concern that it causes harm. Labetalol belongs to a family of medicines called beta blockers. Studies have not shown that beta blockers cause birth defects, stillbirth, or preterm birth.
When should a pregnant woman take labetalol?
1 The National Institute for Health and Care Excellence (NICE) recommends labetalol as first-line antihypertensive treatment for non-severe (<160/110 mm Hg) gestational hypertension and pre-eclampsia once blood pressure exceeds 150/100 mm Hg.
What is the safest blood pressure medication during pregnancy?
Methyldopa has been used for decades to treat high blood pressure in pregnancy and it appears to be safe....For the initial treatment of high blood pressure in pregnancy, these are the most commonly used and recommended medications:Labetalol (Normodyne, Trandate)Nifedipine (Procardia, Adalat)Methyldopa (Aldomet)
How quickly does labetalol lower blood pressure?
Labetalol starts to work within 2 hours, but it can take a few days to take full effect.
What are side effects of labetalol?
Side effects of labetalolFeeling sleepy, dizzy or weak. If labetalol makes you feel dizzy or weak, stop what you're doing and sit or lie down until you feel better. ... Headaches. Make sure you rest and drink plenty of fluids. ... Cold fingers or toes. ... Feeling sick or being sick (nausea or vomiting) ... Diarrhoea. ... Stomach pain.
Can labetalol cause fetal growth restriction?
Overall, the available studies do not suggest that gestational labetalol exposure increases the risks of fetal growth restriction or preterm delivery; however, because maternal hypertension is associated with both of these outcomes, analysis is complex.
Does labetalol prevent preeclampsia?
Labetalol, a combined alpha and beta blocker, has been used for many years to safely treat hypertension in preeclamptic women, and is now known to reduce CPP in women with preeclampsia.
What is the first line treatment for hypertension in pregnancy?
Background: Hydralazine, labetalol, and nifedipine are the recommended first-line treatments for severe hypertension in pregnancy.
Can labetalol cross the placenta?
During the final part of pregnancy and parturition these drugs should therefore only be given after weighing the needs of the mother against the risk to the foetus. Labetalol is known to cross the placental barrier and has been found to bind to the eyes of foetal animals.
When should you not take labetalol?
You should not use labetalol if you are allergic to it, or if you have:asthma;"AV block" (2nd or 3rd degree);uncontrolled heart failure;very low blood pressure;slow heartbeats that have caused you to faint; or.if your heart cannot pump blood properly.
Does labetalol affect fetal heart rate?
Conclusion. Decreased frequency of accelerations is seen after exposure to hydralazine or labetalol, but there is no additional effect on other parameters of the fetal heart rate pattern.
Does labetalol cross placenta?
Labetalol Pregnancy Warnings During the final part of pregnancy and parturition these drugs should therefore only be given after weighing the needs of the mother against the risk to the fetus. -This drug crosses the placental barrier and has been found to bind to the eyes of fetal animals.
How long does it take for labetalol to get out of your system?
Labetalol is metabolized by the liver resulting in an inactive glucuronide conjugate. It has an onset of action within 2 to 5 minutes, reaches its peak effects at 5 to 15 minutes, has an elimination half-life of 5.5 hours, and a duration of action up to four hours.
Is Preeclampsia linked to autism?
Therefore, preeclampsia can increase risk for developing autistic disorders [3,19]. According to 2 meta-analyses, obesity is a risk factor for preeclampsia and ASD [25,26]. Therefore, increasing obesity prevalence has paralleled the increase in preeclampsia and ASD.
What is the FDA pregnancy category C?
US FDA pregnancy category C: Animal reproduction studies have shown an adverse effect on the fetus and there are no adequate and well-controlled studies in humans, but potential benefits may warrant use of the drug in pregnant women despite potential risks. AU: Contraindicated during the first trimester of pregnancy.
Can you breastfeed with Labetalol?
Labetalol Breastfeeding Warnings. -The effects in the nursing infant are unknown. Because of the low levels of this drug in breastmilk, amounts ingested by the infant are small and would not be expected to cause any adverse effects in full-term breastfed infants.
Can labetalol be used during pregnancy?
Exposure to labetalol at any stage in pregnancy would not usually be regarded as medical grounds for termination of pregnancy. In pregnancies complicated by maternal hypertension and/or where labetalol has been administered, careful monitoring of fetal growth is advised. Other risk factors may also be present in individual cases which may independently increase the risk of adverse pregnancy outcome. Clinicians are reminded of the importance of considering such factors when performing case-specific risk assessments.
Is lbetalol a beta blocker?
Labetalol is a non-selective beta-blocker with additional alpha adrenoceptor blocking properties. It is licensed for the treatment of mild to severe hypertension, hypertension in pregnancy, and angina pectoris with existing hypertension. NICE guidelines state that where clinically appropriate, labetalol is recommended as first-line antihypertensive treatment in pregnancy.
