What are evaluation and management medical billing codes?
What are Evaluation and Management Medical Billing Codes. In this article. Evaluation and management (E&M) codes are the most commonly billed codes and the medical coder/biller will use them a lot. These are the codes for every office visit and encounter a physician has with a patient, which typically involve non-invasive physician services.
What is the CPT code for evaluation and treatment?
The Current Procedural Terminology (CPT) code range for Evaluation and Management Services 99091-99499 is a medical code set maintained by the American Medical Association. Subscribe to Codify and get the code details in a flash.
Is the CPT code the same as the procedure code?
When a service or procedure is described the same by both CPT coding and HCPCS coding, the CPT code is used. When a CPT code includes instructions to add more information, a HCPCS code is used. There are 16 sections in the HCPCS manual. ADVERTISEMENT.
What is the CPT code for initial evaluation?
This article is revised to change the initial PT/OT evaluation codes to 97162-97163 for PT and 97165-97167 for OT and Reevaluation codes 97164 & 97168 and deleted CPT ® codes 97001, 97002, 97003 & 97004 effective 01/01/2017.
What are the evaluation and management CPT codes are based on three factors?
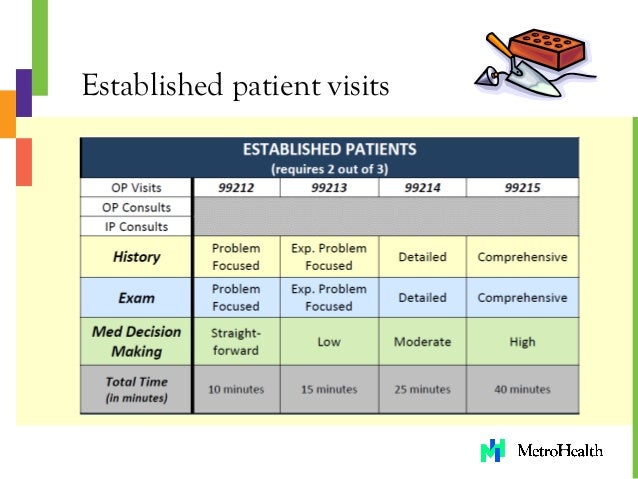
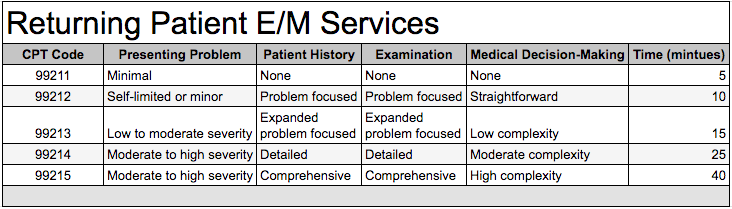
The charts that follow address the three KEY components to consider when selecting the level of code: History. Exam. Medical Decision Making.
What is the difference between E&M codes and CPT codes?
E/M stands for “evaluation and management”. E/M coding is the process by which physician-patient encounters are translated into five digit CPT codes to facilitate billing. CPT stands for “current procedural terminology.” These are the numeric codes which are submitted to insurers for payment.
What is the purpose of evaluation and management codes?
Evaluation and Management coding is a medical coding process in support of medical billing. Practicing health care providers in the United States must use E/M coding to be reimbursed by Medicare, Medicaid programs, or private insurance for patient encounters.
What are evaluation and management services?
Evaluation and management (E/M) services are cognitive (as opposed to procedural) services in which a physician or other qualified healthcare professional diagnoses and treats illness or injury.
What are the 3 key components of evaluation and management?
3 Key Components of E/M Coding: History, Exam, Medical Decision Making. Evaluation and management coding is a type of medical coding used by physicians and certain other healthcare providers to report their services as part of medical billing.
Can you bill an E&M with a procedure?
You can bill an E/M and a minor procedure (procedure with 0 or 10 global days) on the same calendar date. The writer quoted the CMS Claims Processing Manual. The same language is in the CMS manual and the NCCI manual.
Where are clinical examples for evaluation and management codes?
Where are clinical examples for evaluation and management codes found in the CPT® code book? Rationale: Appendix C of the CPT® code book contains clinical examples of evaluation and management codes. The appendix may be used in addition to the E/M code descriptors.
What services do evaluation and management codes report?
