
The murmur of tricuspid regurgitation is frequently not heard. When evident, it is a holosystolic murmur heard best at the left middle or lower sternal border or at the epigastrium with the bell of the stethoscope when the patient is sitting upright or standing.
What you should know about tricuspid regurgitation?
What you should know about tricuspid regurgitation
- Overview. People who have an echocardiogram (a very common heart test, usually done in basically healthy people) are told they have tricuspid regurgitation – a “leaky” tricuspid heart valve that ...
- Tricuspid valve and tricuspid regurgitation. ...
- risk. ...
- reason. ...
- symptom. ...
- diagnosis. ...
- manage. ...
- treat. ...
What are the symptoms of tricuspid valve regurgitation?
- Shortness of breath, especially with exertion or when you lie down
- Fatigue, especially during times of increased activity
- Cough, especially at night or when lying down
- Heart palpitations
- Swollen feet or ankles
- Chest pain (angina) or tightness
- Dizziness
Is it normal to have mild mitral regurgitation?
People also ask, is mild mitral regurgitation normal? When it's mild, mitral valve regurgitation usually does not cause any problems. However, severe mitral valve regurgitation can lead to complications, including: Heart failure. Heart failure results when your heart can't pump enough blood to meet your body's needs.
Is mild tricuspid regurgitation dangerous?
Tricuspid regurgitation (TR) is the most common lesion of the tricuspid valve (TV). Mild TR is common and usually is benign. However, moderate or severe TR can lead to irreversible myocardial damage and adverse outcomes. Despite these findings, few patients with significant TR undergo surgery.
Is tricuspid regurgitation a systolic or diastolic murmur?
Conversely, regurgitation of the same valves will result in a diastolic murmur as blood flows backward through the diseased valve when ventricular pressures drop during relaxation. Regarding the mitral and tricuspid valves, stenosis would result in a diastolic murmur and regurgitation a systolic murmur.
What type of murmur is tricuspid regurgitation?
The murmur of tricuspid regurgitation is similar to that of mitral regurgitation. It is a high pitched, holosystolic murmur however it is best heard at the left lower sternal border and it radiates to the right lower sternal border.
Is tricuspid stenosis a diastolic murmur?
Tricuspid stenosis is the rarest of all causes for a diastolic murmur. Usually, it is found in patients with rheumatic heart disease.
What are the diastolic murmurs?
A diastolic heart murmur is an unusual “whoosh” sound in your heart. It occurs when your heart relaxes between beats (diastole). Sometimes, diastolic murmurs don't need treatment. Other times, heart murmurs are a sign of another heart condition.
What conditions cause diastolic murmurs?
Diastolic murmurs are due to a narrowing (stenosis) of the mitral or tricuspid valves, or regurgitation of the aortic or pulmonary valves.
Why does tricuspid stenosis cause diastolic murmur?
Common causes include aortic or pulmonary regurgitation and left anterior descending artery stenosis. Mid-diastolic murmurs start after S2 and end before S1. They are due to turbulent flow across the atrioventricular (mitral & tricuspid) valves during the rapid filling phase from mitral or tricuspid stenosis.
How do you know if a murmur is systolic or diastolic?
Systolic murmurs occur between the first heart sound (S1) and the second heart sound (S2). Diastolic murmurs occur between S2 and S1. In addition, timing is used to describe when murmurs occur within systole or diastole.
Is aortic regurgitation a diastolic murmur?
Aortic regurgitation (AR) The murmur of aortic regurgitation is a soft, high-pitched, early diastolic decrescendo murmur usually heard best at the third intercostal space on the left (Erb's point) at end expiration while the patient is sitting up and leaning forward.
Is mitral regurgitation a systolic murmur?
Mitral regurgitation is a systolic murmur, best heard at the left 5th midclavicular line with possible radiation to the left axilla. It is commonly associated with infective endocarditis, rheumatic heart disease, congenital anomalies, and inferior wall myocardial infarctions.
Which murmurs are systolic?
A systolic murmur is a murmur that begins during or after the first heart sound and ends before or during the second heart sound.
What are the 3 kinds of murmurs of the heart?
