Is Mycobacterium tuberculosis motile or nonmotile?
Mycobacterium tuberculosis is a nonmotile, non-spore-forming, obligate aerobe, acid-fast bacillus that often appears beaded or unstained using Gram stain. Like all mycobacteria, it is distinguished by its ability to form stable mycolate complexes with arylmethane dyes (carbolfuchsin, auramine, and rhodamine).May 23, 2016
How does the Mycobacterium tuberculosis move?
Transmission. TB is spread through the air from one person to another. Microscopic droplets that contain the bacteria may be expelled when a person who has infectious TB coughs or sneezes. They can remain suspended in the air for several hours, depending on the environment.Sep 22, 2014
Is Mycobacterium tuberculosis flagellated?
The bacterium has neither cilia or flagella, and is therefore non-motile. Its hydrophobic cell wall contains a high concentration of lipids which repels water. Metabolically, M. tuberculosis is obligate aerobic; it requires oxygen to undergo cellular respiration.Sep 27, 2010
What are the characteristics of Mycobacterium tuberculosis?
M. tuberculosis is a small, rod-shaped, strictly aerobic, acid-fast bacillus 1 . Like other mycobacteria, it is slow growing, resulting in more gradual development of disease when compared with other bacterial infections. Acid-fast bacilli are bacilli, which once stained, resist discoloration by acid and alcohol.
Is TB airborne or droplet?
Mycobacterium tuberculosis is transmitted in airborne particles called droplet nuclei that are expelled when persons with pulmonary or laryngeal TB cough, sneeze, shout, or sing.Oct 5, 2020
What are the virulence factors of Mycobacterium tuberculosis?
In the present review, the virulence determinants have been divided into the following categories based on their function, molecular features or cellular localization: (1) Lipid and fatty acid metabolism, including catabolism of cholesterol, (2) cell envelope proteins: including cell wall proteins, lipoproteins and ...
Is Mycobacterium smegmatis motile?
M. smegmatis is a non-motile bacterium which, due to its relatively fast growth, is used as a model for other mycobacteria, particularly Mycobacterium tuberculosis.Sep 22, 2020
Is Mycobacterium leprae motile?
An unculturable very slow-growing, acid-fast, obligate intracellular bacterium, which is non-motile and rod-shaped, Mycobacterium leprae is responsible for leprosy.
What is the morphology of Mycobacterium tuberculosis?
Mycobacterium tuberculosis is a fairly large nonmotile rod-shaped bacterium distantly related to the Actinomycetes. Many non pathogenic mycobacteria are components of the normal flora of humans, found most often in dry and oily locales. The rods are 2-4 micrometers in length and 0.2-0.5 um in width.
Why is Mycobacterium tuberculosis aerobic?
tuberculosis with a microscope. The physiology of M. tuberculosis is highly aerobic and requires high levels of oxygen. Primarily a pathogen of the mammalian respiratory system, it infects the lungs....Mycobacterium tuberculosisM. tuberculosis coloniesScientific classificationDomain:BacteriaPhylum:Actinomycetota9 more rows
Does Mycobacterium tuberculosis have DNA or RNA?
Mycobacterium tuberculosis contains at least nine small RNA families in its genome. The small RNA (sRNA) families were identified through RNomics – the direct analysis of RNA molecules isolated from cultures of Mycobacterium tuberculosis.
What type of organism is Mycobacterium tuberculosis?
Humans are the only reservoir for Mycobacterium tuberculosis. The organism is an acid-fast, aerobic bacillus with a high cell wall content of high-molecular-weight lipids. Visible growth takes 3 to 8 weeks on solid media.
Why is M. tuberculosis waxy?
First discovered in 1882 by Robert Koch, M. tuberculosis has an unusual, waxy coating on its cell surface primarily due to the presence of mycolic acid. This coating makes the cells impervious to Gram staining, and as a result, M. tuberculosis can appear either Gram-negative or Gram-positive.
What is the best way to identify M. tuberculosis?
Acid-fast stains such as Ziehl–Neelsen, or fluorescent stains such as auramine are used instead to identify M. tuberculosis with a microscope. The physiology of M. tuberculosis is highly aerobic and requires high levels of oxygen. Primarily a pathogen of the mammalian respiratory system, it infects the lungs.
