
What are macrolides and ketolides?
Macrolides and ketolides are antibiotics that inhibit bacterial protein synthesis Synthesis ...
Does clindamycin belong to macrolides?
The topically used clindamycin phosphate is a phosphate- ester prodrug of clindamycin. Clindamycin has a primarily bacteriostatic effect. At higher concentrations, it may be bactericidal. It is a bacterial protein synthesis inhibitor by inhibiting ribosomal translocation, in a similar way to macrolides.
Is nitrofurantoin a macrolide antibiotic?
Nitrofurantoin (Macrobid) is known as a nitrofuran antibiotic. This is currently the only product available in the United States that belongs to this class of medication. It isn't related to other antibiotics, such as penicillin or sulfa medications (e.g., Bactrim or Septra (sulfamethoxazole / trimethoprim) ), so providers might prescribe nitrofurantoin (Macrobid) if you are allergic to other antibiotics.
What does macrolides mean?
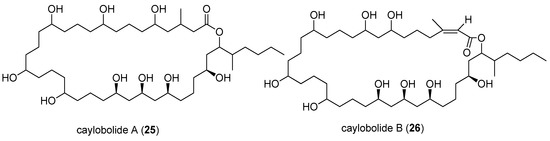
The macrolides are a class of natural products that consist of a large macrocyclic lactone ring to which one or more deoxy sugars, usually cladinose and desosamine, may be attached. The lactone rings are usually 14-, 15-, or 16-membered. Macrolides belong to the polyketide class of natural products.
What is the best macrolide antibiotic?
Erythromycin, azithromycin and clarithromycin are equally effective against most gram-positive organisms. However, clarithromycin and azithromycin have much better activity against Haemophilus influenza and Moraxella catarrhalis. Thus, these 2 drugs are better choices for the treatment of community-acquired pneumonia.
What drug belongs to macrolides?
Macrolides are a class of antibiotic that includes erythromycin, roxithromycin, azithromycin and clarithromycin.
What is the generic name of macrolides?
List of Macrolides:Drug NameAvg. RatingReviewsAzithromycin Dose Pack Generic name: azithromycin6.765 reviewsDificid (Pro) Generic name: fidaxomicin7.713 reviewsBiaxin XL Generic name: clarithromycin7.29 reviewsErythrocin (Pro) Generic name: erythromycin7.23 reviews11 more rows
Is amoxicillin a macrolide?
Azithromycin is in the macrolide category of antibiotics, while amoxicillin is in the beta-lactam/penicillin category. They work in different ways and have some differences, such as in indications and drug interactions.
What are the 4 macrolide antibiotics?
Five macrolide antibiotics are currently available for use in the United States: erythromycin, clarithromycin, azithromycin, fidaxomicin and telithromycin, the latter being a related ketolide.
Is penicillin a macrolide?
The antimicrobial spectrum of macrolides is slightly wider than that of penicillin, and, therefore, macrolides are a common substitute for patients with a penicillin allergy.
What are macrolides best used for?
Macrolides are a class of drugs used to manage and treat various bacterial infections. Azithromycin, clarithromycin, and erythromycin are commonly used to treat infections like pneumonia, sinusitis, pharyngitis, and tonsillitis. They are also used in uncomplicated skin infections and otitis media in pediatric patients.
What should you not take with azithromycin?
If you are taking aluminum or magnesium-containing antacids, do not take them at the same time that you take Zithromax®. These medicines may keep azithromycin from working properly. However, you can take antacids with Zmax®.
Is ciprofloxacin a macrolide?
Zithromax Z-PAK (azithromycin) and Cipro (ciprofloxacin) are antibiotics used to treat susceptible bacterial infections. Zithromax and Cipro belong to different antibiotic classes. Zithromax is a macrolide antibiotic and Cipro is a quinolone antibiotic.
What is the strongest antibiotic for bacterial infection?
Vancomycin, long considered a "drug of last resort," kills by preventing bacteria from building cell walls. It binds to wall-building protein fragments called peptides, in particular those that end with two copies of the amino acid D-alanine (D-ala).
Which is stronger azithromycin or amoxicillin?
Conclusions: In adults with acute sinusitis, a 3-day course of azithromycin was as effective and well tolerated as a 10-day course of amoxicillin/clavulanic acid. A significantly simpler dosage regimen and faster clinical effect were the advantages of azithromycin.
What is the strongest antibiotic for pneumonia?
Azithromycin is a first-line treatment for healthy adults under age 65 with bacterial pneumonia. It is often paired with another antibiotic like doxycycline or amoxicillin. Azithromycin is currently being studied for its effectiveness in treating secondary bacterial pneumonia that is sometimes associated with COVID-19.
Is ciprofloxacin a macrolide?
