Initial antibiotic therapy for critically ill patients before cultures and sensitivities: Ampicillin + gentamicin This medication is used to treat minor skin infections or minor infections related to some skin conditions. This medication is a rifamycin antibiotic used to prevent and treat tuberculosis and other infections.Gentamicin
Rifampin
Endocarditis
Infection of the endocardium, usually involving heart valves.
Who is at risk for infective endocarditis?
There are four main groups of people who are at risk for infective endocarditis. People with underlying heart problems such as congenital heart disease, valvular heart disease, hypertrophic cardiomyopathy, rheumatic heart disease, or previous bouts of endocarditis. People who have undergone heart valve repair or replacement, or have had a pacemaker inserted into their chest.
How serious is endocarditis?
This can cause serious damage and infections in the lungs and brain, causing strokes, as well as many other parts of the body, including the kidneys, liver, spleen, and important blood vessels. The infections can be hard to clear and continually seed the bacteria in the blood, leading to a serious, uncontrolled infection.
What is the initial treatment of infective endocarditis (IE)?
Treatment and escalation:
- Take bloods – U&Es, FBC (for Hb) and clotting.
- Consider stopping anticoagulation – depending on the patient’s state and degree of blood loss
- If there is a large Hb drop, do a group and save and call your senior – the patient might need a transfusion. ...
- Check renal function, and if AKI is present, follow your usual treatment protocol.
Do you need antibiotics before dental work with mitral valve prolapse?
In the past, antibiotic prophylaxis before dental work was recommended for the majority of patients with mitral valve prolapse, but that is no longer the case. Nowadays, medical professionals generally advise against antibiotics before dental treatment if you have the condition.

What antibiotics are used for prophylaxis?
The three antibiotics used in adult surgical prophylaxis, where weight-based dosing is recommended, are cefazolin, vancomycin, and gentamicin.
What is the drug of choice for prophylaxis to prevent bacterial endocarditis before a dental procedure?
Penicillin is the drug of choice in treating dental infections. Patients at high risk include those with infective endocarditis, immunocompromised conditions and dental procedures which may produce bacteremias. Invasive dental procedures if performed in such patients should be preceded with an antibiotic prophylaxis.
What is the best antibiotic for endocarditis?
Treatment with aqueous penicillin or ceftriaxone is effective for most infections caused by streptococci. A combination of penicillin or ampicillin with gentamicin is appropriate for endocarditis caused by enterococci that are not highly resistant to penicillin.
When do you give prophylaxis for infective endocarditis?
Infective endocarditis prophylaxis for dental procedures should be recommended only for patients with underlying cardiac conditions associated with the highest risk of adverse outcome from infective endocarditis (see “Patient Selection,” in the main text).
What are 5 typical antibiotics used in dentistry?
What Are The Antibiotics Used In Dentistry?Amoxicillin.Azithromycin.Cephalexin.Clindamycin.Penicillin.
How much amoxicillin should i take before teeth cleaning?
The preferred prescription for prophylactic antibiotic treatment is: Amoxicillin 500 mg, 4 tabs, 1 hour prior to procedure/dental cleaning. If allergic to Penicillin then Clindamycin 300 mg, 2 tabs, 1 hour prior.
What is the first line treatment for endocarditis?
First-line treatment: Cefepime 2 g IV q8h for normal renal function. Second-line treatment (if patient is penicillin or cephalosporin intolerant): Aztreonam 2 g IV q8h for normal renal function. Antipseudomonal penicillin plus aminoglycoside recommended if Pseudomonas aeruginosa endocarditis is suspected.
Can you take oral antibiotics for endocarditis?
Patients with endocarditis caused by common bacteria can be treated effectively and safely with oral antibiotics once they have been stabilized on an intravenous course of therapy, data from the POET trial suggest.
Does amoxicillin treat endocarditis?
Oral amoxycillin is effective in uncomplicated streptococcal endocarditis, and should not be used with prosthetic valve infections.