Can labetalol cause congenital heart defects?
Although single studies have found no association between gestational exposure to labetalol and congenital heart defects or hypospadias, these findings remain to be confirmed. It is noteworthy that while some women with chronic hypertension may be switched to labetalol during early pregnancy, gestational hypertension is, by definition, diagnosed after 20 gestational weeks and its treatment will therefore pose a low risk of structural anomaly.
Does gestational labetalol cause stillbirth?
Overall, the available studies do not suggest that gestational labetalol exposure increases the risks of fetal growth restriction or preterm delivery; however, because maternal hypertension is associated with both of these outcomes, analysis is complex. Very limited data do not raise concern that gestational labetalol exposure increases the risk of stillbirth, but this remains to be confirmed. Data on rates of miscarriage and neurodevelopmental outcomes are too limited to permit a risk assessment.
What is the most commonly used antihypertensive medication for the treatment of hypertension during pregnancy?
Introduction: Labetalol is one of the most commonly used antihypertensive medications for the treatment of hypertension during pregnancy, an increasingly common and leading cause of maternal mortality and morbidity worldwide.
Is lbetalol good for pregnancy?
Labetalol is a reasonable choice for treatment of severe or non-severe hypertension in pregnancy. However, we should continue our search for other therapeutic options.
What is labetalol used for?
1318. Also called as ‘beta-blocker’, labetalol is used for treating high blood pressure. Orally, this is used for long term hypertension management, whereas intravenously, in severe hypertension situations. Labetalol slows the heart rate and improves the blood flow which further decreases the blood pressure. Although it does not cure it but one has ...
Why is a baby stillborn?
Some of the reasons that can be held responsible for this are the genetic factors, mother’s health, age and lifestyle. There have been cases where women taking labetalol experienced stillbirth but at the same time, there are also women who had a safe delivery. It is basically the effect of high blood pressure that causes the risk of stillbirth rather than labetalol. Considering this, it is a little difficult to say whether labetalol can cause stillbirth.
Is labetalol safe during pregnancy?
Uses of labetalol during pregnancy: As a first-line drug, labetalol supersedes all other drugs and is absolutely safe in the first trimester of pregnancy. Causes smooth fall in blood pressure.
Does Labetalol lower blood pressure?
Labetalol slows the heart rate and improves the blood flow which further decreases the blood pressure. Although it does not cure it but one has to remain careful about its side effects as well.
Can labetalol cause a miscarriage?
A lot of women worry about this but there are no evidences if labetalol has caused a miscarriage.
Can you take labetalol while pregnant?
For those who were given treatment for high blood pressure before pregnancy, they are advised to move on from their previous medicine and switch to labetalol. However, you must consult your doctor before taking the medicine as it is vital for you to follow all the precautions for the betterment of your baby and yourself.
Is labetalol safe for a person with a stomach problem?
Although labetalol is considered to be safe and is recommended to only a certain patients. But Some of the side effects that are pretty common are as listed below: Regular dosage of the medicine can lead to an upset stomach. Can lead to tingling scalp or skin. Regular consumption of the medicine can lead to fatigue.
When does labetalol cause birth defects?
Since most of the baby’s internal organs develop within the first 3 months (12 weeks) of pregnancy, any risk of birth defects will be higher at this time. Only a few studies have been conducted to identify if conditions like hypospadias or heart defects are linked to consumption of labetalol during pregnancy. The studies do not show any such link between labetalol and these defects at present. In short, labetalol doesn’t cause any effects to the baby hence given safely
What Is Labetalol?
Labetalol is a drug used for treating high blood pressure. This medication is termed ‘beta-blocker’ – a group of drugs that can be given orally for long-term hypertension management and intravenously in severe hypertensive situations. Lowering blood pressure helps prevent heart attacks, strokes, and kidney problems. It relaxes the blood vessels and slows the heart rate, which results in improved blood flow, thus decreasing blood pressure.
Can labetalol affect the baby?
It is absolutely uncertain whether a labetalol dose in pregnancy can affect the baby after birth. There are some known side-effects of a labetalol dose in pregnancy, like low heart rate , low blood pressure, and low blood sugar. Sometimes, these effects are found in babies who were exposed to labetalol in their mother’s womb. However, a number of studies have suggested that the likelihood of any complication with the baby after birth is not due to the exposure of the baby to labetalol in the mother’s womb. Therefore, mothers who have been taking labetalol during pregnancy should arrange for the baby to be born in a unit where the baby can be well-monitored and treated for a few hours or days after birth if required.
Does labetalol cause low birth weight?
Many of the studies that were conducted on expectant mothers found no evidence that taking labetalol during pregnancy increased the risk of low birth weight in the baby. It is high blood pressure that causes less birth weight and not labetalol.
