- To track progress. SOAP notes create a treatment record so you can track the client’s progress towards their therapy goals. ...
- To communicate with other therapists. This is how we communicate with other massage therapists. ...
- For future reference. ...
- Liability protection. ...
How to write massage therapy SOAP notes?
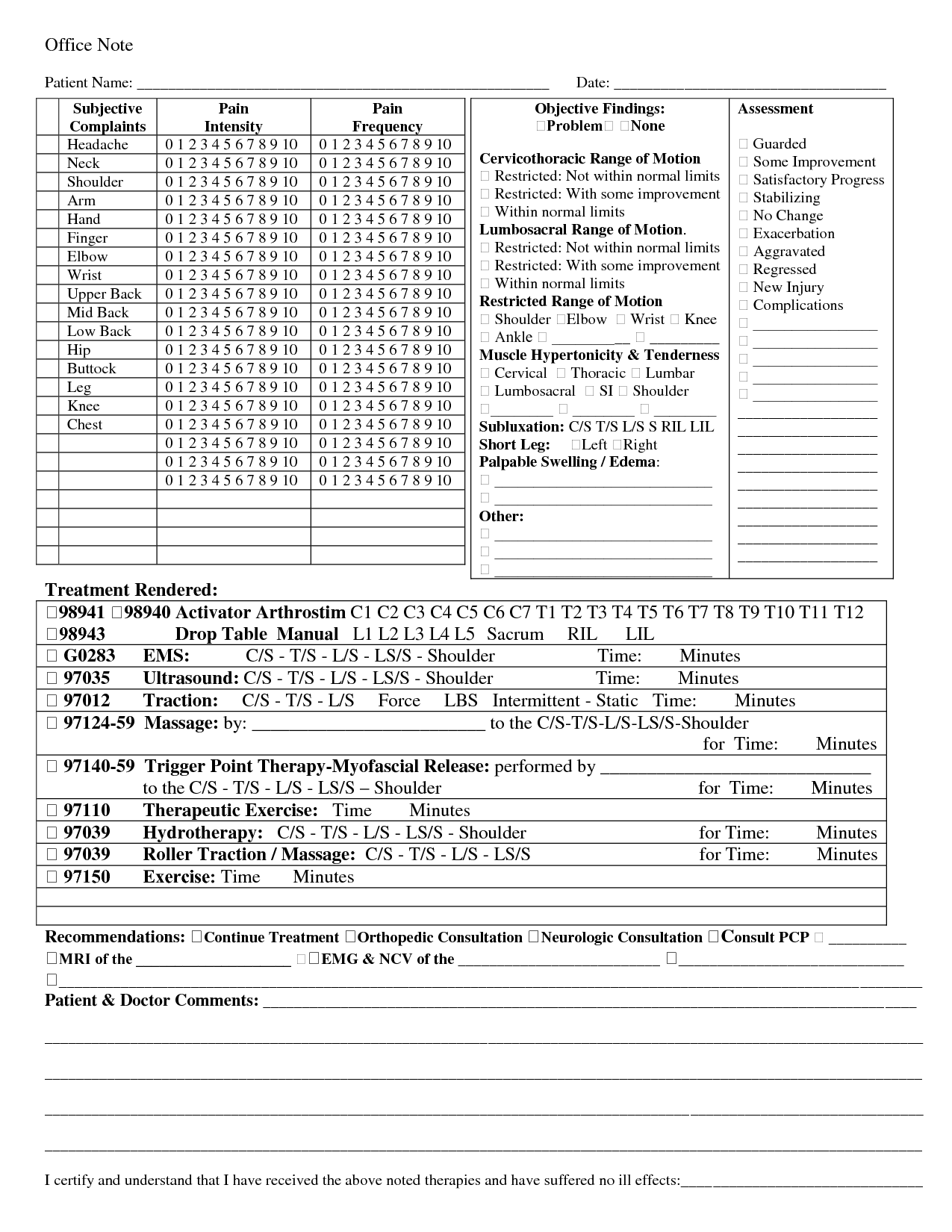
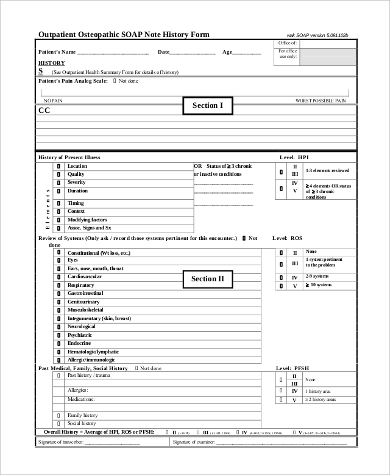
What goes in the Objective section of a SOAP note?
- Observations from assessment or reassessment, e.g. ROM, posture, etc.
- Progress towards goals, based on objective findings
- Details of specific treatments/modalities provided today. ...
- Observable or palpable response to today’s massage treatment
What does SOAP notes stand for?
The Subjective, Objective, Assessment and Plan (SOAP) note is an acronym representing a widely used method of documentation for healthcare providers. The SOAP note is a way for healthcare workers to document in a structured and organized way.[1][2][3]
What are SOAP notes considered?