When is antibiotic prophylaxis required?
According to these guidelines, antibiotic prophylaxis should be considered for people with: Artificial heart valves. A history of an infection of the lining of the heart or heart valves known as infective endocarditis, an uncommon but life-threatening infection.
When should prophylactic antibiotics be given?
Prophylactic antibiotic administration should be initiated within one hour before the surgical incision, or within two hours if the patient is receiving vancomycin or fluoroquinolones. The goal of antibiotic prophylaxis is to ensure effective serum and tissue levels of the drug for the duration of the surgery.
What is bacterial endocarditis prophylaxis?
Endocarditis prophylaxis seeks to prevent IE by administering antibiotics to high-risk patients when they undergo procedures that can induce bacteremia.
What is a dental prophylaxis in dentistry?
A dental prophylaxis is a cleaning procedure performed to thoroughly clean the teeth. Prophylaxis is an important dental treatment for halting the progression of periodontal disease and gingivitis.
What is IE in medical terms?
Infective endocarditis (IE) is an uncommon disease but has devastating consequences; a significant proportion of patients develop heart failure or stroke or require valve surgery, with high in-hospital and 6-month mortality approximating 20% and 30%, respectively. 1 Because of the significant morbidity and mortality, recommendations for preventative strategies were developed as early as the 1950s. Recommendations were based on animal models of IE along with in vitro susceptibilities of microorganisms known to cause endocarditis. Amoxicillin has been shown to have a significant impact on the incidence and duration of bacteremia after dental procedures. 2 However, clinical evidence for endocarditis prevention is lacking, and there has never been a randomized controlled trial to determine whether antibiotic administration prevents IE. Thus, these recommendations were not strictly evidence-based but rather expert consensus that prevention in at-risk patients is a better strategy than treatment of a disease with high morbidity and mortality.
What are the limitations of Garg et al?
First, there is no International Classification of Diseases code specific to viridans group Streptococcus, the organism most likely to be affected by AP. Second, microbiological data were missing in 26% of cases. Third, as with all ecological studies, causal relationships cannot be established.
How long after the IE revision did the hospitalization increase?
Garg et al 13 concluded that the increase in hospitalizations because of IE that occurred in both groups 3 years after guideline revision was not likely related to the change in guideline recommendation, because (1) the increase did not occur until 3 years after the guideline revision; (2) the increase occurred in both high- and moderate-risk groups and not just the moderate-risk group, for whom AP recommendations changed; and (3) the relative proportion of streptococcal IE versus staphylococcal IE decreased, at least in the younger adult population, over time.
Why is the streptococcus to staph ratio the same over time?
Importantly, the finding that the Streptococcus to Staphylococcus ratio remained the same over time among older individuals raises concern, particularly because the authors found that comorbidities that increase healthcare contact and risk for Staphylococcus infection increased over time.
How much has AP decreased?
For example, investigators in North America have found a 64% decrease in AP prescriptions in moderate-risk patients and a significant 20% decrease even in high-risk patients. 7
When did Garg et al 13 perform a cross sectional time series analysis?
In this issue of Circulation, Garg et al 13 add to a growing body of epidemiological data by performing a population-based, cross-sectional time series analysis in adults at moderate and high risk for IE between 2002 and 2014 in Ontario, Canada, to assess for differences in AP prescribing practices and IE incidence. In adults ≥65 years of age, they found that AP decreased significantly in the moderate-risk group for IE after the changes to guideline recommendations, with no significant change in AP prescriptions in the high-risk group.
What should be included in future studies?
Future studies should ideally include granular data on underlying cardiac conditions and devices, invasive dental exposures within a predefined time period, whether the patients received AP, and the microbial pathogenesis of the incident IE cases, focusing on microorganisms specifically targeted by AP. Electronic health records may provide an opportunity for a large pragmatic clinical trial to prospectively assess these important factors.