As the name E/M indicates, these medical codes apply to visits and services that involve evaluating and managing patient health. Examples of E/M services include office visits, hospital visits, home services, and preventive medicine services.
What are the 4 levels of history in E&M coding?
The E/M guidelines recognize four “levels of history” of incrementally increasing complexity and detail:Problem Focused.Expanded Problem Focused.Detailed.Comprehensive.
What is the first category of evaluation and management codes?
Office or Other Outpatient Services (99201-99215) is the first category that appears in the E/M section, but not all office and outpatient services are coded here. The category 99201-99215 identifies services to diagnose or treat health problems and symptoms.
How do I code E&M office visits?
Total time may be used alone to select the appropriate code level for office visit E/M services (99202-99205, 99212-99215). A key change in the new guidelines is the updated definition of time....Selecting E/M Codes by Total Time.CPT CodeTime Range9921320-29 minutes9921430-39 minutes9921540-54 minutes5 more rows
Why is the evaluation and management section located at the beginning of the CPT?
located at the beginning of CPT because these codes describe services (e.g., office visits) that are most frequently provided by physicians and other health care practitioners (e.g., nurse practitioner, physician assistant).
What are E&M codes used for in medical billing and coding?
Evaluation and management (E/M) coding is the use of CPT® codes from the range 99202-99499 to represent services provided by a physician or other qualified healthcare professional. As the name E/M indicates, these medical codes apply to visits and services that involve evaluating and managing patient health.
Who can bill for E&M codes?
PhysiciansReimbursement Guidelines CPT guidance instructs that E/M (CPT codes 99091, 99202-99499) should only be reported by Physicians or other qualified health care professionals.
What is a CPT code?
What is a CPT® code? The Current Procedural Terminology (CPT®) codes offer doctors and health care professionals a uniform language for coding medical services and procedures to streamline reporting, increase accuracy and efficiency.
What are the 4 levels of history in E&M coding?
The E/M guidelines recognize four “levels of history” of incrementally increasing complexity and detail:Problem Focused.Expanded Problem Focused.Detailed.Comprehensive.
What is the AMA CPT code set?
The AMA CPT ® code set includes E/M guidelines, but CMS has also published more specific guidance on proper E/M coding and documentation. Most notably, CMS issued the 1995 E/M Documentation Guidelines and the 1997 Documentation Guidelines to help providers and medical coders distinguish the various E/M service levels. Both the 1995 and 1997 E/M Documentation guidelines from CMS are still in use. Many third-party payers also apply these guidelines.
How many categories are there in CPT?
CPT ® includes more than two dozen categories of E/M codes, from office and other outpatient services to advance care planning. You may find further divisions within each category, such as separate options for new patients and established patients.
How many components are in an E/M code?
There are seven components used in the descriptors of many E/M codes, according to the CPT ® E/M guidelines section “Guidelines for Hospital Observation, Hospital Inpatient, Consultations, Emergency Department, Nursing Facility, Domiciliary, Rest Home, or Custodial Care, and Home E/M Services.” The first three are called key components for E/M level selection.
Why is E/M coding so difficult?
E/M coding can be difficult because of the factors involved in selecting the correct code. For example, many E/M codes require the coder to determine the type of history, examination, and medical decision making, which can involve using special grids and tables to check requirements.
What is E/M billing?
E/M service codes also may be used to bill for outpatient facility services. Facilities and practices may use E/M codes internally, as well, to assist with tracking and analyzing the services they provide. E/M services are high-volume services.
What are some examples of E/M services?
Examples of E/M services include office visits, hospital visits, home services, and preventive medicine services . Codes for services like surgeries and radiologic imaging are found outside of the E/M section of the CPT ® code set.
What is E/M code?
Medicare, Medicaid, and other third-party payers accept E/M codes on claims that physicians and other qualified healthcare professionals submit to request reimbursement for their professional services. E/M service codes also may be used to bill for outpatient facility services.
Why do physicians use E&M codes?
Physicians use E&M CPT codes to bill for services and obtain reimbursement. The AMA is responsible for creating the evaluation and management codes and the guidelines for how those codes are utilized. Physicians and coders must understand the guidelines so that they can accurately select the appropriate E&M codes for the service. Below are some important considerations to better understand the guidelines for selecting the appropriate evaluation and management codes.