What are the host derived lipids in M. tuberculosis?
tuberculosis, consisting entirely of host-derived lipids such as fats and cholesterol. Bacteria isolated from the lungs of infected mice were shown to preferentially use fatty acids over carbohydrate substrates.
What is XDR TB?
Additionally, extensively drug-resistant M. tuberculosis (XDR TB) is characterized by resistance to both isoniazid and rifampin, plus any fluoroquinolone and at least one of three injectable second-line drugs (i.e., amikacin, kanamycin, or capreomycin).
What is the growth rate of M. tuberculosis?
Compared to other commonly studied bacteria, M. tuberculosis has a remarkably slow growth rate, doubling roughly once per day. Commonly used media include liquids such as Middlebrook 7H9 or 7H12, egg-based solid media such as Lowenstein-Jensen, and solid agar-based such as Middlebrook 7H11 or 7H10.
Why are granulomas formed in M. tuberculosis?
Protective granulomas are formed due to the production of cytokines and upregulation of proteins involved in recruitment.
How long does it take for tuberculosis to divide?
M. tuberculosis divides every 18–24 hours. This is extremely slow compared with other bacteria, which tend to have division times measured in minutes ( Escherichia coli can divide roughly every 20 minutes). It is a small bacillus that can withstand weak disinfectants and can survive in a dry state for weeks.
Why is Mycobacterium tuberculosis unique to other bacteria?
Mycobacterium tuberculosis is unique to other bacteria because a large chunk of its coding capacity is dedicated for the production of enzymes that are involved in lipogenesis and lipolysis. Studies have shown that lipolytic enzymes are potential biomarkers for possible diagnoses of active Tuberculosis ( Badcock et al., ).
What is the cell membrane of M. tuberculosis made of?
A key factor of the M. tuberculosis cell membrane is that over 60% of it is made out of lipids. The cell wall of M. tuberculosis is unique in that it has mycolic acids, cord factor, and mAPG complex ( Todar ). Mycolic acids are long fatty acids found in the cell wall of M. Tuberculosis. Because mycolic acids contribute to ...
How big is a tuberculosis cell?
Here is some information regarding the cell structure for Mycobacterium tuberculosis, the cause for the horrid and contagious disease, Tuberculosis! Mycobacterium Tuberculosis has a rod-shape and its a pretty large bacteria! The length of the bacteria usually ranges from 2 to 4 micrometers and the width is somewhere between 0.2 to 0.5 micrometers.
How many base pairs are there in the genome of M. tuberculosis?
Size and shape of M. Tuberculosis. Next, the genome of M. tuberculosis is comprised of 4, 411, 529 base pairs and 4,000 different genes. Not to mention, M. tuberculosis ‘s genome has a very large guanine + cytosine content which is reflected in the amino acid content of the protein products. Mycobacterium tuberculosis is unique to other bacteria ...
What are mycolic acids?
Mycolic acids are long fatty acids found in the cell wall of M. Tuberculosis. Because mycolic acids contribute to the waxy-like coating on the cell surface, the bacterial cells are essentially impervious to normal gram staining techniques.
Is Mycobacterium tuberculosis a single-celled organism?
The length of the bacteria usually ranges from 2 to 4 micrometers and the width is somewhere between 0.2 to 0.5 micrometers. Interestingly, Mycobacterium tuberculosis is a non-motile bacteria ( Todar ). Additionally, because M. tuberculosis is a prokaryotic bacteria, it is a single-celled organism.
Is M. tuberculosis a Gram positive or negative?
Interestingly, M. tuberculosis is not classified as either gram positive or gram negative bacteria because it does not have all the characteristics that a gram +/- bacteria would typically have; M. Tuberculosis is considered to be an acid-fast bacteria.
What is post primary tuberculosis?
Post-primary tuberculosis. Reactivation of dormant foci of tubercle bacilli or exogenous reinfection leads to post-primary tuberculosis, which differs in several respects from the primary disease. For unknown reasons, reactivation or reinfection tuberculosis tends to develop in the upper lobes of the lungs.
What is considered positive for HIV?
For patients, at the highest risk of developing the active disease (eg, HIV-infected persons, people who have had exposure to persons with active tuberculosis) 5 mm or larger of induration is considered positive.
What is the atmosphere of the lung?