What Are Antibiotic Prophylactic Regimens for Endocarditis?
People at risk for this infection receive prophylactic antibiotics before medical and dental procedures to stop a potential infection.
How Is Endocarditis Diagnosed?
Endocarditis is diagnosed with a history and physical exam, which will include the healthcare professional listening to the heart with a stethoscope to detect a heart murmur, which can be a sign of endocarditis.
What Is the Treatment for Endocarditis?
Endocarditis is usually treated in a hospital with intravenous antibiotics.
How often should I take vancomycin?
For patients with gram-positive cocci in clusters found on gram stain, monotherapy with empiric vancomycin every 8 to 12 hours dosed to maintain a concentration of 15 to 20 mg/kg is appropriate. When cultures and sensitivities are available, antibiotics coverage should be narrowed. If the patient is found to have methicillin-sensitive endocarditis, then nafcillin or oxacillin dosed up to 12g per day divided dosed every four to six hours. Vancomycin has less effective bactericidal action than penicillin or beta-lactamase-based therapies. As such, it should be limited to patients with severe reactions to PCN or beta-lactamase or patients with MRSA. In patients who have methicillin-resistant staph aureus, monotherapy with vancomycin 30mg/kg or daptomycin 6 to 10mg/kg is the treatment of choice. Historically, combination therapy using a beta-lactam with an aminoglycoside was formerly the treatment of choice. However, aminoglycosides in combination with vancomycin have increased the risk of nephrotoxicity and ototoxicity while providing minimal to no survival benefit. As such, the American Heart Association now discourages concomitant aminoglycoside use with vancomycin for use in MRSA.
What is the best antibiotic for native valve endocarditis?
Empiric antimicrobial therapy in native valve endocarditis targets the three most common pathogens: staphylococcus, streptococcus, or enterococci.[5] Critically ill patients may require more intensive antibiotic therapy such as ampicillin with gentamicin and flucloxacillin, or oxacillin can be used empirically in severely ill patients with native valve endocarditis or late PVE.[6] Antibiotic therapy should undergo adjustment as gram stain, culture, and susceptibilities become available. Native valve endocarditis treatment typically requires 2 to 6 weeks of antibiotics.
What is the best way to select antibiotics?
Selection of appropriate antibiotic regimens requires an interprofessional team approach involving physicians and nurses (particularly those with specialized infectious disease backgrounds), pharmacists, and primary care physicians. Further, consultation and coordination with an infectious disease specialist are usually necessary. [Level 5] Empirical antibiotic therapy is recommended if the suspicion of endocarditis is high; once culture results are obtained, the antibiotic selection can target the sensitivity of the organism.
What is the best team for antibiotic management?
Management of antibiotic regimens for infective endocarditis is best achieved with an interprofessional team involving physicians, infectious disease experts, specialty-trained nursing staff, and pharmacists all collaborating to manage the cases to an optimal patient outcome. [7][8][Level 5]
How often does endocarditis occur?
Endocarditis is an uncommon infection occurring every 3 to 7 per 100000 person-years. Yet, it is also the fourth most common life-threatening infection after sepsis, pneumonia, and intraabdominal abscess, with an estimated inpatient mortality rate between 15 to 30%. When endocarditis was first widely studied in the 1960s, streptococcus viridian was the most commonly identified pathogen. However, the epidemiology has shifted, with Staphylococcus aureus being the most frequently identified pathogen. While this shift is partially attributable to an increased rate of intravenous drug abuse in North America, the healthcare-associated infection has become increasingly common, representing about 30% of all endocarditis cases.
How to manage endocarditis?
