Is PNH an autoimmune hemolytic anemia?
Autoimmune hemolytic anemia (AIHA) and paroxysmal nocturnal hemoglobinuria (PNH) are distinct blood disorders with different underlying causes and treatment approaches. Each is rare and potentially fatal.
Is PNH a progressive disease?
PNH is a chronic, progressive, debilitating, and life-threatening ultra-rare blood disorder characterized by complement-mediated hemolysis (destruction of red blood cells).
What is the major cause of PNH?
Causes. Variants (also known as mutations) in the PIGA gene cause almost all cases of PNH. Variants in the PIGT gene cause the rare, inflammatory form of the condition. The proteins produced from both genes are involved in a multistep process that connects particular proteins to the surface of cells.
What is the survival rate of PNH?
The disease process of PNH is insidious and has a chronic course, with a median survival of about 10.3 years. Morbidity depends on the variable expressions of hemolysis, bone marrow failure, and thrombophilia that define the severity and clinical course of the disease.
How many people in the world have PNH?
PNH is characterized by destruction of red blood cells (hemolytic anemia), blood clots (thrombosis), and impaired bone marrow function (not making enough of the three blood components). PNH affects 1-1.5 persons per million of the population.
Does PNH go into remission?
Nevertheless, as our study shows, true remissions occur, but the patients need to be carefully followed up for a potential emergence of malignancy. Among the six patients, where the PNH clone disappeared, four are healthy and have no treatment.
Can PNH go away?
Paroxysmal nocturnal hemoglobinuria (PNH) is considered to be curable only through the means of allogeneic stem cell transplantation (SCT) [1].
Are you born with PNH?
People aren't born with PNH, and you can't pass it along to your child. It happens when a certain gene (called PIGA) in your bone marrow's stem cells mutates. This affects the way these stem cells create red blood cells. Once the gene mutates, the stem cells make red blood cells that are missing a protein.
Is there a cure for PNH?
The only way to cure PNH is with what's called an allogenic stem cell transplant. Also called a bone marrow transplant, it replaces your damaged stem cells with healthy ones from a donor, usually a close relative because they're often the best match.
Can you live with PNH?
Most cases of PNH can be life threatening. The average survival period after diagnosis is 10 years, but some people live for several decades and only experience minor symptoms.
How do you get PNH disease?
PNH is caused by a problem with a gene. But you don't get it from your parents, and you can't pass it on to your kids. A change in a gene, called a mutation, causes your body to make abnormal red blood cells. These cells don't have proteins that shield them from your immune system.
Can you drink alcohol with PNH?
Drink Lots of Water It's also a good idea to limit alcohol and caffeine. Staying hydrated is really important, and water is your best bet.
Can PNH go away?
Paroxysmal nocturnal hemoglobinuria (PNH) is considered to be curable only through the means of allogeneic stem cell transplantation (SCT) [1].
How does PNH develop?
Most likely, PNH arises in the setting of autoimmune bone marrow failure, as occurs in most cases of acquired aplastic anemia. Researchers believe that defective PNH stem cells survive the misguided attack by the immune system and multiply, while healthy stem cells are destroyed, resulting in the development of PNH.
Can PNH turn into MDS?
People with PNH can share symptoms with aplastic anemia patients, such as low blood cell counts. On average, 2 out of 100 people with PNH go on to develop myelodysplastic syndrome (MDS).
Can you live with PNH?
Most cases of PNH can be life threatening. The average survival period after diagnosis is 10 years, but some people live for several decades and only experience minor symptoms.
What is PNH in medical terms?
Paroxysmal nocturnal hemoglobinuria (PNH) is an acquired disorder that leads to the premature death and impaired production of blood cells. It can occur at any age, but is usually diagnosed in young adulthood. People with PNH have recurring episodes of symptoms due to hemolysis, which may be triggered by stresses on the body such as infections ...
What is related disease?
Related diseases are conditions that have similar signs and symptoms. A health care provider may consider these conditions in the table below when making a diagnosis. Please note that the table may not include all the possible conditions related to this disease.
Is PNH inherited?
It is caused by acquired, rather than inherited , mutations in the PIGA gene; the condition is not passed down to children of affected individuals.
Can aplastic anemia cause PNH?
Sometimes, people who have been treated for aplastic anemia may develop PNH. [1] . The treatment of PNH is largely based on symptoms; stem cell transplantation is typically reserved for severe cases of PNH with aplastic anemia or those whose develop leukemia. [2] Last updated: 1/15/2011.