The SOAP note stands for Subjective, Objective, Assessment, and Plan. This note is widely used in medical industry. Doctors and nurses use SOAP note to document and record the patient’s condition and status. The SOAP note is considered as the most effective and standard documentation used in the medical industry along with the progress note.
Do you use SOAP note?
SOAP notes are used so staff can write down critical information concerning a patient in a clear, organized, and quick way. SOAP notes, once written, are most commonly found in a patient’s chart or electronic medical records.

Do massage therapists have to take SOAP notes?
(Updated for 2022) Writing treatment notes is one of the routine activities that massage therapists do every day. The most common form that therapists use to document their client sessions is the SOAP note.
How do you write a good SOAP note?
Tips for Effective SOAP NotesFind the appropriate time to write SOAP notes.Maintain a professional voice.Avoid overly wordy phrasing.Avoid biased overly positive or negative phrasing.Be specific and concise.Avoid overly subjective statement without evidence.Avoid pronoun confusion.Be accurate but nonjudgmental.
What does SOAP notes stand for?
Subjective, Objective, Assessment and PlanIntroduction. The Subjective, Objective, Assessment and Plan (SOAP) note is an acronym representing a widely used method of documentation for healthcare providers. The SOAP note is a way for healthcare workers to document in a structured and organized way.[1][2][3]
What is the 3 important skills in hand massage?
These skills can be divided into three categories: social, physical, and mental skills. Since massage therapists work closely with clients, it is very important that they possess certain social skills, such as the ability to communicate effectively.
How do you write a SOAP note for a massage?
SOAP stands for a four-step note-taking process:Subjective: information about the client's own description of their chief complaint.Objective: observable and measurable information about the client's current symptoms gathered by the massage therapist and other professionals.More items...•
How do you start a SOAP note?
information gathered during your session.Focus on your next steps for the upcoming session. ... Focus on things both parties have agreed to.Note nutritional, physical, medical attributes that will contribute to the client's therapeutic goals.Note any progression/regression client has made in treatment.Implementation.More items...
What should be included in a SOAP note assessment?
SOAP Note TemplateDocument patient information such as complaint, symptoms and medical history.Take photos of identified problems in performing clinical observations.Conduct an assessment based on the patient information provided on the subjective and objective sections.Create a treatment plan.More items...•
How do you write SLP SOAP notes?
What is the SOAP method?S: Subjective. This is a statement about the relevant status or behavior that has been observed in your patient. ... O: Objective. This section includes quantifiable, measurable, and observable data. ... A: Assessment. This is where you interpret what “S” and “O” mean in your report. ... P: Plan.
What goes under assessment in a SOAP note?
An evaluation SOAP note must include all scores from the eval. This could include: Summary of Screening results. Assessment/Test/Evaluation results.
What are the four attributes of successful massage therapists?
Here are the four traits that make for a successful and effective massage therapist:They excel at communication. Being a massage therapist means working with a wide array of clients. ... They love working with people. ... They're dedicated to the craft. ... They don't mind a little hard work.
What are the basic massage movements?
The first thing that every student must master is “the basics.” The four basic massage strokes are effleurage-(light or deep stroking), petrisage-(kneading), tapotement-(gentle slapping), and friction.
What makes a good massage therapist?
What are the Qualities of a Good Massage Therapist?Quality #1: Educated. The most important part of being a massage therapist is having the correct training. ... Quality #2: Articulate. ... Quality #4: Flexible. ... Quality #5: Friendly. ... Quality #7: Comforting. ... Quality #8: Careful. ... Quality #9: Methodical. ... Quality #10: Hygienic.More items...•
Free SOAP Notes Form
SOAP (Subjective, Objective, Assessment and Plan) notes are used at intake and ongoing to document a client's condition and progress. They are also useful when communicating with insurance companies.
Prefer Digital SOAP Notes?
If you're ready to take your client documentation off the page and into the cloud, check out ClinicSense, a complete practice management software package — AMTA members save 25%.
Why Are SOAP Notes Important?
SOAP Notes can be time-consuming to complete. But don’t underestimate the importance of this record-keeping method. Well-written, detailed SOAP Notes enable you and your staff to quickly memorialize and communicate essential information about a person’s current health status and their ongoing treatment plan.
SOAP: What Does It Stand For?
Subjective: information about the client’s own description of their chief complaint
A Massage Therapy SOAP Notes Example
To illustrate the entire note-taking process in action, let’s take another massage therapy SOAP notes example. In this case, the subjective phase of the SOAP process begins by noting that the client’s chief complaint is pain in the lower back and upper leg.
Tips for Writing Good SOAP Notes
How can you create well-written SOAP Notes that help keep everyone on the same page?
Speed up Your Note-taking and Streamline Your Filing by Going Digital with Help from ClinicSense
Taking handwritten notes using a printed form can get the job done. But, if manually recording and filing your SOAP notes seems like too much of a drag on your time, there is an alternative.