The management of endocarditis requires an interprofessional approach by infectious disease, cardiology, and cardiac surgery to manage antimicrobial therapy and assess for possible surgical intervention.[1] Early consultation with cardiothoracic surgery has been shown to improve mortality and is mandatory in patients presenting with complications. Approximately 50% of patients with endocarditis will require some form of surgical intervention.[2] According to the American Heart Association recommendation, a consult with an infectious disease expert should occur before initiating empiric antibiotic therapy due to the many nuances associated with treating endocarditis. Vegetations contain densely packed bacteria interlocked within a biofilm composed of fibrin and platelets, which creates a mechanical barrier limiting antibiotic penetration. Each antibiotic class has differing pharmacological properties which influence the rate of diffusion, distribution, and ability of the antibiotic to penetrate the vegetation, which ultimately determines the bactericidal efficacy. The duration of therapy for successfully eradicating bacteria has its basis in the bactericidal action of the specific antibiotic, minimal inhibitory concentration, pathogen, vegetation burden, and area of involvement. The duration of treatment can range from 2 to 6 weeks.
How long does endocarditis last after valve replacement?
Late endocarditis occurs one year or longer after valve replacement. It typically results from organisms similar to those found in native valve endocarditis.
What is the ADA extension number?
ADA members may use the Association’s toll-free number (1-800-621-8099) and ask for extension 2878. The most current guidelines for prophylaxis against IE can be found by clicking on the following link: http://www.ada.org/prof/resources/topics/infective_endocarditis_guidelines.pdf.
What are the risks of taking prophylactic antibiotics?
The risks include: . Adverse reactions to antibiotics ranging from mild to death. The development of drug-resistant bacteria.
What is Osler's node?
Osler’s nodes: tender, red , raised lesions on the hands or feet
Can you take antibiotics before dental treatment?
It has long been recommended that patients with certain heart conditions take antibiotics before dental treatment to prevent Subacute Bacterial Endocarditis, now known as infective endocarditis (IE).
Is prophylaxis recommended after dental surgery?
Only patients at the greatest risk of a bad outcome if they were to develop IE after a dental procedure are covered by the new recommendations, and for these patients, prophylaxis is recommended for all procedures that involve manipulation of the gingiva (including cleaning) or the periapical region of the teeth, or that involve the perforation of the oral mucosa (except anesthetic injections through non-infected tissue).
Do dental clinics have to download the legal sidebar?
It is recommended that every dental clinic download a copy of the recommendations and the legal sidebar and keep them in a readily accessible area of the clinic for quick reference.
Who Might Benefit from Antibiotic Prophylaxis?
Antibiotic prophylaxis is recommended for a small number of people who have specific heart conditions. The American Heart Association has guidelines identifying people who should take antibiotics prior to dental care. According to these guidelines, antibiotic prophylaxis should be considered for people with:
What is an artificial heart valve?
Artificial heart valves. A history of an infection of the lining of the heart or heart valves known as infective endocarditis, an uncommon but life-threatening infection. A heart transplant in which a problem develops with one of the valves inside the heart. Heart conditions that are present from birth, such as:
What to do if playback doesn't begin?
If playback doesn't begin shortly, try restarting your device.
Do you need antibiotics for artificial joints?
Learn more about why the ADA and American Association of Orthopedic Surgeons updated the recommendations and no longer recommend antibiotics for everyone with artificial joints.
Do you take antibiotics before dental surgery?
At times physicians and dentists recommend that a patient take antibiotics before certain dental procedures. This is called “antibiotic prophylaxis.”. But why do healthcare providers suggest this extra step?
Can bacteria enter the bloodstream?
We all have bacteria in our mouths, and a number of dental treatments—and even daily routines like chewing, brushing or flossing—can allow bacteria to enter the bloodstream (bacteremia). For most of us, this isn’t a problem. A healthy immune system prevents these bacteria from causing any harm.
What is IE in healthcare?
All healthcare team members should be diligent in considering the possibility of IE in at-risk patients as early treatment will improve outcomes. As mentioned above, subacute bacterial endocarditis prophylaxis requires close monitoring and communication, and follow-up monitoring requires coordination between clinicians, specialists, nurses, specialty-trained nurses, dentists, and pharmacists. In summary, an interprofessional team approach for the patients will translate to better patient outcomes, maximize efficacy and minimize adverse drug reactions. [Level 5]
What is the difference between acute and subacute bacterial endocarditis?