Types of murmurs include the following:Systolic murmur. A heart murmur that occurs during a heart muscle contraction. ... Diastolic murmur. A heart murmur that occurs during heart muscle relaxation between beats. ... Continuous murmur. A heart murmur that occurs throughout the cardiac cycle.
What type of murmur is mitral regurgitation?
Mitral regurgitation is a systolic murmur, best heard at the left 5th midclavicular line with possible radiation to the left axilla. It is commonly associated with infective endocarditis, rheumatic heart disease, congenital anomalies, and inferior wall myocardial infarctions.
What does a tricuspid valve murmur sound like?
2:054:19Heart Sounds and Heart Murmurs, Animation. - YouTubeYouTubeStart of suggested clipEnd of suggested clipThis results in a crescendo decrescendo. Or a diamond-shaped murmur which starts a short momentMoreThis results in a crescendo decrescendo. Or a diamond-shaped murmur which starts a short moment after s1 it is often preceded by an ejection click caused. By the opening of the stenotic valve.
Can tricuspid regurgitation cause a heart murmur?
(Tricuspid Insufficiency; Tricuspid Incompetence) The most common cause is dilation of the right ventricle. Symptoms and signs are usually absent, but severe TR can cause neck pulsations, a holosystolic murmur, and right ventricular–induced heart failure or atrial fibrillation.
How can you tell the difference between tricuspid and VSD regurgitation?
¶ Innocent Still murmur and tricuspid regurgitation can also be heard in this location and can be distinguished from VSD murmurs by the quality and timing of the murmur (VSD murmurs are harsh and holosystolic [although small muscular defects may produce early systolic murmurs]; Still murmur has a vibratory or musical ...
What is the condition that affects the tricuspid valve?
Congenital heart disease. You may be born with a condition or heart defect that affects your tricuspid valve, such as Ebstein's anomaly.
What causes tricuspid valve to stop working?
Tricuspid valve regurgitation is usually caused by the lower right heart chamber (right ventricle) increasing in size , which can cause the tricuspid valve to stop working properly.
What is the name of the valve that allows blood to flow back into the heart?
This situation results in blood flowing back into your heart's upper right chamber (right atrium). A normal heart is shown on the left. Tricuspid valve regurgitation is a condition in which the valve between the two right heart chambers (right ventricle and right atrium) doesn't close properly. The malfunctioning valve allows blood ...
Why does the pressure in the right ventricle rise?
In severe tricuspid valve regurgitation, pressure can rise in your right ventricle due to blood flowing backward into the right atrium and less blood flowing forward through the right ventricle and into the lungs. Your right ventricle can expand and weaken over time, leading to heart failure.
What is the name of the valve that doesn't close properly?
Tricuspid valve regurgitation. In tricuspid valve regurgitation, shown in the heart on the right, the valve between the two right heart chambers (right ventricle and right atrium) doesn't close properly. This situation results in blood flowing back into your heart's upper right chamber (right atrium).
Why does the tricuspid valve flap close?
Then the flaps close to prevent the blood that has just passed into the right ventricle from flowing backward. In tricuspid valve regurgitation, the tricuspid valve doesn't close tightly. This causes the blood to flow back into the right atrium during each heartbeat.
Why does blood leaking backwards into the right atrium?
Tricuspid valve regurgitation in children is usually caused by heart disease present at birth (congeni tal heart disease). Ebstein's anomaly is the most common congenital heart disease that causes the condition.
Where to hear tricuspid regurgitation?
When evident, it is a holosystolic murmur heard best at the left middle or lower sternal border or at the epigastrium with the bell of the stethoscope when the patient is sitting upright or standing. The murmur may be high-pitched if TR is trivial and due to pulmonary hypertension, or it may be medium-pitched if TR is severe and has other causes. When the murmur is not present at all, the diagnosis is best made by the appearance of the jugular venous wave pattern and the presence of hepatic systolic pulsations. The murmur varies with respiration, becoming louder with inspiration (Carvallo sign).
Where is the heart murmur heard?
Heart sounds include a holosystolic murmur heard best at the left middle or lower sternal border or at the epigastrium when the patient is sitting upright or standing; the murmur becomes louder with inspiration. TR is usually well tolerated, but severe cases may require annuloplasty, valve repair, or valve replacement.
