Medication
Over-the-counter (OTC) oral antibiotics are not approved in the U.S. A bacterial infection is best treated with a prescription antibiotic that is specific for the type of bacteria causing the infection. Using a specific antibiotic will increase the chances that the infection is cured and help to prevent antibiotic resistance.
Procedures
Rarely, if bacteria gets into peritoneal dialysis equipment used to treat people with kidney failure, this can cause infection. If you're diagnosed with peritonitis, you'll need treatment in hospital to get rid of the infection. This might take 10 to 14 days.
Nutrition
Using the layman’s definition that an antibiotic is an antibacterial drug, you can treat most bacterial infections but there are some resistant strains of bacteria, such as MRSA, and some bacterial infections that aren’t worth treating. There are also some bacteria that aren’t resistant per se but aren’t susceptible to most antibiotics.
Specialist To Consult
- Consistent efficacy of rifaximin in treatment trials.
- Durable response after cessation of rifaximin therapy.
- No side effects with rifaximin, unlike other IBS therapies such as tricyclic antidepressants.
- No demonstrable absorption.
- Not needed to treat systemic life-threatening infections.
Are bacterial infections treated with antibiotics?
How long does peritonitis last?
Can antibiotics cure bacterial infections?
What antibiotic is used for intestinal bacterial infection?
What is the best antibiotic for peritonitis?
Cefotaxime is effective against 98% of causative organisms and is considered the treatment drug of choice.
Can peritonitis be cured with antibiotics?
Peritonitis treatment usually involves antibiotics and, in some cases, surgery. Left untreated, peritonitis can lead to severe, potentially life-threatening infection throughout your body.
How is bacterial peritonitis treated?
Individuals with secondary bacterial peritonitis should undergo surgical intervention of the perforated viscus or drainage of the abscess and should be treated with broad-spectrum antibiotics, such as third-generation cephalosporins, with the addition of an antimicrobial agent that has good anaerobic coverage, such as ...
How do you confirm peritonitis?
Peritonitis is often diagnosed by analyzing a sample of the infected fluid taken from the belly (abdomen). Other tests for peritonitis may include: X-rays. Imaging tests that make pictures of your body's tissues, bones, and organs.
What type of bacteria causes peritonitis?
Escherichia coli, streptococci (mostly pneumococci), and Klebsiella cause most episodes of spontaneous bacterial peritonitis in patients who are not receiving selective intestinal decontamination (Garcia-Tsao 1992).
How quickly does peritonitis develop?
How fast does peritonitis develop? Peritonitis is a medical emergency that requires prompt medical attention, as it develops very rapidly. Upon rupture of the abdominal wall or abdominal organs, the peritoneum can become infected within 24 to 48 hours.
What are 4 signs of peritonitis?
The first symptoms of peritonitis are typically poor appetite and nausea and a dull abdominal ache that quickly turns into persistent, severe abdominal pain, which is worsened by any movement. Other signs and symptoms related to peritonitis may include: Abdominal tenderness or distention. Chills.
How long does it take for antibiotics to work for peritonitis?
If you're diagnosed with peritonitis, you'll need treatment in hospital to get rid of the infection. This might take 10 to 14 days. Treatment usually involves being given antibiotics into a vein (intravenously).
Can you have peritonitis for months?
Of the 161 patients, 111 (68.9%) experienced just 1 episode of peritonitis during the study period. The median duration on PD of patients who presented with peritonitis episodes was 34.8 months (range: 15.7 - 56.4 months).
Can peritonitis be treated at home?
Spontaneous bacterial peritonitis can be life-threatening. You'll need to stay in the hospital. Treatment includes antibiotics and supportive care.
What are three causes of peritonitis?
What causes peritonitis?an abdominal wound, such as a surgical wound.an abdominal injury.a ruptured appendix.a stomach ulcer.a perforated colon.diverticulitis.pancreatitis.liver disease, such as cirrhosis of the liver.More items...
Which symptom is often observed in cases of peritonitis?