Can labetalol cause preterm birth?
Therefore, it cannot definitely be concluded that the medicines that are used to treat high blood pressure during pregnancy are actually responsible for preterm delivery. Some studies of preterm birth rate were conducted, in which it was found that taking labetalol during pregnancy is not linked to an increased risk of preterm birth.
When can you take lbetalol?
Labetalol supersedes all other medicines as a first-line drug and can be safely taken in the first trimester of pregnancy.
Does labetalol lower blood pressure during pregnancy?
Pregnancy is a time when you need to stay in good health to keep all the complications at bay. It is a well-known fact that la betalol is considered effective in lowering high blood pressure during pregnancy, but one must remain very careful about its probable side-effects as well. It slows the heart rate and improves blood flow, thus decreasing blood pressure. However, it does not cure it. The drug is only a part of the complete treatment for high blood pressure, which includes exercise, diet, and overall weight control. Hence, as a precautionary measure, one must know all about the medicine.
When should you monitor labetalol during pregnancy?
It has been suggested that preterm infants that were exposed to labetalol for a long-time during pregnancy should be carefully monitored during the first week after birth especially if the infant presents with complications such as lack of oxygen, seizures, heart defects, or electrolyte imbalance.
What is labetalol used for?
Labetalol is used to treat high blood pressure and chest pain. Labetalol works by slowing the heart rate and opening up blood vessels to improve blood flow and lower blood pressure.
Can labetalol cause a miscarriage?
Miscarriage can occur in any pregnancy. It is not known if labetalol increases the chance of miscarriage.
Can you take beta blocker after birth?
While not commonly observed, there have been instances where the effects of beta-blocker exposure occurred a week after birth, and the symptoms were more severe and life-threatening. Some of the observed symptoms were abnormal breathing, sepsis (blood infection) and seizures. More study is needed to prove an association. It has been suggested that preterm infants that were exposed to labetalol for a long-time during pregnancy should be carefully monitored during the first week after birth especially if the infant presents with complications such as lack of oxygen, seizures, heart defects, or electrolyte imbalance.
Can you breastfeed a baby with labetalol?
Labetalol has been found in small amounts in breastmilk. Because of this, it is not expected to cause problems in full-term breastfed infants. Be sure to talk to your healthcare provider about all of your breastfeeding questions.
Does labetalol make it harder to get pregnant?
There is no current data to suggest that taking labetalol makes it harder to become pregnant.
Does labetalol cause low birth weight?
Most studies do not find that labetalol itself increases the chance for low birth weight (less than 5 pounds 8 ounces), preterm delivery (delivery before 37 weeks of pregnancy), or stillbirth. There have been a few reports of labetalol exposure in late pregnancy leading to an infant having temporary symptoms of beta-blockade that appear shortly after birth. Beta-blockade symptoms are caused by a beta blocker being in the baby’s system. Symptoms include slowed heart rate, low blood pressure and low blood sugar and generally pass within 3 days.
What is the dosage for labetalol?
The recommended starting oral dose of labetalol is 100 mg twice daily, and the dose can be increased by 100 mg twice daily every 2-3 days based on the response of the blood pressure. Usual maintenance doses are 200-400 mg twice daily. Patients with severely high blood pressure may require 1.2 to 2.4 g daily.
What is labetalol used for?
Labetalol is used for the treatment of high blood pressure ( hypertension ).
How long does it take to take labetalol?
The initial intravenous dose of labetalol is 20 mg injected over 2 minutes. Additional injections of 40 or 80 mg may be administered every 10 minutes as needed up to a total dose of 300 mg. Labetalol also may be administered by intravenous infusion at 1-2 mg/minute.
How long does it take for labetalol to cause lightheadedness?
Patients should be observed for this possible side effect within two to four hours of the first labetalol dose and after any changes in dose.
When was labetalol approved?
When labetalol attaches to and blocks the receptors, arteries expand, resulting in a fall in blood pressure. The FDA approved labetalol in August 1984.
Does cimetidine increase labetalol?
Cimetidine ( Tagamet) may increase the effectiveness of labetalol by blocking its elimination and increasing its levels in the blood. Therefore, less labetalol may be needed when cimetidine and labetalol are used together. Halothane anesthesia may contribute to the blood pressure lowering effects of labetalol.
Does labetalol help with asthma?
If combined with adrenergic stimulating drugs used for treating asthma, for example, albuterol (Proventil, Ventolin) or pirbuterol (Maxair), the adrenergic blocking effects of labetalol may counteract the effects of the stimulating drugs and reduce their effectiveness for treating asthmatic attacks. More of the adrenergic drug may be needed.
Do drugs affect placental perfusion?
As pregnancy progresses, the impact of drugs on blood flow and placental perfusion must be addressed. Even if medications are not teratogenic, less easily detected effects on placental and fetal growth and metabolism are important.