What is TR in heart?
Tricuspid regurgitation (TR) is insufficiency of the tricuspid valve causing blood flow from the right ventricle to the right atrium during systole. The most common cause is dilation of the right ventricle. Symptoms and signs are usually absent, but severe TR can cause neck pulsations, a holosystolic murmur, and right ventricular–induced heart failure or atrial fibrillation. Diagnosis is by physical examination and echocardiography. TR is usually benign and does not require treatment, but some patients require annuloplasty or valve repair or replacement.
Can tricuspid regurgitation cause neck pulsations?
Tricuspid regurgitation usually causes no symptoms, but some patients experience neck pulsations due to elevated jugular pressures. Symptoms of severe TR include fatigue, abdominal bloating, and anorexia. Patients may also develop symptoms of AF or atrial flutter.
Can TR cause neck pulsations?
Symptoms and signs are usually absent, but severe TR can cause neck pulsations, a holosystolic murmur, and right ventricular–induced heart failure or atrial fibrillation. Diagnosis is by physical examination and echocardiography.
Is RV regurgitation a decompensation?
However, in contrast to left-sided valvular regurgitation, there is no robust way to discern when the RV is starting to decompensate. Given this, patients are commonly referred late for surgery. In the context of the significant risks of surgery the overall outcome is poor.
Is a murmur high or medium?
The murmur may be high-pitched if TR is trivial and due to pulmonary hypertension, or it may be medium-pitched if TR is severe and has other causes. When the murmur is not present at all, the diagnosis is best made by the appearance of the jugular venous wave pattern and the presence of hepatic systolic pulsations.
Where to hear tricuspid regurgitation?
When evident, it is a holosystolic murmur heard best at the left middle or lower sternal border or at the epigastrium with the bell of the stethoscope when the patient is sitting upright or standing. The murmur may be high-pitched if TR is trivial and due to pulmonary hypertension, or it may be medium-pitched if TR is severe and has other causes. When the murmur is not present at all, the diagnosis is best made by the appearance of the jugular venous wave pattern and the presence of hepatic systolic pulsations. The murmur varies with respiration, becoming louder with inspiration (Carvallo sign).
Where is the heart murmur heard?
Heart sounds include a holosystolic murmur heard best at the left middle or lower sternal border or at the epigastrium when the patient is sitting upright or standing; the murmur becomes louder with inspiration. TR is usually well tolerated, but severe cases may require annuloplasty, valve repair, or valve replacement.
What is TR in heart?
Tricuspid regurgitation (TR) is insufficiency of the tricuspid valve causing blood flow from the right ventricle to the right atrium during systole. The most common cause is dilation of the right ventricle. Symptoms and signs are usually absent, but severe TR can cause neck pulsations, a holosystolic murmur, and right ventricular–induced heart failure or atrial fibrillation. Diagnosis is by physical examination and echocardiography. TR is usually benign and does not require treatment, but some patients require annuloplasty or valve repair or replacement.
Can tricuspid regurgitation cause neck pulsations?
Tricuspid regurgitation usually causes no symptoms, but some patients experience neck pulsations due to elevated jugular pressures. Symptoms of severe TR include fatigue, abdominal bloating, and anorexia. Patients may also develop symptoms of AF or atrial flutter.
Can TR cause neck pulsations?
Symptoms and signs are usually absent, but severe TR can cause neck pulsations, a holosystolic murmur, and right ventricular–induced heart failure or atrial fibrillation. Diagnosis is by physical examination and echocardiography.
Is RV regurgitation a decompensation?
However, in contrast to left-sided valvular regurgitation, there is no robust way to discern when the RV is starting to decompensate. Given this, patients are commonly referred late for surgery. In the context of the significant risks of surgery the overall outcome is poor.
Is a murmur high or medium?
The murmur may be high-pitched if TR is trivial and due to pulmonary hypertension, or it may be medium-pitched if TR is severe and has other causes. When the murmur is not present at all, the diagnosis is best made by the appearance of the jugular venous wave pattern and the presence of hepatic systolic pulsations.
What is diastolic murmur?