The diagnosis of peritonitis is a clinical diagnosis, based mostly on history and physical examination. The main symptom in all cases is abdominal pain. The pain can be sharp or insidious; often the pain is constant and intense, and is aggravated with movement.
How long does it take for antibiotics to work for peritonitis?
If you're diagnosed with peritonitis, you'll need treatment in hospital to get rid of the infection. This might take 10 to 14 days. Treatment usually involves being given antibiotics into a vein (intravenously).
Can you survive peritonitis?
Both types of peritonitis are life-threatening. The death rate from peritonitis depends on many factors, but can be as high as 40% in those who also have cirrhosis. As many as 10% may die from secondary peritonitis.
Can you have peritonitis for months?
Of the 161 patients, 111 (68.9%) experienced just 1 episode of peritonitis during the study period. The median duration on PD of patients who presented with peritonitis episodes was 34.8 months (range: 15.7 - 56.4 months).
What are the stages of peritonitis?
Peritonitis can usually be divided into an early formative or absorptive stage during which bacteriemia and bacterial toxemia preponderate, and the fully developed later stage in which circulatory disturbances and inhibition ileus preponderate.
Drugs used to treat Peritonitis
The following list of medications are in some way related to, or used in the treatment of this condition.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
What is the most common etiology of peritonitis?
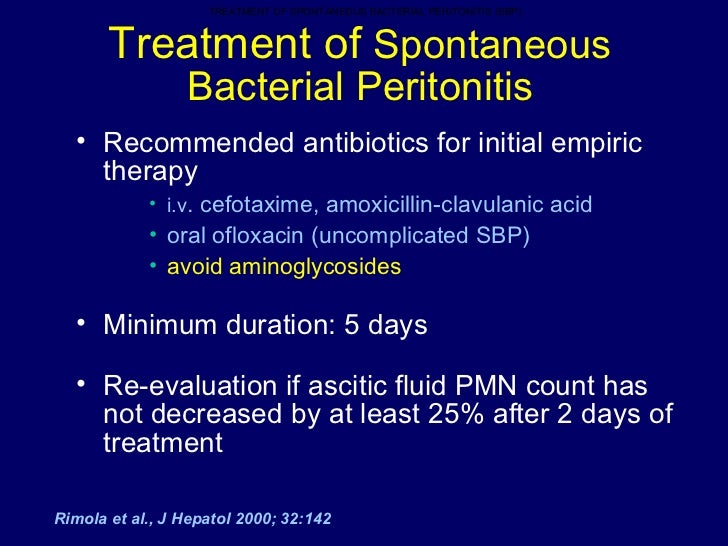
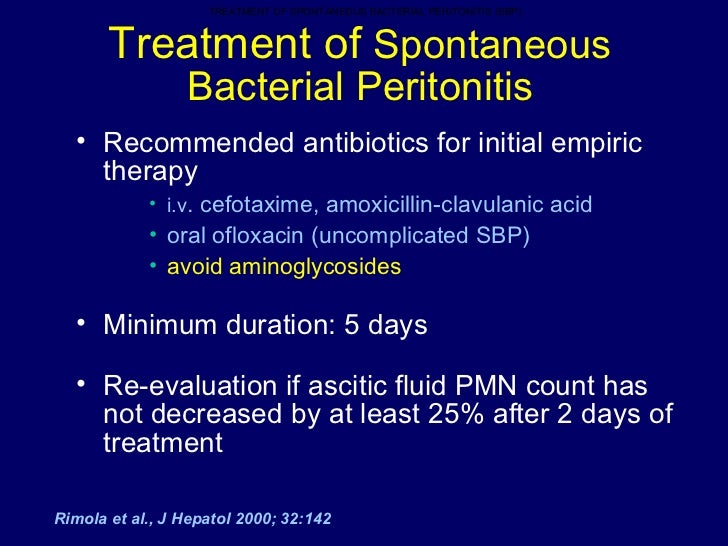
Spontaneous bacterial peritonitis (SBP) resulting from chronic liver disease or nep hritic syndrome with no obvious source of infection is the most common etiology of primary peritonitis. Untreated SBP has a mortality rate of up to 50%, but with prompt diagnosis and treatment of the condition, this figure may be reduced to 20%. Empiric therapy with a third-generation cephalosporin must be started promptly. [ 3] SBP usually does not require any surgical intervention.