There are several differences between subacute bacterial endocarditis and acute bacterial endocarditis. Most cases of subacute bacterial endocarditis are caused by penicillin-sensitive Streptococcus viridans, while Staphylococcus aureus causes most cases of acute bacterial endocarditis.[3] Subacute bacterial endocarditis mostly happens in pre-existing heart disease, while acute bacterial endocarditis mostly happens in healthy hearts. After treatment, subacute bacterial endocarditis rarely leads to severe cardiac damage; however, most patients who survive acute bacterial endocarditis often die of cardiac failure within weeks or months. [3]
What is IE in medical terms?
Infective endocarditis (IE) is an infection of the endocardial surfaces of the heart, which includes one or more heart valves. The incidence of infective endocarditis hospitalization in the United States is estimated at 12.7 per 100,000 annually. A majority of the patients (57.7%) are male, and more than a third are 70 years and older. Several risk factors predispose patients to IE, such as structural heart disease (valvular disease or congenital heart disease), prosthetic heart valves, indwelling cardiovascular device, an intravascular catheter, chronic hemodialysis, human immunodeficiency virus infection, diabetes, or history of infective endocarditis. Other risk factors include males older than 60 years, male gender, intravenous (IV) drug use, poor dentition, or dental infection. Infective endocarditis may present as acute or subacute infection. Acute infections present as a rapidly progressive disease with high fevers, rigors, and sepsis. On the other hand, subacute bacterial endocarditis diagnosis is often delayed and presents with non-specific symptoms such as weight loss, fatigue, dyspnea over several weeks to months. There are several differences between subacute bacterial endocarditis and acute bacterial endocarditis. Most cases of subacute bacterial endocarditis are caused by penicillin-sensitive Streptococcus viridans, while Staphylococcus aureus causes most cases of acute bacterial endocarditis. Subacute bacterial endocarditis mostly happens in pre-existing heart disease, while acute bacterial endocarditis mostly happens in healthy hearts. After treatment, subacute bacterial endocarditis rarely leads to severe cardiac damage; however, most patients who survive acute bacterial endocarditis often die of cardiac failure within weeks or months. This activity reviews the prophylaxis of subacute endocarditis and highlights the role of the interprofessional team approach.
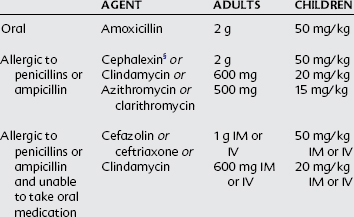
What antibiotics are used for dental procedures?
For dental and respiratory procedures, the most common bacteria are the various Streptococcus viridansspecies. The recommended prophylactic antibiotic is amoxicillin 2 grams orally 1 hour before the procedure. If the patient needs intravenous (IV) medication, ampicillin or ceftriaxone may be used. Cephalexin or azithromycin may be used in patients with a penicillin allergy. [There is new penicillin resistance of theStreptococcus viridian; therefore, the prescribing physician must consider the resistance in their practice area when prescribing the appropriate antibiotic. In cases where Staphylococcus aureusis suspected, antistaphylococcal penicillin or vancomycin is recommended.
What is dental procedure?
Dental procedures involve manipulation of gingival tissue, manipulation of the periapical region of teeth, or perforation of the oral mucosa. This does not include routine anesthetic injections through noninfected tissue, dental radiographs, placement or adjustment of orthodontic devices, or trauma to the lips and teeth. [4][6]
Is prophylaxis recommended for tonsillectomy?
The 2007 AHA guidelines also recommended prophylaxis for invasive respiratory tract procedures that involve incision or biopsy of the respiratory mucosa (e.g., tonsillectomy, adenoidectomy). Antibiotic prophylaxis has not been recommended for bronchoscopy unless the procedure involves an incision of the respiratory tract mucosa. [4]
What is NCBI bookshelf?