A diastolic murmuris a sound of some duration occurring during diastole. All diastolic murmurs imply some alteration of anatomy or function of the cardiovascular structures. The four most commonly encountered diastolic murmurs include aortic and pulmonary valve regurgitation, and mitral and tricuspid valve rumbles (Table 27.1). Compared to most systolic murmurs, diastolic murmurs are usually more difficult to hear, and certain auscultatory techniques are essential for their detection.
What is a murmur of pulmonary valve regurgitation?
The murmur of pulmonary valve regurgitationassociated with pulmonary hypertension is an early diastolic, decrescendo murmur beginning with the pulmonary component of the second sound, best heard along the upper left sternal border. Auscultatory techniques are like those for aortic regurgitation. The quality of pulmonary valve regurgitation is similar to that of aortic regurgitation, and differentiation may be difficult. The murmur of pulmonary valve regurgitation may increase in intensity with inspiration. In association with mitral regurgitation, intensity may actually decrease with inspiration. The presence of bounding pulses and a wide pulse pressure support the diagnosis of aortic regurgitation. Pulmonary valve regurgitation frequently results from severe pulmonary hypertension. When the murmur is associated with mitral stenosis and pulmonary hypertension, it usually represents trivial aortic regurgitation simply because aortic regurgitation is more common than pulmonary valve regurgitation in this clinical setting.
What causes aortic valve regurgitation?
Aortic valve regurgitationis the result of a loss of perfect apposition of the aortic cusps in diastole. There may be deformity of the cusps or the supporting structures. The problem may develop gradually, as in rheumatic heart disease, or acutely, as in bacterial endocarditis. The symptoms and physical findings depend on the severity of the regurgitation and the duration of its development. A minimal regurgitant volume causes no abnormalities other than the presence of the murmur. The regurgitant volume increases diastolic filling of the left ventricle, and as this gradually progresses, there is an increase in stroke volume, left ventricular dilatation, and hypertrophy. The peripheral pulses are hyperdynamic, and the pulse pressure is widened. An apical diastolic rumble (Austin-Flint) may be heard at the apex. This is due to partial closure of the anterior leaflet of the mitral valve. The apex impulse becomes laterally displaced and sustained. Resting and exercise cardiac output is maintained until progressive left ventricular dilatation causes impairment of myocardial function. Easy fatigue and dyspnea ensue. Severe left ventricular dilatation causes inadequate apposition of the mitral leaflets, and a murmur of mitral regurgitation is heard. As left ventricular diastolic pressure increases and is reflected into the left atrium and pulmonary veins, eventual pulmonary hypertension, right ventricular dilatation, tricuspid regurgitation, and elevated jugular venous pressure develop. The presence of a widened pulse pressure, a murmur that continues throughout diastole, and an apical diastolic rumble (Austin-Flint rumble) imply significant aortic regurgitation even before the development of pulmonary hypertension and right heart failure.
How to hear a rumble in the mitral valve?
A mitral valve rumbleis a diastolic murmur of low frequency occurring in middiastole and/or late diastole (presystole). It is frequently localized to a small area at the apex impulse. The patient should be relaxed in a left lateral decubitus position and the apex impulse localized. The bell of the stethoscope should be applied with very lightpressure, just enough to make contact with the skin. Concentrate on diastole and move the bell over and just adjacent to the apex impulse. Listen in middiastole and just before the first sound. If the murmur is due to mitral stenosis, there may be accentuation of the first sound and an opening snap. The opening snap is a high-frequency sound that introduces the middiastolic component of the rumble and occurs .03 to .14 second after the second sound. Maneuvers that transiently increase cardiac output, such as sit-ups, coughing, or squatting, may aid in detection. When the apex impulse is not easily located, scanning the area, listening for the point of maximum intensity of the heart sounds, can help identify the apex impulse and the area on which to concentrate for the mitral diastolic rumble.
Where is the murmur of aortic regurgitation heard?
It is usually a high-frequency, "blowing" sound, most often heard best along the left lower sternal border, although occasionally only in the second right intercostal space. It may be of maximum intensity along the right sternal border (see discussion later in this chapter). Rarely, the murmur may be isolated at the apex impulse.
What is the result of a cusp apposition?