The atmosphere of the lung, with a high carbon dioxide level, is ideal for supporting the growth of the bacilli, and huge numbers of these are found in the cavity walls. Once the cavity is formed, large numbers of bacilli gain access to the sputum, and the patient becomes an open or infectious case.
Which cell entraps bacteria in the lung?
The bacteria are phagocytosed by alveolar macrophages in the lung, entraps the bacteria in phagosome and action of lysosome along with phagosome collectively called as phagolysosome to kill the bacteria.
What is the second line of fluoroquinolones?
Two or more core second-line agents include ethionamide, prothionamide, cycloserine, terizidone, clofazimine, or linezolid.
What are the three zones of granuloma?
When fully developed, this lesion, a chronic granuloma, consists of three zones. a central area of large, multinucleated giant cells containing tubercle bacilli; a mid-zone of pale epithelioid cells often arranged radially; and. a peripheral zone of fibroblasts, lymphocytes, and monocytes.
What is XDR TB?
The newer category of extensively drug-resistant tuberculosis (XDR-TB) is defined as resistance to, at least, isoniazid, rifampicin, fluoroquinolone, and any injectable agent. The second line drugs include. A later generation of fluoroquinolones such as moxifloxacin, levofloxacin, or gatifloxacin.
What is the etiological agent of paratuberculosis?
M. avium ssp. paratuberculosis (Map) is the etiological agent of paratuberculosis or Johne's disease in ruminants and Crohn disease in human patients. Susceptibility to disinfectants: Mycobacteria are susceptible to ionic detergents and phenolic disinfectants.
What are the most common pathogens in the genus Mycobacterium?
The genus Mycobacterium is composed of more than 100 recognized or proposed species. The most familiar pathogens are Mycobacterium tuberculosis complex (tuberculosis) and Mycobacterium leprae (leprosy or Hansen’s disease). Mycobacterium species produce a wide spectrum of infections in humans and animals ranging from localized lesions to disseminated disease. Most of the nontuberculous mycobacteria live freely in the environment and some have been implicated as opportunistic pathogens in patients with underlying lung disease, immunosuppression, or percutaneous trauma. New rapid culture methods and the application of molecular biology have decreased the time required to isolate and identify clinically significant mycobacteria.
How are mycobacteria phylogenetic studies based?
Phylogenetic studies of the genus Mycobacterium have been based, in the past three decades, on the sequence of the 16S rRNA gene, on concatenated sequences of a few housekeeping genes and, very recently, on whole genome sequences. Surprisingly these approaches produced highly consistent phylogenetic reconstructions. In all cases, the rapidly and slowly growing species were clearly separated. The species composition of the major clusters was largely overlapping and one of them, the M. terrae complex, constantly took its place between the branches leading to rapid and slow growers. The clade of rapid growers including the species of the M. abscessus-chelonae complex was revealed to be the most ancestral and is located close to the root of the genus. The pathogenic species ( M. tuberculosis and M. leprae) clustered together with most species frequently involved in opportunistic human infections. The major discrepancies among different phylogenetic approaches occurred with a group of species genetically related to M. simiae; the large grouping defined by the 16S sequences emerged scaled down in the phylogeny inferred by the whole genome sequences with most of them reallocated among other, apparently unrelated, species.
What happens when phages are lysed?
Mycobacteria captured by the phage immobilized on the electrode are lysed, resulting in a change to the electrical properties of the electrode which is monitored by the piezoelectric detection system.
Where can I find mycobacteria?
Mycobacteria are often found in waters that receive runoff from pasture land and in a study of the River Tywi in South Wales, UK, 48 of 70 water samples (69%) were contaminated with M. avium subsp. paratuberculosis ( Pickup et al., 2006 ).
Which mycobacteria have staining properties similar to pathogenic types?
The saprophytes have staining properties similar to the pathogenic types. Tubercle bacilli are the most important clinically significant mycobacteria. Numerous mechanisms have been associated with the susceptibility and development of disease in animals exposed to virulent tubercle bacilli.
Where do mycobacteria live?
The latter are ubiquitous in the environment and occur in soil and water ; some of them are present in the gastrointestinal tract of some humans and animals.