What is the choice of antibiotics?
Choice of antibiotics largely depends on whether the infection is community acquired or hospital acquired (nosocomial), the local spectrum of organisms grown and their sensitivity to antibiotics (antibiogram) in similar patients in the near past, costs and side effects of the antibiotics, and comorbidities (especially renal and liver dysfunction) in the patient.
Why do we need antibiotics?
Antibiotic therapy is used to prevent local and hematogenous spread of an intra-abdominal infection and to reduce late complications. [ 1] . Several different antibiotic regimens are available for the treatment of intra-abdominal infections (see Table 1 below). [ 1]
How long should antibiotics be discontinued?
Antibiotics can be discontinued once the clinical signs of infection (eg, fever, tachycardia, leukocytosis) have resolved. Recurrence is a concern with certain infections, such as those with Candida and Staphylococcus aureus, and treatment should be continued for 2-3 weeks. Table 1.
How long does antibacterial therapy last?
Usually, in patients with intra-abdominal infection who have been treated with proper source control and prompt surgical intervention, antibacterial therapy is given for 5-7 days, but this regimen may need to be extended, depending on the clinical situation. [ 1] . Shorter courses also have been used successfully.
Which bacteria are covered by cefotaxime?
Initial coverage should include gram-negative enteric bacteria and gram-positive cocci, which are responsible for 90% of infections. [ 4] Cefotaxime is effective against 98% of causative organisms and is considered the treatment drug of choice. Anaerobic, pseudomonal, and staphylococcal coverage is not needed.
When should antimicrobial therapy be discontinued?
Antimicrobial therapy should continue until signs of infection (eg, fever, tachycardia, leukocytosis) have resolved; if signs of infection continue, persistent infection or the presence of a nosocomial infection should be investigated.
How long should antibiotics be given for peritonitis?
Antibiotics are routinely given for 5–7 days for generalized peritonitis. Antimicrobial agents should be continued until temperature and white blood cell count are within normal limits. Duration of antimicrobial therapy in postoperative peritonitis should not be longer than 7 days. Persistent clinical signs of fever or leukocytosis should prompt a search for a drainable focus of infection in the abdomen or treatable site elsewhere. (Grade A, B and C)
When was peritonitis surgically treated?
Reports on surgical treatment of peritonitis were available at the beginning of the century (Mikulicz 1889; Krönlein 1885; Körte 1892). Kirschner was among the first who demonstrated a reduction in mortality rate by surgical treatment from 80–100% to about 60% in 1926. However, there were doubts that the drainage of the peritoneal cavity is “physical and physiological impossible” (Yates 1905). Since 1926, mortality in peritonitis has decreased to an average of 30–40% with the development of new operative techniques, the introduction of antibiotics and intensive care treatment.
What is secondary bacterial peritonitis?
Secondarybacterial peritonitis describes peritoneal infections secondary to intraabdominal lesions, such as perforation of the hollow viscus, bowel necrosis, nonbacterial peritonitis, or penetrating infectious processes.
What are the signs of peritonitis?
The diagnosis of peritonitis is supported by clinical signs, e.g., abdominal pain and tenderness, nausea, vomiting, diminished intestine sounds, fever, shock, and diagnostic tests, e.g., abdominal x-ray, chest x-ray, ultrasound and CT scan. Ultrasound may be positive in up to 72%, CT in up to 82%. Leukocytes and C reactive protein may be altered but are not direct signs of peritonitis.
What is the difference between sepsis and peritonitis?
Contamination means the presence of bacteria in normal sterile tissue without any host reaction. Infection is the presence of bacteria in normal sterile tissue with local host response (inflammation), clinically evident. Sepsis is the systemic response to local infection. Peritonitis may be caused by traumatic perforation of the bowel, anastomotic dehiscence, translocation of germs, inflammation or perforation of hollow viscus, e.g., appendicitis or colonic diverticulitis.