What is the primary clinical finding associated with PNH?
The premature destruction of red blood cells (hemolysis) is the primary clinical finding associated with PNH. Hemolysis may result in hemoglobin in the urine, although many individuals with hemolysis do not have visible hemoglobin in the urine. When hemolysis occurs, a red blood cell’s outer wall (membrane) breaks down (lysis) releasing hemoglobin. Hemoglobin is excreted from the body in the urine, resulting in the dark-colored or blood colored urine (hemoglobinuria) that is characteristic of this disorder. Hemolysis is ongoing, but may worsen (i.e., a person may have a hemolytic episode) during periods of infection, trauma or stress. The premature destruction of red blood cells may result in low levels of circulating red blood cells (hemolytic anemia) that is made worse by the underlying bone marrow dysfunction.
What is the test for PNH?
The main diagnostic test for individuals with suspected PNH is flow cytometry, a blood test that can identify PNH cells (blood cells that are missing GPI-anchored proteins).
What is the name of the disorder in which red blood cells break apart?
Paroxysmal nocturnal hemoglobinuria (PNH) is a rare disorder in which red blood cells break apart prematurely. It is an acquired hematopoietic stem cell disorder. Hematopoietic stem cells are created in the bone marrow, the spongy center of the long bones of the body. These cells grow and eventually develop into red blood cells, white blood cells and platelets. Some hematopoietic stem cells in individuals with PNH are defective and consequently produce defective blood cells. These defective red blood cells of PNH are extremely susceptible to premature destruction by a particular part of a person’s own immune system called the complement system. The destruction of red blood cells (hemolysis) by complement leads to episodes of hemoglobin in the urine (hemoglobinuria). Hemoglobin is the red, iron-rich, oxygen-containing pigment of the blood. Individuals with hemoglobinuria may exhibit dark-colored or blood colored urine. This finding is most prominent in the morning, after the urine has concentrated overnight during sleep. However, hemolysis in individuals with PNH is a constant process (i.e., it does not occur only at night). Hemoglobin in the urine may not always be visible to the eye. In addition to hemolysis, individuals with PNH are also susceptible to developing repeated, potentially life-threatening blood clots (thromboses). Affected individuals also have some degree of underlying bone marrow dysfunction. Severe bone marrow dysfunction results in low levels of red and white blood cells and platelets (pancytopenia). The specific symptoms of PNH vary greatly from one person to another and affected individuals usually do not exhibit all of the symptoms associated with the disorder.
Why is paroxysmal nocturnal hemoglobinuria called paroxysmal nocturnal?
The disorder was termed paroxysmal nocturnal hemoglobinuria because of the mistaken belief that hemolysis and subsequent hemoglobinuria occurred in only in intermittent episodes (paroxysmally) and with greater frequency during the night (nocturnal).
Why do people with PNH need folic acid?
Some individuals with PNH receive folic acid (folate) supplements to insure that the supply of folate is adequate as demand increases when the bone marrow attempts to compensate for the hemolytic anemia of PNH by augmenting red blood cell production (erythropoiesis) in the bone marrow. Supplemental iron should be given to individuals with iron-deficiency, which can occur because of red blood cell destruction and the consequent loss of iron in the urine.
How many people have PNH?
The prevalence is estimated to be between 0.5-1.5 per million people in the general population. The disorder has been described in many racial groups and has been identified in all areas of the world. The disorder may occur with greater frequency in individuals of Southeast Asia or the Far East who experience greater rates of aplastic anemia. The disorder can affect any age group. The median age at diagnosis is during the 30s.
What is defective in PNH?
Some hematopoietic stem cells in individuals with PNH are defective and consequently produce defective blood cells. These defective red blood cells of PNH are extremely susceptible to premature destruction by a particular part of a person’s own immune system called the complement system. The destruction of red blood cells (hemolysis) ...
Why does PNH occur?
PNH occurs because of a genetic change ( mutation) in the PIG-A gene of a single stem cell in your bone marrow. Here are the steps that lead to PNH: The abnormal stem cell makes copies of or "clones" itself. This leads to a whole population of bone marrow stem cells that have mutant PIG-A.
How to understand PNH?
To understand PNH, you must first learn how your immune system works, and how your bone marrow makes blood. This section defines the process and explains what goes wrong when you get PNH.