What is CPT 4?
According to CMS, Current Procedural Terminology (CPT-4) is a numeric coding system maintained by the American Medical Association (AMA). The CPT-4 is a uniform coding system consisting of descriptive terms and identifying codes that are used primarily to identify medical services and procedures furnished by physicians and other healthcare professionals. These health care professionals use the CPT-4 to identify services and procedures for which they bill public or private health insurance programs. Evaluation and management codes are a part of the CPT-4 system and reviewed on a periodic basis by the AMA. In addition, CMS considers the CPT-4 as Level-I HCPCS for provider reimbursement under its HCPCS (Healthcare Common Procedure Coding System) reimbursement methodology.
What is an E&M code?
Evaluation and management codes, often referred to as E&M codes or E and M codes are a coding system that involve the use of CPT codes from the range 99202 to 99499 which represent services provided by a physician or other qualified healthcare professional. These evaluation and management CPT codes are utilized when the provider is involved in either evaluating or managing patient health. These E&M CPT codes are commonly used by specialty care consultants, emergency room physicians and primary care physicians. For example, office visits, hospital visits, home services and preventive medicine services are considered E&M codes. Codes for procedures like surgeries, radiology and diagnostic tests, and certain treatment therapies are not considered evaluation and management services.
Should CPT codes be reported separately?
Any additional procedure performed during the same encounter with a specific procedure code should be reported separately. For example, any diagnostic tests performed or interpreted and billed separately should not be included in determining the amount of time utilized when determining the appropriate evaluation and management CPT codes.
Is physical examination considered an element of outpatient codes?
However, the extent of the physical examination is not an element in selection of the level of office or other outpatient codes.
Is CPT reimbursement lowered?
In the past twenty years or so and even as recently as 2020, CMS has improved reimbursement for evaluation and management CPT codes. The counter trend is that reimbursement for procedures like surgeries and related specialties are being lowered. For example, endocrinologists, rheumatologists, hematologists/oncologists, family physicians and psychiatrists have seen reimbursement increases over the past few years. Conversely, radiologists, cardiac surgeons, anesthesiologists, critical care physicians and general surgeons are among those types of physicians projected to see the largest drops in Medicare reimbursement. Many other types of specialists will see drops as well.
Who performs E&M codes?
Evaluation and Management (E&M) codes are to be performed by physicians, nurse practitioners and physician assistants. Physician codes should be billed using the rendering provider’s individual NPI.
What is the Medicare level 2 outpatient visit code?
However, effective January 1, 2014, when E&M services are paid under Medicare’s Partial Hospitalization Program (PHP) and not in the physician office setting, the CPT outpatient visit codes 99201-99215 have been replaced with one Level II HCPCS code – G0463.
What is 99205 in medical?
99205 Office or other outpatient visit for the evaluation and management of a new patient, which requires these three key components: a comprehensive history; a comprehensive examination; and medical decision making of high complexity. Counseling and/or coordination of care with other physicians, other qualified health care professionals, or agencies are provided consistent with the nature of the problem (s) and the patient’s and/or family’s needs. Usually, the presenting problem (s) are of moderate to high severity. Typically, 60 minutes are spent face-to-face with the patient and/or family. Billing Instructions: Bill 1 unit per visit.
How long is a 99211 visit?
Usually, the presenting problem (s) are minimal. Typically, 5 minutes are spent performing or supervising these services.
How long does it take to get Medicare reimbursement for 99422?
99422 for 11 to 20 minutes of cumulative time within seven days. Medicare reimbursement is $30.01 every seven days.
What is the new 99423 code?
Three of the six new codes—99421, 99422, and 99423—apply to patient-initiated digital services provided by physicians. These codes enable physicians to bill for time they spend monitoring and evaluating patients between scheduled visits.
What is the CPT code for E/M office visit?
The revisions to the E/M office visit CPT® codes (99201-99215) code descriptors and documentation standards directly address the continuing problem of administrative burden for physicians in nearly every specialty.
When will E/M office visit coding be implemented?
These landmark changes to E/M office visit coding went into effect on January 1, 2021.
What is the code for prolonged Medicare?
Rather, physicians should use Healthcare Common Procedure Coding System (HCPCS) code G2212 for prolonged services for Medicare patients when the total time on the date of service exceeds the maximum required time of the primary procedure code that has been selected using total time on the date of the primary service.