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Is antibiotic prophylaxis unwarranted?
In the following examples, the guidance has been that antibiotic prophylaxis is unwarranted unless the person is predisposed, for some reason, to infection, in which case, it may be appropriate for the treating physician to prescribe the antibiotic. ADA member inquiries have included questions regarding indications such as artificial joint replacement, 2, 5 solid organ transplant, 15 breast augmentation with implants, 15 or penile implant. 16, 17 The National Institute of Dental and Craniofacial Research recommends that in patients receiving chemotherapy who have a central venous catheter, dental professionals consult the treating oncologist about the need for antibiotic prophylaxis before any dental procedures. 18
Can you give antibiotics prior to dental surgery?
With the exception of the AHA/ACC guidelines regarding prevention of infective endocarditis, 7, 8, 10 there is no general guidance or recommendation to provide antibiotics as a prophylactic measure prior to dental procedures except for specific individuals with extenuating circumstances, where the determination and prescription is made by the patient’s surgeon or other treating physician. However, there are a myriad of other conditions that either patients, physicians, or dentists may think that antibiotic prophylaxis prior to dental treatment might be warranted to prevent development of infections at remote locations by bacteria normally associated with the oral flora.
Is there a correlation between antibiotic prophylaxis and endocarditis?
In 2015, The Lancet published a study out of the United Kingdom that reported a correlation between institution of more limited antibiotic prophylaxis guidelines by the National Institute for Health and Clinical Evidence (NICE) in 2008 and an increase in cases of infective endocarditis. 13 Because of the retrospective and observational nature of the study, the authors acknowledged that their “data do not establish a causal association.” At this time, the ADA recommends that dentists continue to use the AHA/ACC guidelines discussed above. Dental professionals should periodically visit the ADA website for updates on this issue.
Do you have to premedicate for antibiotic prophylaxis?
Sometimes, patients forget to premedicate before their appointments. The recommendation is that for patients with an indication for antibiotic prophylaxis, the antibiotic be given before the procedure. This is important because it allows the antibiotic to reach adequate blood levels. However, the guidelines to prevent infective endocarditis 7, 8 state, “If the dosage of antibiotic is inadvertently not administered before the procedure, the dosage may be administered up to 2 hours after the procedure.” If a patient with an indication for prophylaxis who appropriately received antibiotic premedication prior to a dental procedure one day and who is then scheduled the following day for a dental procedure also warranting premedication (e.g., dental prophylaxis), the antibiotic prophylaxis regimen should be repeated prior to the second appointment. Because of the nature of the pharmacokinetics of an antibiotic prophylaxis regimen, a single loading dose is given in order to cover the period of potential bacteremia produced by a single procedure. 11-13
Can antibiotics be given to children?
Beyond identifying the specific patient population for whom antibiotic prophylaxis is appropriate, special consideration should be given to the antibiotic dose prescribed to children, as it will vary according to the child’s weight. Weight-based regimens for children are outlined in Table 2 of the 2007 American Heart Association guidelines and Table 5 of the 2021 AHA scientific statement. 7-9 As with any medication, check with the primary caregiver to determine whether the child has an allergy to antibiotics or other antibiotic-related concerns before prescribing.
Is antibiotic prophylaxis recommended for congenital heart disease?
b Except for the conditions listed above, antibiotic prophylaxis is no longer recommended for any other form of congenital heart disease.
Is endocarditis prophylaxis premedication?
For infective endocarditis prophylaxis, American Heart Association guidelines (updated with a scientific statement in 2021) support premedication for a relatively small subset of patients. This is based on a review of scientific evidence, which showed that the risk of adverse reactions to antibiotics generally outweigh the benefits of prophylaxis for many patients who would have been considered eligible for prophylaxis in previous versions of the guidelines. Concern about the development of drug-resistant bacteria also was a factor.