Zithromax Z-PAK (azithromycin) and Cipro (ciprofloxacin) are antibiotics used to treat susceptible bacterial infections. Zithromax and Cipro belong to different antibiotic classes. Zithromax is a macrolide antibiotic and Cipro is a quinolone antibiotic.
Is macrolide a tetracycline?
Abstract. Macrolides, lincosamides, tetracyclines and chloramphenicol are structurally unrelated antibiotics which share protein synthesis inhibition as their common mechanism of action.
Is clindamycin a macrolides?
Clindamycin is a macrolide antibiotic, which, when used as an antiprotozoan agent, is always combined with other therapies for the treatment of falciparum malaria, toxoplasmosis, and babesiosis.
What class of drug is clarithromycin?
Clarithromycin belongs to the class of medicines, known as macrolide antibiotics. It works by killing bacteria or preventing their growth. However, this medicine will not work for colds, flu, or other virus infections. This medicine is available only with your doctor's prescription.
What are the side effects of macrolide?
Some of the most common side effects of macrolide are nausea, vomiting, and diarrhea. Severe side effects include anaphylaxis, permanent sensorineu...
What kind of drugs are macrolides?
Macrolides are antibiotics that are bacteriostatic in nature, which means, these antibiotics have the ability to inhibit the growth of bacteria. Ho...
What are examples of macrolide antibiotics?
Some of the common examples of macrolide antibiotics are erythromycin, clarithromycin, azithromycin, fidaxomicin, and telithromycin. Different dose...
What is a macrolide?
Macrolides - StatPearls - NCBI Bookshelf. Macrolides are a class of drugs used in the management and treatment of various bacterial infections. This activity reviews the mechanism of action, indications, contraindications, and other key factors (e.g., off-label uses, dosing, pharmacodynamics, pharmacokinetics, monitoring, ...
How do macrolides work?
The mechanism of action of macrolides revolves around their ability to bind the bacterial 50S ribosomal subunit causing the cessation of bacterial protein synthesis. Once bound, the drug prevents the translation of mRNA, specifically the growing peptide chain, by preventing the addition of the next amino acid by the tRNA. Since the bacterial ribosomal structure is highly conserved across most, if not all, bacterial species, it is considered to be broad-spectrum.[7] Macrolides are considered to be bacteriostatic as they only inhibit protein synthesis, although, at high doses, they can be bactericidal.
Why are macrolides resistant to antibiotics?
Due to the overprescription of antibiotics, there has been tremendous growth in resistance to many mainstay therapies. Macrolides are no exception to this, and many organisms are excessively resistant to them. Studies show a strong link to genetic mutations in bacteria and the ability to spread these genes via transposable elements. The gene in question allows bacteria to be resistant to macrolides, lincosamides, and streptogramin groups of antibiotics at once. [8]
Why are macrolides used in COPD?
The use of these drugs in COPD is because of their anti-inflammatory and immunomodulating characteristics. [6] Mechanism of Action.
What is macrolide therapy?
Macrolides are a class of drugs used in the management and treatment of various bacterial infections. This activity reviews the mechanism of action, indications, contraindications, and other key factors (e.g., off-label uses, dosing, pharmacodynamics, pharmacokinetics, monitoring, relevant interactions) related to macrolides. NCBI.
Which antibiotic has the highest tendency to cause ventricular fibrillation?
Erythromycin has the highest tendency, and azithromycin has the lowest. The increase in the intervals puts patients at risk of cardiac arrhythmias like Torsades de pointes, ventricular tachycardia, and ventricular fibrillation. The most common arrhythmia arising from the use of macrolides would be Torsades de Pointes.
Can macrolides cause nausea?
Like any other antibiotic, macrolides carry a significant risk of typical adverse effects like nausea, vomiting , abdominal pain, and diarrhea. Abdominal symptoms are largely the result of macrolides being motilin agonists causing an increased risk of gastrointestinal upset and side effects.[9] .
What is macrolide used for?
Antibiotic macrolides are used to treat infections caused by Gram-positive bacteria (e. g., Streptococcus pneumoniae) and limited Gram-negative bacteria (e.g., Bordetella pertussis, Haemophilus influenzae ), and some respiratory tract and soft-tissue infections. The antimicrobial spectrum of macrolides is slightly wider than that of penicillin, and, therefore, macrolides are a common substitute for patients with a penicillin allergy. Beta-hemolytic streptococci, pneumococci, staphylococci, and enterococci are usually susceptible to macrolides. Unlike penicillin, macrolides have been shown to be effective against Legionella pneumophila, mycoplasma, mycobacteria, some rickettsia, and chlamydia .
Which bacteria are susceptible to macrolides?