Pulmonary valve regurgitationis the result of imperfect cusp apposition resulting from deformity of the cusps or the supporting structures. It is most frequently secondary to severe pulmonary hypertension with dilatation of the supporting structures. In such cases, the regurgitant volume is small and of no hemodynamic importance. Pulmonary valve regurgitation may also occur with normal pulmonary artery pressures. In such cases, even a large regurgitation volume is usually well tolerated by the right ventricle. There is right ventricular dilatation and elevation of the jugular venous pressure. Rarely will severe right heart failure develop.
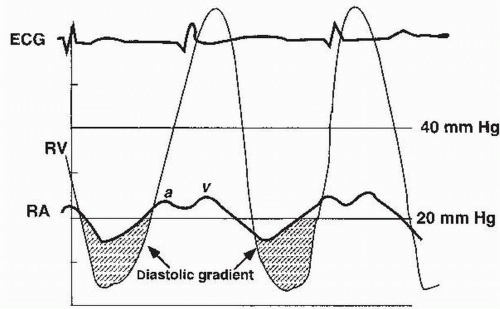
Where is the tricuspid valve rumble located?
A tricuspid valve rumblehas similar characteristics as the mitral rumble, but is localized along the left lower sternal border and increases in intensity with inspiration. The bell should be placed, again with very lightpressure, exploring from the third to the fifth interspaces, concentrating in diastole both during inspiration and expiration. Similar maneuvers to increase venous return may augment the murmur. The inspiratory accentuation aids in differentiation from the mitral rumble, although the latter does not usually radiate to the left sternal border. Accentuation of the first sound (tricuspid component) and a tricuspid opening snap may also be present. The presystolic component of the tricuspid valve rumble is often crescendo—decrescendo, unlike the crescendo pattern of the mitral rumble.
What is a tricuspid murmur?
1. Tricuspid regurgitation murmur shares all the features listed under the general characteristics of regurgitant murmurs. In general it is high in frequency and blowing in quality and usually lasts all the way to S2.
Where is tricuspid regurgitation loud?
5. Irrespective of the etiology, tricuspid regurgitation murmurs are maximal in loudness over the xiphoid area and over the lower sternal region. In addition, tricuspid regurgitation murmur will typically increase in intensity or loudness on inspiration ( Carvallo's sign) (6). It may be heard over the apex area if the right ventricle is enlarged or dilated and has taken over the apex area.
Why is the murmur so short?
The murmur may vary in length, early systolic to being holo- or pansystolic. When the regurgitation is associated with normal right ventricular pressures, the murmur is often soft and short with low to medium frequencies and confined to the early half of systole (99). The intensity often diminishes toward the end of systole because the right atrial v wave and the rising right ventricular systolic pressures tend to equalize toward the end of ejection. This will cause the regurgitant flow to diminish in later systole. The inadequacy ofthe right ventricular function may also produce a poor inspiratory increase in its stroke volume. This may, therefore, result in a poor inspiratory increase in the intensity of the murmur.
Is tricuspid regurgitation present on Doppler?
8. The audibility of tricuspid regurgitation murmur is often variable. Sometimes significant tricuspid regurgitation may be present on the Doppler, and yet the associated murmur may be absent. This is more likely when the right ventricular systolic pressures are normal. Jugular venous pulse contour may sometimes be characteristic of tricuspid regurgitation, and yet the murmur may be inconspicuous. While the X descent may be visible with mild and occasionally mild-to-moderate tricuspid regurgitation on the Doppler, significant tricuspid regurgitation will usually lead to the loss of the normal X descent in the jugulars. In addition, the typical fast-rising large-amplitude v wave followed by the y descent will reveal the tricuspid regurgitation. In Ebstein's anomaly, the huge right atrium, because of partial atrialization of the right ventricle and the resultant high capacitance effect of the right atrium, may sometimes hide the presence of tricuspid regurgitation in the jugulars, and the jugular pulsations may in fact be quite unimpressive in such patients.
What is the diastolic murmur of pulmonary regurgitation?
The diastolic murmur of pulmonary regurgitation is very similar to the one of aortic regurgitation. It is a decrescendo diastolic murmur with a blowing character. However, contrary to the one of aortic regurgitation, this murmur is loudest at the left upper sternal border, around the 2 nd and 3 rd intercostal spaces. Because of their similarity, it can be very difficult to differentiate between these two murmurs relying on auscultation alone. The key differential element is the presence of a peripheral arterial bounding pulse, that only patients with aortic regurgitation will demonstrate.