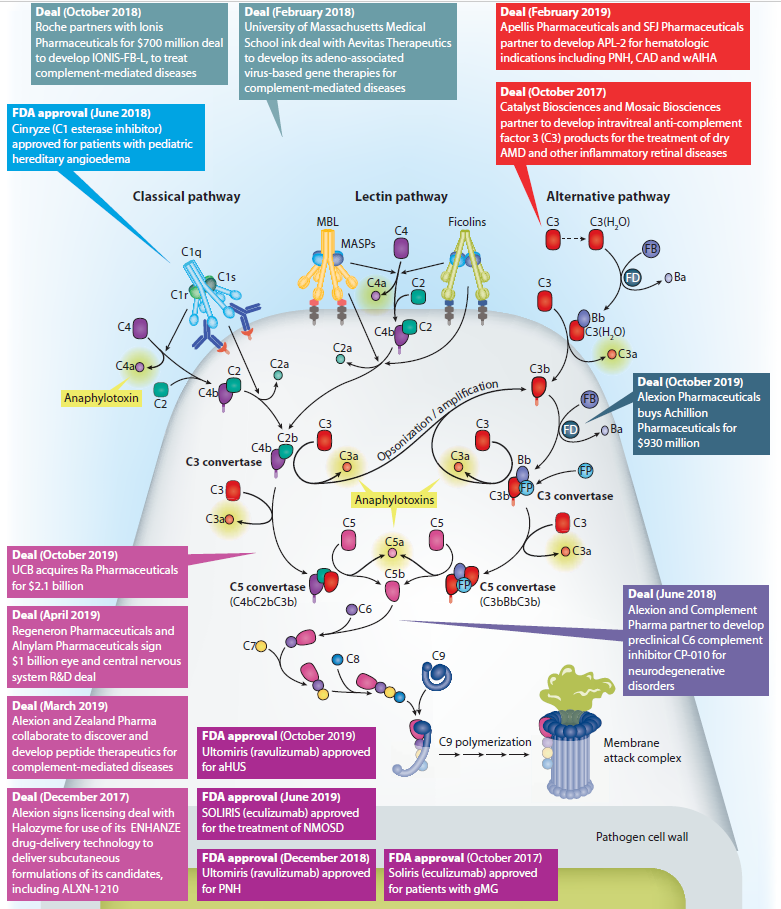
What is the complement system in PNH?
The complement system is a group of proteins in the blood. They help support (complement) the work of white blood cells by fighting infections.
How many people with aplastic anemia develop PNH?
More than 10 out of every 100 people with aplastic anemia will develop PNH. In addition, some people with PNH will develop aplastic anemia. People with PNH can share symptoms with aplastic anemia patients, such as low blood cell counts. On average, 2 out of 100 people with PNH go on to develop myelodysplastic syndrome (MDS).
How many people with PNH develop MDS?
On average, 2 out of 100 people with PNH go on to develop myelodysplastic syndrome (MDS).
Do PNH cells have a shield?
The PNH red blood cells lack the shield of proteins that protect normal red blood cells from the complement system, leaving them open to attack and destruction by the complement system proteins. Many healthy people have a small number of PNH stem cells.
Can you have severe PNH?
The course and impact of PNH may vary from person to person. You may have only mild symptoms, or you may have severe symptoms and need medicines or blood transfusions.
Overview
PNH is a rare disease in which the body’s red blood cells are prematurely destroyed. PNH is an acquired, not inherited, hematopoietic stem cell disorder, caused by mutation of the PIGA gene which causes defective blood cells to multiply.
Common Symptoms
Darker urine, erectile dysfunction/male impotence, severe bone marrow dysfunction, blood clots, acute and chronic renal (kidney) disease, rapid heart beat, chest pains, difficulty breathing when exercising, difficulty swallowing (dysphagia), painful abdominal contractions, esophageal spasms, fatigue, and headaches.
Coexisting Diseases and Conditions
Hemoglobinuria, thromboses, thrombocytopenia, bone marrow dysfunction, pancytopenia, leukemia (rarely), Budd-Chiari syndrome, refractory anemia, aplastic anemia, and myelodysplastic syndrome.
Risk Factors
Females are believed to be affected at slightly higher rates. While the disease can impact someone of any age, the median age is 30-40.
What is the cause of PNH?
PNH results from a genetic mutation in the stem cells that form RBCs and other immune cells. This mutation prevents a class of proteins called glycosylphosphatidylinositol (GPI)-anchored proteins from developing on the surface of RBCs.
Why does PNH occur?
According to the National Organization for Rare Disorders, the mutation responsible for PNH occurs for no apparent reason. The random nature of the mutation makes it difficult to predict which people are at risk of developing PNH in the general population.