Beta-hemolytic streptococci, pneumococci, staphylococci, and enterococci are usually susceptible to macrolides. Unlike penicillin, macrolides have been shown to be effective against Legionella pneumophila, mycoplasma, mycobacteria, some rickettsia, and chlamydia .
What is macrolide antibiotic?
The macrolide antibiotics erythromycin, clarithromycin, and roxithromycin have proven to be an effective long-term treatment for the idiopathic , Asian-prevalent lung disease diffuse panbronchiolitis (DPB).
How does bacterial resistance to macrolides occur?
The primary means of bacterial resistance to macrolides occurs by post-transcriptional methylation of the 23S bacterial ribosomal RNA. This acquired resistance can be either plasmid -mediated or chromosomal, i.e., through mutation, and results in cross-resistance to macrolides, lincosamides, and streptogramins (an MLS-resistant phenotype).
How old can a horse be to take macrolide?
It can be used in horses less than one year old, but care must be taken that other horses (such as a foal's mother) do not come in contact with the macrolide treatment. Macrolides can be administered in a variety of ways that include tablets, capsules, suspensions, injectings and topically.
When was the first macrolide discovered?
The first macrolide discovered was erythromycin, which was first used in 1952 . Erythromycin was widely used as a substitute to penicillin in cases where patients were allergic to penicillin or had penicillin-resistant illnesses. Later macrolides developed, including azithromycin and clarithromycin, stemmed from chemically modifying erythromycin;
What is the mechanism of action of macrolides?
The mechanism of action of macrolides is inhibition of bacterial protein biosynthesis, and they are thought to do this by preventing peptidyltransferase from adding the growing peptide attached to tRNA to the next amino acid (similarly to chloramphenicol) as well as inhibi ting bacterial ribosomal translation.
What are the main concerns with macrolides?
Main concerns with macrolides include. Gastrointestinal (GI) disturbances (mainly with erythromycin) QT-interval prolongation by erythromycin. Inhibition of hepatic metabolism, leading to numerous drug interactions.
Where do macrolides diffuse?
Once absorbed macrolides diffuse well into body fluids, except cerebrospinal fluid, and are concentrated in phagocytes. Excretion is mainly in bile.
What subunit of the ribosome is a macrolide?
Videos (0) Macrolides (see table Macrolides) are antibiotics that are primarily bacteriostatic; by binding to the 50S subunit of the ribosome, they inhibit bacterial protein synthesis.
Is a macrolide contraindicated?
Macrolides are contraindicated in patients who have had an allergic reaction to them.
Does food affect macrolides?
Food has the following effects on macrolide absorption: For azithromycin capsules and erythromycin (including base and stearate formulations), decreased absorption. Once absorbed macrolides diffuse well into body fluids, except cerebrospinal fluid, and are concentrated in phagocytes. Excretion is mainly in bile.
What are the advantages of macrolides?
A great advantage of macrolides is that they are active against harmful Gram-positive cocci. Antibiotics of this group can easily cope with pneumococci, pyogenic streptococci, atypical mycobacteria. Among other things, they destroy:
What is the name of the drug that fights atypical mycobacteria?
The macrolide drug, called Clarithromycin, fights Helicobacter and atypical mycobacteria.
What is the name of the group of drugs that are used to control bacteria?
All representatives of the list of drugs-macrolides - antibacterial drugs. Their chemical structure is based on the macrocyclic lactone ring. Hence - the name of the group. They are used to control various types of bacteria. And thanks to the fact that these funds are quite effective, medicine uses them very actively.
Can macrolides be used for rheumatism?
Antibiotics of this group are also prescribed for the sanation of patients who are carriers of meningococcus. And they can be a good prevention of rheumatism or endocarditis.
What is macrolide used for?
Macrolides are used in the treatment of a wide range of infections – both Gram-positive and Gram-negative infections. In the case of H. pylori infection, macrolides are used alongside other drugs – typically a penicillin and a proton-pump inhibitor (what is referred to as “ triple therapy ”).
What is macrolide antibiotic?
Antibacterial macrolides are widely prescribed drugs for an even wider variety of infections. Here, we review the macrolides pharmacology you need to know. We discuss the indications that macrolides are licensed to treat, how they work, what side effects they’re linked to, and what drug interactions you need to bear in mind.
Why do bacteria resist macrolides?
However, bacterial resistance to macrolides is relatively common, often caused by mutations within the ribosome that prevent the macrolide from binding.
Which subunit does macrolides bind to?
More specifically, macrolides bind to the 50S ribosomal subunit; binding that results in blockade of the translocation process which is needed for the polypeptide chain to grow and elongate.
Can macrolides prolong QT?