What is a diastolic murmur?
Diastolic murmurs are always a pathological finding on the auscultation of the heart, indicating the presence of a valvular abnormality. The physical exam can, by itself, reveal the cause of a diastolic murmur. However, it is very important to perform the physical exam with the right technique in order to maximize our chances to identify ...
What causes a continuous murmur?
We will briefly describe two of the most common causes of a continuous murmur, that are the patent ductus arteriosus and pericarditis.
How does aortic regurgitation affect blood pressure?
In a patient with aortic regurgitation there is an increase in the differential blood pressure (systolic blood pressure – diastolic blood pressure). This is caused by both an increase in the SBP, secondary to a greater stroke volume, and also by a reduction of the DBP as a consequence of the regurgitant blood flow during diastole. The increased differential pressure manifests as a bounding arterial pulse that can be appreciated basically at any artery around the body. For this reason, there are many different peripheral signs of aortic regurgitation, based on the specific artery considered. The most famous ones are the Corrigan’s pulse, visible at the carotids, and the Water-Hammer pulse, that can be observed at the wrists.
Why does the ductus arteriosus close?
Normally it closes right after birth when the pressure in the pulmonary circulation increases. However, if the ductus arteriosus stays open it will be possible to appreciate a continuous murmur that is loudest at the left infraclavicular area. This murmur is continuous since the blood pressure in the aorta is higher than the pressure in the pulmonary artery both during systole and during diastole. This allows for a continuous blood flow across the defect.
What causes mitral stenosis?
Other less frequent causes of mitral stenosis are atrial myxoma, calcific annular degeneration of the mitral valve and congenital causes , which are seen mostly in the pediatric population.
Where to hear tricuspid stenosis murmur?
The murmur of tricuspid stenosis is heard best at the left lower sternal border using the bell of the stethoscope, similarly to the murmur of mitral stenosis. Also, we can increase the intensity of the tricuspid stenosis murmur by asking the patient to take a deep breath, thus increasing the blood flow to the right side of the heart and across the stenotic valve. Lastly, in isolated tricuspid stenosis there will be a fixed split S1, secondary to the delayed closure of the stenotic tricuspid valve.
What is a late diastolic murmur?
Late diastolic ( presystolic) murmurs start after S2 and extend up to S1 and have a crescendo configuration. They can be associated with AV valve narrowing. They include mitral stenosis, tricuspid stenosis, myxoma, and complete heart block.
What is the difference between a mid diastolic and a late diastolic murmur?
Mid-diastolic murmurs start after S2 and end before S1. They are due to turbulent flow across the atrioventricular (mitral & tricuspid) valves during the rapid filling phase from mitral or tricuspid stenosis. Late diastolic ( presystolic) murmurs start after S2 and extend up to S1 and have a crescendo configuration.
What is Austin Flint murmur?
An Austin Flint murmur is usually associated with significant aortic regurgitation. Pulmonary regurgitation is most commonly due to pulmonary hypertension ( Graham-Steell murmur ). It is a high-pitched and blowing murmur with a decrescendo configuration.
What causes diastolic murmurs to end before S1?
Common causes include aortic or pulmonary regurgitation and left anterior descending artery stenosis.
What is the name of the heart murmur that starts at S2?
Auscultogram from normal and abnormal heart sounds. Diastolic heart murmurs are heart murmurs heard during diastole, i.e. they start at or after S2 and end before or at S1. Many involve stenosis of the atrioventricular valves or regurgitation of the semilunar valves .
Where is the aortic murmur heard?
Aortic regurgitation. The murmur is low intensity, high-pitched, best heard over the left sternal border or over the right second intercostal space , especially if the patient leans forward and holds breath in full expiration. The radiation is typically toward the apex.
Does Dock's murmur extend to S1?
The murmur usually does not extend to S1. Early diastolic. Left anterior descending artery stenosis. This murmur, also known as Dock's murmur, is similar to that of aortic regurgitation and is heard at the left second or third intercostal space. A Coronary artery bypass surgery can eliminate the murmur.