What is the best treatment for PNH?
The Food and Drug Administration (FDA) approved the first drug to treat PNH in 2007. The drug, known as eculizumab (Soliris), is a humanized monoclonal antibody. It slows down or halts the breakdown of RBCs by blocking the immune system from destroying them, and it reduces the risk of blood clots. People with PNH need to take eculizumab every 2 weeks.
How long does a person live with PNH?
Most cases of PNH can be life threatening. The average survival period after diagnosis is 10 years, but some people live for several decades and only experience minor symptoms.
What is paroxysmal hemoglobinuria?
Paroxysmal nocturnal hemoglobinuria is a rare blood disease that affects a person’s quality of life and increases the risk of health complications.
How long does it take to get diagnosed with PNH?
People with PNH tend to receive a diagnosis months or years after their symptoms first appear. The reason for this is that the symptoms of PNH are nonspecific, so it is easy to mistake the condition for other diseases.
How many subtypes of PNH are there?
Researchers have so far identified three subtypes of PNH:
What is PNH in medical terms?
Specialty. Hematology. Paroxysmal nocturnal hemoglobinuria ( PNH) is a rare, acquired, life-threatening disease of the blood characterized by destruction of red blood cells by the complement system, a part of the body's innate immune system. This destructive process occurs due to deficiency of the red blood cell surface protein DAF, ...
How to tell if you have PNH?
Signs and symptoms. The classic sign of PNH is red discoloration of the urine due to the presence of hemoglobin and hemosiderin from the breakdown of red blood cells. As the urine is more concentrated in the morning, this is when the color is most pronounced.
What is the name of the disease that causes the destruction of red blood cells?
Paroxysmal nocturnal hemoglobinuria. Paroxy smal nocturnal hemoglobinuria ( PNH) is a rare, acquired, life-threatening disease of the blood characterized by destruction of red blood cells by the complement system, a part of the body's innate immune system. This destructive process occurs due to deficiency of the red blood cell surface protein DAF, ...
What is the only hemolytic anemia caused by an acquired (rather than inherited) intrinsic defect in the cell?
PNH is the only hemolytic anemia caused by an acquired (rather than inherited) intrinsic defect in the cell membrane (deficiency of glycophosphatidylinositol or GPI) leading to the absence of protective exterior surface proteins that normally attach via a GPI anchor. It may develop on its own ("primary PNH") or in the context of other bone marrow disorders such as aplastic anemia ("secondary PNH "). Only a minority of affected people have the telltale red urine in the morning that originally gave the condition its name.
How often should I monitor flow cytometry for PNH?
PNH is a chronic condition. In patients with only a small clone and few problems, monitoring of the flow cytometry every six months gives information on the severity and risk of potential complications. Given the high risk of thrombosis in PNH, preventive treatment with warfarin decreases the risk of thrombosis in those with a large clone (50% of white blood cells type III).
Who first described paroxysmal hemoglobinuria?
The first description of paroxysmal hemoglobinuria was by the German physician Paul Strübing ( Greifswald, 1852–1915) during a lecture in 1881, later published in 1882. Later comprehensive descriptions were made by Ettore Marchiafava and Alessio Nazari in 1911, with further elaborations by Marchiafava in 1928 and Ferdinando Micheli in 1931.
Is bone marrow transplantation the only cure for PNH?
Allogeneic bone marrow transplantation is the only cure, but has significant rates of additional medical problems and death. The monoclonal antibody eculizumab reduces the need for blood transfusions and improves quality of life for those affected by PNH.
What is the rarest autoimmune disease?
Here are 10 in the category of rare autoimmune diseases: 1. Eosinophilic granulomatosis with polyangiitis (EGPA) Formerly known as Churg Strauss syndrome, this autoimmune disease is characterized by elevated levels of white blood cells called eosinophils, which often leads to inflammation in blood vessels. That, in turn, can lead ...
Why do people with autoimmune disease have trouble urinating?
People with this autoimmune disease have trouble urinating because extra fibrous tissue grows up to create masses that block the ureters, which are the tubes that carry urine from the kidneys to the bladder. As a result, toxic chemicals can build up in the blood, and kidney damage can develop. 9. Scleroderma.
What is the disease that causes redness in the mouth and lips?
Kawasaki disease. Like EGPA, Kawasaki disease involves vasculitis, or the inflammation of blood vessels. It affects young children, typically showing up with a high fever, a rash, swollen lymph nodes and redness inn the lips, eyes and mouth. 4.