QT prolongation. At high doses, macrolides can cause ototoxicity. QT prolongation is more likely if macrolides are administered along side other drugs that also prolong the QT interval – such as SSRIs, antipsychotics, quinine, and fluoroquinolones.
Can you use macrolides for Helicobacter pylori?
Eradication of Helicobacter pylori infection. In the case of H. pylori infection, macrolides are used alongside other drugs – typically a penicillin and a proton-pump inhibitor (what is referred to as “ triple therapy ”). Patients who are allergic to penicillins can be given metronidazole instead.
Can macrolides interact with statins?
Given that macrolides interact with many CYP enzymes, there are important drug interactions to consider. Taking macrolides with statins can, for example, increase the risk of myopathies. Both erythromycin and clarithromycin inhibit CYP enzymes, whereas azithromycin does not. Similarly, taking macrolides with warfarin can increase the risk of bleeding.
Which antibiotics are considered macrolides?
Lincosamides: Lincosamide antibiotics are considered with macrolides due to similar antimicrobial spectra, therapeutic application and mechanism of action (inhibits protein synthesis by binding to 50S ribosome). Lincomycin and Clindamycin:
What are macrolide antibiotics?
Here is a list of various macrolide antibiotics. 1. Erythromycin : (i) This macrolide antibiotic was isolated from Streptomyces erythreus, a soil- born organism in 1952. (ii) It consists of two sugars, desosamine and cladinose, which are attached to erythronolide, a macro cyclic lactone. (iii) It is slightly water soluble.
What is the antimicrobial spectrum?
Antimicrobial Spectrum: These are active against gram positive pathogens like penicillinase producing staphylococcus, streptococcus, Clostridium tetani, cl. diphtheriae, cl. welchii as well as several Actinomyces, some Nocardia and certain strains of Mycoplasma pneumoniae.
Is a bacterial fagilis effective against mycobacteria?
2. In addition, it is effective against Mycobacterium avium complex, other atypical mycobacteria, Mycobacterium leprae and some anaerobes but not Bact. fagilis.

Overview
Examples
US FDA-approved :
• Azithromycin - unique; does not extensively inhibit CYP3A4
• Clarithromycin
• Erythromycin
Definition
In general, any macrocyclic lactone having greater than 8-membered rings are candidates for this class. The macrocycle may contain amino nitrogen, amide nitrogen (but should be differentiated from cyclopeptides), an oxazole ring, or a thiazole ring. Benzene rings are excluded, in order to differentiate from tannins. Also lactams instead of lactones (as in the ansamycin family) are excluded. Included are not only 12-16 membered macrocycles but also larger rings as in tacrolim…
History
The first macrolide discovered was erythromycin, which was first used in 1952. Erythromycin was widely used as a substitute to penicillin in cases where patients were allergic to penicillin or had penicillin-resistant illnesses. Later macrolides developed, including azithromycin and clarithromycin, stemmed from chemically modifying erythromycin; these compounds were designed to be more easily absorbed and have fewer side-effects (erythromycin caused gastrointestinal side-effects i…
Uses
Antibiotic macrolides are used to treat infections caused by Gram-positive bacteria (e.g., Streptococcus pneumoniae) and limited Gram-negative bacteria (e.g., Bordetella pertussis, Haemophilus influenzae), and some respiratory tract and soft-tissue infections. The antimicrobial spectrum of macrolides is slightly wider than that of penicillin, and, therefore, macrolides are a common substitute for patients with a penicillin allergy. Beta-hemolytic streptococci, pneumococci
Mechanism of action
Macrolides are protein synthesis inhibitors. The mechanism of action of macrolides is inhibition of bacterial protein biosynthesis, and they are thought to do this by preventing peptidyltransferase from adding the growing peptide attached to tRNA to the next amino acid (similarly to chloramphenicol ) as well as inhibiting bacterial ribosomal translation. Another potential mechanism is premature dissociation of the peptidyl-tRNA from the ribosome.
Resistance
The primary means of bacterial resistance to macrolides occurs by post-transcriptional methylation of the 23S bacterial ribosomal RNA. This acquired resistance can be either plasmid-mediated or chromosomal, i.e., through mutation, and results in cross-resistance to macrolides, lincosamides, and streptogramins (an MLS-resistant phenotype).
Two other types of acquired resistance rarely seen include the production of drug-inactivating e…
Side-effects
A 2008 British Medical Journal article highlights that the combination of some macrolides and statins (used for lowering cholesterol) is not advisable and can lead to debilitating myopathy. This is because some macrolides (clarithromycin and erythromycin, not azithromycin) are potent inhibitors of the cytochrome P450 system, particularly of CYP3A4. Macrolides, mainly erythromycin and clarithromycin, also have a class effect of QT prolongation, which can lead to torsades de po…