Make Taking SOAP Notes Easy with ClinicSense
With ClinicSense, taking SOAP notes is as easy as pointing and clicking to answer a few key questions. No more writing, typing or trying to figure out what to say. Transform your responses into finalized notes quickly, easily and professionally.
What is a premium soap note?
Premium SOAP Notes let you draw on the anatomical figure itself. These visual markers make it easy to see and remember a patient’s condition during their next visit. All client SOAP notes are easily accessible directly from the schedule or from a client’s individual record in the client management area. Another example of how MassageBook’s seamlessly integrated solution can simplify things dramatically and put the information you need at your fingertips.
What is massage book?
MassageBook electronically captures massage therapy session notes about your patients to help you track the treatment process and insurance billing. In addition to SOAP notes, this software is also a massage therapist’s one-stop-shop for marketing, website development, online scheduling, gift certificates, and more.
Do massage therapists need soap notes?
Free, simple, and effective SOAP notes for massage therapists. SOAP notes are not only a great way to keep track of your clients’ progress, they‘re required if you’re considering doing any insurance billing.
Is massage book backed up?
Unlike paperwork, which you can easily misplace, your MassageBook SOAP notes are backed up online. There’s no need for offsite storage, and you can access them remotely any time and from anywhere.
Is massage book soap note secure?
SOAP notes are not only a great way to keep track of your clients’ progress; they‘re required if you’re considering doing any insurance billing. MassageBook SOAP notes are easy to use and seamlessly tied to each client’s appointment records, making it easy to find past notes and create new ones. They’re fully secure and HIPAA-compliant, so you’ll ...
What Are SOAP Notes?
One standard form of healthcare documentation is called SOAP notes, which stands for Subjective Objective Assessment and Plan. Each section of this general formula is key to gathering a comprehensive report of the patient’s current experience and determining the best treatment plan.
Importance of SOAP Notes and Treatment Documentation
The phrase “if it’s not documented, then it didn’t happen” might sound extreme, but in the world of healthcare—whether medical or holistic—it’s the norm.
Why SOAP Notes are Important for Insurance Billing
SOAP notes are also important for insurance billing purposes; because healthcare documentation is an essential part of operating a successful holistic practice, it’s vital that your insurance billing process is as streamlined as possible.
What is a therapy soap note?
Therapy SOAP notes follow a distinct structure that allows medical and mental health professionals to organize their progress notes precisely. [1] As standardized documentation guidelines, they help practitioners assess, diagnose, and treat clients using information from their observations and interactions.
What is a soap note?
An effective SOAP note is a useful reference point in a patient’s health record, helping improve patient satisfaction and quality of care.
What is a soap progress note?
SOAP is an acronym for the 4 sections, or headings, that each progress note contains: Subjective: Where a client’s subjective experiences, feelings, or perspectives are recorded. This might include subjective information from a patient’s guardian or someone else involved in their care.
Why are soap notes important?
SOAP notes also play a valuable role in Applied Behavior Analysis, by allowing professionals to organize sessions better and communicate with a client’s other medical professionals. Legally, they may also accompany insurance claims to evidence the service being provided. [4]
What is the purpose of a detailed assessment?
A detailed Assessment section should integrate “subjective” and “objective” data in a professional interpretation of all the evidence thus far, and. Plan: Where future actions are outlined.
Is soap a subjective or unbiased?
Unbiased: In the Subjective section, particularly, there is little need for practitioners to use weighty statements, overly positive, negative, or otherwise judgmental language. SOAP notes are frequently used both as legal documents and in insurance claims.
SOAP note example for Nurse or Nurse Practitioner
John reports that he is feeling 'tired' and that he 'can't seem to get out of bed in the morning.' John is 'struggling to get to work' and says that he 'constantly finds his mind wondering to negative thoughts.' John stated that his sleep had been broken and he does not wake feeling rested.
SOAP note example for Psychotherapist
Stacey reports that she is 'feeling good' and enjoying her time away. Stacey reports she has been compliant with her medication and using her meditation app whenever she feels her anxiety.
SOAP note example for Paediatrician
Mrs. Jones states that Julia is "doing okay." Mrs. Jones said her daughter seems to be engaging with other children in her class. Mrs. Jones said Julia is still struggling to get to sleep and that "she may need to recommence the magnesium." Despite this, Mrs. Jones states she is "not too concerned about Julia's depressive symptomology.
SOAP note example for Social Worker
Martin has had several setbacks, and his condition has worsened. Martin reports that the depressive symptoms continue to worsen for him. He feels that they are 'more frequent and more intense. Depressive symptomology is chronically present.
SOAP note example for Psychiatrist
Ms. M. states that she is "doing okay." Ms. M. states that her depressive symptomatology has improved slightly; she still feels perpetually "sad." Ms. M.
SOAP note example for Therapist
"I'm tired of being overlooked for promotions. I don't know how to make them see what I can do." Frasier's chief complaint is feeling "misunderstood" by her colleagues.
SOAP note example for Counselor
David states that he continues to experience cravings for heroin. He desperately wants to drop out of his methadone program and revert to what he was doing.