What is E/M in Medicare 2021?
Many health systems that employ members are not implementing the evaluation and management (E/M) increases included in the 2021 Medicare physician fee schedule. Continuing to compensate at pre-2021 levels means meaningful investments in primary care are not being shared with employed physicians.
What is the CPT code for G2212?
Physicians should not bill HCPCS code G2212 with the following CPT codes: 99354, 99355, 99358, 99359, 99415, or 99416. Selecting E/M Codes by MDM. MDM is the reflection of complexity in establishing a diagnosis, assessing the status of a condition and/or selecting a management option.
What is E/M in medical?
Evaluation and management (E/M) codes are at the core of most family physician practices. Family physicians and other qualified health professionals (QHPs), such as nurse practitioners or physician assistants, can maximize payment and reduce the stress associated with audits by understanding how to properly document and code for E/M services.
Should physicians document time spent on the date of the encounter?
Physicians should ensure they document the total time spent on the date of the encounter in the patient’s medical record. Physicians should avoid documenting time ranges and instead document specific total time spent on activities on the date of the encounter. CPT Code. Time Range.
Is CPT code 99201 still valid?
These elements may still be necessary for clinical practice, professional liability (i. e., malpractice) reasons, and quality measurement. 99201 is no longer a valid code: CPT code 99201 has been deleted and is no longer available as a CPT code selection.
When was the CPT E/M revision approved?from ama-assn.org
To address this, on Feb. 9, 2019, the AMA-convened CPT Editorial Panel approved revisions to the CPT E/M office or other outpatient visit reporting guidelines and code descriptors. These revisions were in direct response to the leadership demonstrated by CMS Administrator, Seema Verma, to take on the challenge of revising the (E/M) office visit reporting guidelines.
What is the CPT code for E/M office visit?from ama-assn.org
This provision includes revisions to the Evaluation and Management (E/M) office visit CPT® codes (99201-99215) code descriptors and documentation standards that directly address ...
What is the ICd 10 code for TBI?from asha.org
The R41.84- series of ICD-10-CM codes is most commonly used to report cognitive deficits following TBI and includes specific codes for attention and concentration, cognitive communication , and frontal lobe and executive function deficits. Report this series of codes in conjunction with the S06- series to describe the type of TBI giving rise to the cognitive deficits. SLPs should always consult the medical record or referring physician to confirm the appropriate code to describe the type of TBI.
What is CPT 92605?from therapyplayground.com
In anticipation of the deletion of 92506, ASHA submitted a letter to the Centers for Medicare and Medicaid Services (CMS) requesting that CPT 92605 (Evaluation for prescription of non-speech-generating augmentative and alternative communication device , face-to-face with the patient; first hour) and CPT 92618 (each additional 30 minutes) be added to the Medicare Physician Fee Schedule (MPFS). We will not know whether this recommendation was accepted until CMS publishes the 2014 MPFS in November.Who should I contact if I have problems billing the new codes?
What is the CPT code for speech, language, voice, and communication?from asha.org
CPT code 92507 (speech, language, voice, and communication treatment) may also be appropriate if the focus of treatment is cognitive communication and if treatment goals are language-based. However, if the focus of treatment is primarily cognitive function, SLPs should report 97129 and 97130 unless specifically instructed by the payer.
What is the ICd 10 code for cognitive deficit?from asha.org
For patients without a related medical condition or language deficit, consider ICD-10-CM code F88 (other disorders of psychological development). Informal descriptions for F88 include "cognitive developmental delay."
What is the ICD-10 code for cerebral infarction?from asha.org
Use the I69- series of ICD-10-CM codes to report cognitive deficits following cerebrovascular disease. Each category of cerebrovascular disease—nontraumatic subarachnoid hemorrhage, nontraumatic intracerebral hemorrhage, other nontraumatic intracranial hemorrhage, cerebral infarction, other cerebrovascular diseases, unspecified cerebrovascular diseases—includes codes for specific cognitive deficits, including memory, attention and concentration, frontal lobe and executive function, and cognitive-social deficits. The I69- series of codes is one of the few used by SLPs that incorporate both the medical diagnosis and treating diagnosis in one category. SLPs should always consult the medical record or referring physician to confirm the type of cerebrovascular disease before selecting an I69- code.