Overview
Mycobacterium tuberculosis (M. tb) is a species of pathogenic bacteria in the family Mycobacteriaceae and the causative agent of tuberculosis. First discovered in 1882 by Robert Koch, M. tuberculosis has an unusual, waxy coating on its cell surface primarily due to the presence of mycolic acid. This coating makes the cells impervious to Gram staining, and as a result, M. tuberculosis can appear …
Microbiology
M. tuberculosis was found in a complex in 2019 that has at least 9 members: M. tuberculosis sensu stricto, M. africanum, M. canetti, M. bovis, M. caprae, M. microti, M. pinnipedii, M. mungi, and M. orygis. It requires oxygen to grow, it is debated whether it produces spores, and is nonmotile. M. tuberculosis divides every 18–24 hours. This is extremely slow compared with other bacteria, which tend to have division times measured in minutes (Escherichia colican divide roughly ever…
Pathophysiology
Humans are the only known reservoirs of M. tuberculosis. A misconception is that M. tuberculosis can be spread by shaking hands, making contact with toilet seats, sharing food or drink, or sharing toothbrushes. However, major spread is through air droplets originating from a person who has the disease either coughing, sneezing, speaking, or singing.
Genome
The genome of the H37Rv strain was published in 1998. Its size is 4 million base pairs, with 3,959 genes; 40% of these genes have had their function characterized, with possible function postulated for another 44%. Within the genome are also six pseudogenes.
The genome contains 250 genes involved in fatty acid metabolism, with 39 of these involved in the polyketidemetabolism generating the waxy coat. Such large numbers of conserved genes show …
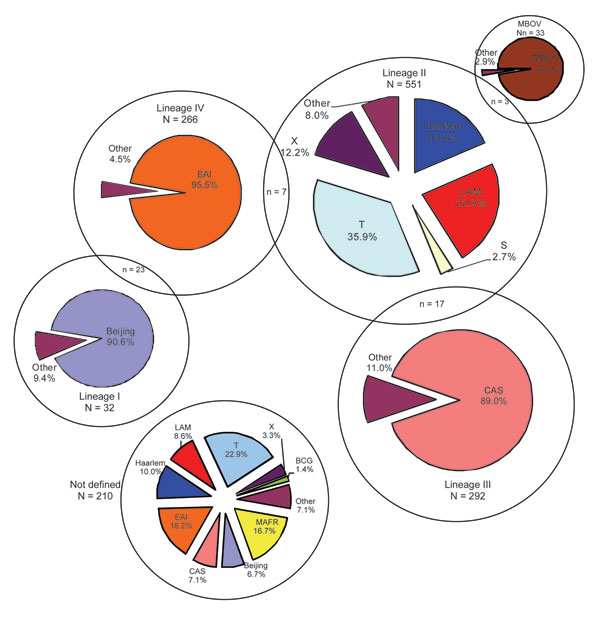
Evolution
The M. tuberculosis complex evolved in Africa and most probably in the Horn of Africa. In addition to M. tuberculosis, the M. tuberculosis complex(MTBC) has a number of members infecting various animal species, these include M. africanum, M. bovis (Dassie's bacillus), M. caprae, M. microti, M. mungi, M. orygis, and M. pinnipedii. This group may also include the M. canettii clade. These animal strains of MTBC do not strictly deserve species status, as they are all closely relat…
Antibiotic resistance (ABR)
M. tuberculosis is a clonal organism and does not exchange DNA via horizontal gene transfer. Despite an additionally slow evolution rate, the emergence and spread of antibiotic resistance in M. tuberculosis poses an increasing threat to global public health. In 2019, the WHO reported the estimated incidence of antibiotic resistant TB to be 3.4% in new cases, and 18% in previously treated cases. Geographical discrepancies exist in the incidence rates of drug-resistant TB. Cou…
Host genetics
The nature of the host-pathogen interaction between humans and M. tuberculosis is considered to have a genetic component. A group of rare disorders called Mendelian susceptibility to mycobacterial diseases was observed in a subset of individuals with a genetic defect that results in increased susceptibility to mycobacterial infection.
Early case and twin studies have indicated that genetic components are important in host susce…
DNA repair
As an intracellular pathogen, M. tuberculosis is exposed to a variety of DNA-damaging assaults, primarily from host-generated antimicrobial toxic radicals. Exposure to reactive oxygen species and/or reactive nitrogen species causes different types of DNA damage including oxidation, depurination, methylation, and deamination that can give rise to single- and double-strand breaks (DSBs).