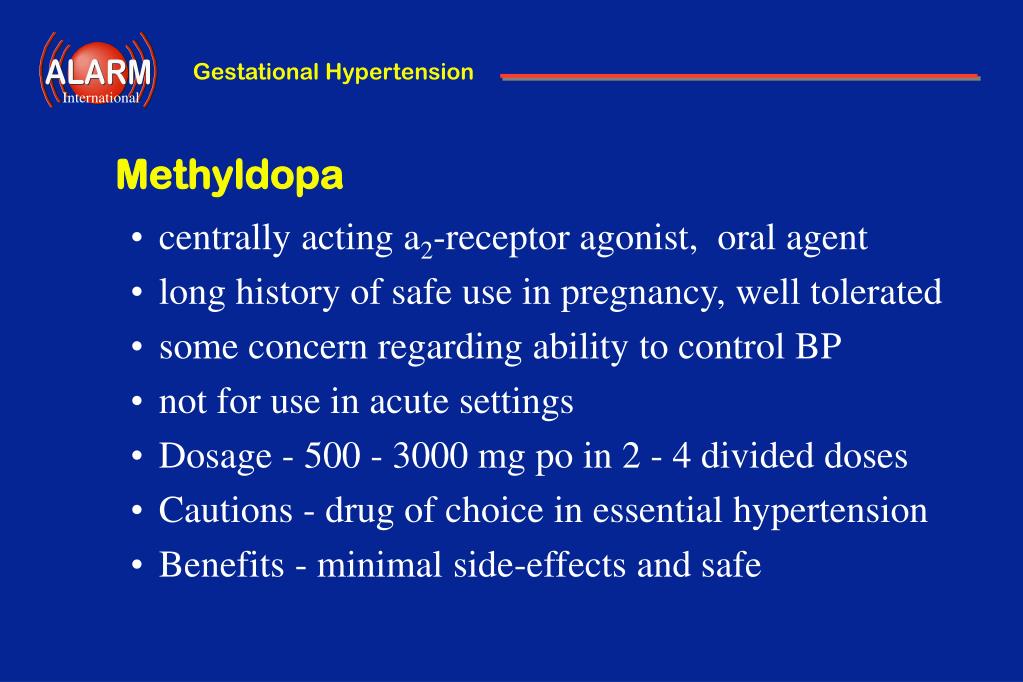
Is methyldopa safe for pregnancy?
The drugs most commonly used—methyldopa, labetalol, and nifedipine—are widely accepted as safe in pregnancy, based on many years of experience, observational data from large databases, and meta‐analyses of multiple small clinical trials.
Is amlodipine safe for pregnancy?
Safety of Amlodipine in Early Pregnancy. Hypertension is one of the most common medical complications of pregnancy. Clinical management is challenging; strategies that are standard of care in nonpregnant individuals, such as lowering blood pressure (BP) to 120/80 mm Hg, may be beneficial for maternal health 1 but must be considered carefully in ...
Is there any evidence for teratogenicity of antihypertensive drugs?
The conclusions of the authors were that although there is no compelling evidence for teratogenicity of most antihypertensive agents, the methodological weakness of the evidence prevents definitive answers about the safety of these drugs, even when including studies with hundreds of thousands of participants. 6.
Is nifedipine a vasodilator?
Nifedipine is also available in a short/immediate‐acting capsule and a prolonged‐acting tablet that is usually prescribed 2 to 3 times daily. Nifedipine is a vasodilator, and the shorter acting preparations are more likely to be associated with more rapid acute decreases in BP and reflex activation of the sympathetic nervous system, causing increases in heart rate and headaches, especially when used at higher doses (>60 mg/d). 15, 16 Moreover, abrupt decreases in BP associated with nifedipine capsules are potentially more problematic for placental perfusion. 17 Dose‐related maternal adverse effects attributable to nifedipine such as headache, tachycardia, hypotension flushing, and nausea have been well documented, 15 although no comparative data exist for amlodipine in pregnancy. Amlodipine, which has a gradual onset of action, 16 is less likely to be associated with vaso dilator symptoms and thus may be associated with better compliance and possibly smoother 24‐hour BP control compared with twice‐daily nifedipine tablets. 18 However, if the extended‐release preparation of nifedipine is used, the differences may not be significant in terms of 24‐hour BP control or side effects. 19 The slow onset of amlodipine also implies that antihypertensive effects are delayed (≈8 hours). 16 Limited information suggests that both nifedipine and amlodipine get into breast milk but are unlikely to be associated with adverse fetal effects. 20 Additional questions, not addressed by most studies, assess the impact of drug safety for different maternal diagnoses (eg, preeclampsia versus chronic hypertension) and pregnancy‐related changes in drug pharmacokinetics.