What is tertiaryperitonitis?
Tertiaryperitonitis, a less well-defined entity, is characterized by persistent or recurrent infections with organisms of low intrinsic virulence or with predisposition for the immunocompromised patient . It usually follows operative attempts to treat secondary peritonitis and is almost exclusively associated with a systemic inflammatory response.
What is the classification of peritonitis?
Peritonitis can be classified into primary, secondary or tertiary peritonitis.
What is the classification of bacterial peritonitis?
Classification of bacterial peritonitis is based upon the source of the infectious bacteria. 2 Primary or spontaneous peritonitis refers to an extraperitoneal etiology, in which the infectious bacteria enter the peritoneal cavity through the circulatory or lymphatic system. 1,2 In these cases, the patient usually has an underlying comorbidity that can lead to bacterial migration into the peritoneum. 1 Such comorbidities may include ascites and indwelling peritoneal dialysis catheters. Primary peritonitis is estimated to occur in 10% to 30% of patients with alcoholic cirrhosis. 1 Additionally, patients on chronic ambulatory peritoneal dialysis (CAPD) have, on average, one incidence of peritonitis every 33 months. 1
How long does it take to get rid of peritonitis?
The recommended duration of treatment is 2 weeks, or 3 weeks for more severe cases. Treatment is dependent on clinical response, which should be seen within 72 hours of initiation of antibiotic therapy. Patients with cloudy effluent after 4 to 5 days of appropriate antibiotic therapy are thought to have refractory peritonitis ...
How often does peritonitis occur?
1 Additionally, patients on chronic ambulatory peritoneal dialysis (CAPD) have, on average, one incidence of peritonitis every 33 months. 1. Secondary peritonitis, the most common etiology, is the result of infectious bacteria from a source within ...
How does peritoneal fluid affect the immune system?
1 This response triggers an inflammatory process, which results in fluid shifts into the peritoneal cavity. This fluid accumulation, along with decreased intestinal motility, often leads to abdominal distention. Additionally, fluid displacement into the abdomen, known as third-spacing , may result in decreased blood volume, leading to hypovolemia in severe cases. Fever, vomiting, and diarrhea may also accompany peritonitis, compounding fluid imbalances and increasing the risk for hypovolemia. Untreated hypovolemia can result in decreased cardiac output, and, ultimately, hypovolemic shock. 1
How long does it take for primary peritonitis to develop?
1 Unlike secondary peritonitis, primary peritonitis may develop over several weeks without any signs of acute distress. Although the patient may complain of abdominal tenderness, nausea, vomiting, or diarrhea, primary peritonitis is usually first suspected when the dialysate appears cloudy in patients undergoing peritoneal dialysis or when encephalopathy worsens in patients with cirrhosis. The laboratory findings following suspicion of primary peritonitis may show mild elevation of the white blood cell (WBC) count and a positive culture of the peritoneal dialysate or ascetic fluid. 1
What was the mortality rate for peritonitis in the 1900s?
Mortality rates associated with peritonitis were around 90% in the early 1900s. These rates have since come down to approximately 30% with the use of appropriate drug therapies and supportive care. 2
What causes peritoneal inflammation?
Conclusion. Peritonitis, an acute inflammation of the peritoneum, can occur due to pathogens or other causes such as chemical exposure. Clinical presentation of primary peritonitis is often nonspecific and may lack initial signs and symptoms.
What is a spontaneous bacterial peritonitis?
Spontaneous bacterial peritonitis (SBP) is defined as an ascitic fluid infection without an evident intra-abdominal surgically treatable source [ 1 ]. The presence of SBP, which almost always occurs in patients with cirrhosis and ascites, is suspected because of signs and symptoms such as fever, abdominal pain, or altered mental status ( table 1 ). (See "Spontaneous bacterial peritonitis in adults: Clinical manifestations" .)