How does a rare disease affect your life?
Find the support you need. Having a rare disease can turn your life upside down. Not only can be it challenging to explain to other people, it can affect every aspect of your life in ways that other people can’t quite grasp. That’s why it’s so crucial to reach out for support if you are diagnosed with one.
How many people are affected by a rare disease?
According to the National Institutes of Health, a rare disease is one that affects fewer than 200,000 people at any particular time in the United States.
Is there more knowledge about rare diseases?
The good news: there is more knowledge now about many of these rare diseases, and research into rare diseases is ongoing, through initiatives like the Rare Diseases Clinical Research Network, which is funded by the National Institutes of Health (NIH).

Symptoms
Prognosis
Pathophysiology
- The premature destruction of red blood cells (hemolysis) is the primary clinical finding associated with PNH. Hemolysis may result in hemoglobin in the urine, although many individuals with hemolysis do not have visible hemoglobin in the urine. When hemolysis occurs, a red blood cells outer wall (membrane) breaks down (lysis) releasing hemoglobin. Hemoglobin is excreted from …
Signs and symptoms
- Chronic hemolysis is central to all the symptoms and physical findings associated with PNH. Mild hemolysis can cause fatigue, rapid heartbeat, headaches, chest pain and difficulty breathing when exercising. If hemolysis is severe, additional symptoms can develop including disabling fatigue, difficulty swallowing (dysphagia) and painful contractions that affect the abdomen, the esophag…
Cause
- Many individuals with PNH may simultaneously have another, closely-related disorder known as acquired aplastic anemia. To a lesser extent, some individuals may have myelodysplasia. Although the exact relationship among these disorders is unknown, researchers now believe that PNH arises from autoimmune bone marrow failure, which is the cause of most...
Function
- The PIGA gene produces a protein that is essential to the creation (biosynthesis) of glycosyl phosphatidylinositol (GPI) anchors. These anchors allow some proteins to attach to a cells membrane. These proteins are called GPI-anchored proteins. In cells with a PIGA gene mutation, the GPI anchors are not formed, and, consequently, GPI-anchored proteins cannot attach to the …
Epidemiology
- PNH is believed to affect males and females in equal numbers, although some studies show a slight female preponderance. The prevalence is estimated to be between 0.5-1.5 per million people in the general population. The disorder has been described in many racial groups and has been identified in all areas of the world. The disorder may occur with greater frequency in individ…
History
- PNH was first reported in the medical literature in the latter half of the 19th century. The disorder was termed paroxysmal nocturnal hemoglobinuria because of the mistaken belief that hemolysis and subsequent hemoglobinuria occurred in only in intermittent episodes (paroxysmally) and with greater frequency during the night (nocturnal). However, while hemoglobinuria may appear paro…
Diagnosis
- Symptoms of the following disorders can be similar to those of PNH. Comparisons may be useful for a differential diagnosis. necessary for a differential diagnosis: A diagnosis of PNH may be suspected in individuals who have symptoms of intravascular hemolysis (e.g., hemoglobinuria, abnormally high serum LDH concentration) with no known cause. A diagnosis may be made bas…
Overview
- Paroxysmal cold hemoglobinuria is a rare autoimmune hemolytic disorder characterized by the premature destruction of healthy red blood cells (hemolysis) minutes to hours after exposure to cold. Autoimmune diseases occur when the bodys natural defenses against invading organisms mistakenly destroy healthy tissue for unknown reasons. Normally, red blood cells have a life spa…
Treatment
- Treatment The treatment of PNH is directed at the specific symptoms that are present in each individual and includes a variety of different therapeutic options. In 2007, the U.S. Food and Drug Administration (FDA) approved the orphan drug eculizumab (Soliris®) as a treatment for PNH. This is the first drug to be approved for this disorder. Soliris does not cure PNH but halts the bre…
Research
- In 2009, Canadas national healthcare regulatory agency, Health Canada, approved the use of Soliris® (eculizumab) for the treatment of patients in Canada with paroxysmal nocturnal hemoglobinuria (PNH).
Management
- The administration of drugs that block the formation of blood clots (anticoagulation therapy) may be prescribed. Some individuals may be placed on long-term anticoagulant therapy. Use of blood thinners must be strictly managed because of the risk of excessive bleeding due to low platelet numbers in some individuals.
Resources
- Information on current clinical trials is posted on the Internet at www.clinicaltrials.gov. All studies receiving U.S. government funding, and some supported by private industry, are posted on this government web site.