When should antibiotics be given for SBP?
However, antibiotics should not be given until ascitic fluid has been obtained for culture . (See 'Timing' below.)
Classification
Treatment
Prognosis
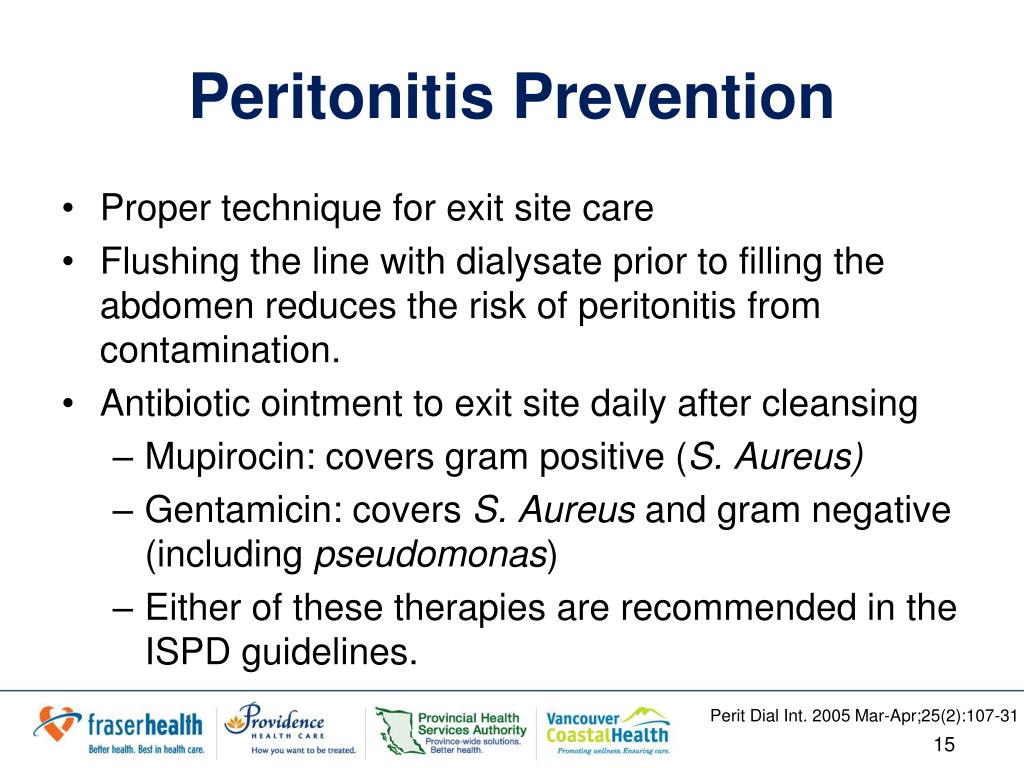
Prevention
Adverse effects
- Peritoneal infections are classified as primary, secondary, or tertiary. Primary peritoneal infections arise from hematogenous dissemination, usually in the setting of an immunocompromised state, while secondary infections are related to a pathologic process in a visceral organ, such as perforation, ischemia and gangrene, trauma, or a postoperative problem, such as anastomotic le…
Causes
- Antibiotic therapy is used to prevent local and hematogenous spread of an intra-abdominal infection and to reduce late complications. [1] Several different antibiotic regimens are available for the treatment of intra-abdominal infections (see Table 1 below). [1] Single-agent, broad-spectrum therapy and combination therapies have been used against these infections, although …
Epidemiology
- In case of severe infections with features of systemic sepsis, a policy of \"hit early and hit hard\" (starting therapy as soon as infection is suspected with broad spectrum antibiotics) reduces the mortality of infection.
Clinical significance
- In patients with community-acquired peritonitis, coverage for Enterococcus is not recommended. Enterococcal coverage may be warranted in patients with septic shock who have received prolonged cephalosporin therapy, in patients who are immunosuppressed and are at risk for bacteremia, in patients with prosthetic heart valves, and in patients with rec...