Neuromuscular blocking agents (NMBAs) are usually administered during anesthesia to facilitate endotracheal intubation and/or to improve surgical conditions. NMBAs may decrease the incidence of hoarseness and vocal cord injuries during intubation, and can facilitate mechanical ventilation in patients with poor lung compliance [ 1-5 ].
What are neuromuscular blocking drugs?
Neuromuscular blocking drugs are medications that induce paralysis. Complete muscle relaxation permits easier tracheal intubation, which is insertion of a breathing tube into the trachea. Intubation is done prior to initiating mechanical ventilation (breathing machine use) in someone having surgery or critically ill patients.
What are the indications for neuromuscular blocking agents?
Neuromuscular Blocking Agents: Use and Controversy in the Hospital Setting. NMBAs are common in surgical situations and rapid sequence intubation, but other indications, such as acute respiratory distress syndrome, therapeutic hypothermia, and elevated intracranial pressure, are somewhat divisive.
What is the best depolarizing neuromuscular blocking agent?
The most well-known depolarizing neuromuscular blocking agent is succinylcholine. It is the only such drug used clinically and is considered by many the drug of choice for emergency department RSI, although this is controversial.
How are neuromuscular blocking agents (NMBAs) administered?
The administration of neuromuscular blocking agents is most effective via an intravenous or intramuscular route. NMBAs are poorly absorbed if administered orally.[15] The route of administration is dependent on the patient’s clinical condition, desired speed of action, and duration of clinical effect.
What is a neuromuscular junction blocker?
Neuromuscular-blocking drugs block neuromuscular transmission at the neuromuscular junction, causing paralysis of the affected skeletal muscles. This is accomplished via their action on the post-synaptic acetylcholine (Nm) receptors.
What drugs can paralyze the body?
Propofol and alfentanyl provide alternatives to thiopental and succinylcholine for rapid sequence intubation. A paralyzing agent can be added to the combination of propofol and fentanyl using the timing principle and, thereby, reduce the doses of sedating agents to achieve the same goal.
What is the primary mode of action of a neuromuscular blocking agent?
Mechanism of Action: Neuromuscular blocking agents prevent acetylcholine stimulation at the motor endplate by combining with and occupying these specific receptors. Through this action, neuromuscular blocking agents prevent muscle contraction and induce temporary muscle immobility (paralysis).
Which patient would a neuromuscular blocking drug be contraindicated in?
Depolarizing agents are absolutely contraindicated in patients with degenerative neuromuscular disorders or a history of malignant hyperthermia. Undiagnosed children with skeletal muscle myopathy, such as Duchenne's muscular dystrophy, are at risk for rhabdomyolysis with hyperkalemia.
How do they wake you up from anesthesia?
After the procedure When the surgery is complete, the anesthesiologist reverses the medications to wake you up. You'll slowly wake either in the operating room or the recovery room. You'll probably feel groggy and a little confused when you first wake.
Which drug causes permanent paralysis?
Common paralytics include atracurium, cisatracurium, mivacurium, rocuronium, succinylcholine, and vecuronium. How long is a paralytic used?
How does a neuromuscular blocking agent interfere with muscle contraction?
They bind to muscle receptors and trigger a muscle contraction but then produce a persistent depolarization, so preventing further muscle contractions.
What tablets are muscle relaxants?
Antispasmodics: Centrally Acting Skeletal Muscle RelaxersCarisoprodol (Soma) Carisoprodol is a centrally acting muscle relaxant. ... Chlorzoxazone (Lorzone, Parafon Forte DSC, Remular-S) ... Cyclobenzaprine (Amrix) ... Metaxalone (Skelaxin) ... Methocarbamol (Robaxin) ... Orphenadrine (Norflex) ... Baclofen (Ozobax) ... Tizanidine (Zaniflex)More items...
What is neuromuscular paralysis?
Abstract. Acute neuromuscular paralysis (ANMP) is a clinical syndrome characterized by rapid onset muscle weakness progressing to maximum severity within several days to weeks (less than 4 wk). Bulbar and respiratory muscle weakness may or may not be present.
Why is it called train of four?
Image by Medscape. The train of four received its name because the machine delivers four electrical impulses one after the next.
Where is the neuromuscular junction located?
The neuromuscular junction (NMJ) is a synaptic connection between the terminal end of a motor nerve and a muscle (skeletal/ smooth/ cardiac). It is the site for the transmission of action potential from nerve to the muscle.
What is the difference between depolarizing and nondepolarizing neuromuscular blockers?
Depolarizing muscle relaxants act as acetylcholine (ACh) receptor agonists, whereas nondepolarizing muscle relaxants function as competitive antagonists.
Is there a drug that causes temporary paralysis?
The FDA has approved sugammadex, marketed as Bridion, to reverse the effects of neuromuscular blockade induced during certain types of surgery by rocuronium bromide and vecuronium bromide. The 2 neuromuscular blocking drugs cause temporary paralysis by interfering with nerve impulse transmission to muscles.
What is a drug that causes temporary paralysis by blocking the transmission?
Succinylcholine often is used to produce paralysis quickly at the start of a surgical procedure (and then is supplemented later with a competitive blocking agent) or for brief procedures.
What drugs affect the spinal cord?
Methamphetamine, or "meth," is a central nervous system stimulant. The drug attacks the brain and spinal cord by interfering with normal nuerotransmissions. By doing so it creates feelings of well being and prolonged energy reserves.
What are the drugs acting on nervous system?
There are many different types of drugs that work on the CNS, including anesthetics, anticonvulsants, antiemetics, antiparkinson agents, CNS stimulants, muscle relaxants, narcotic analgesics (pain relievers), nonnarcotic analgesics (such as acetaminophen and NSAIDs), and sedatives.
What was the significance of the introduction of neuromuscular blocking agents?
The introduction of NMBA led to a significant conceptual change in the practice of anesthesia. Anesthesia was redefined to include a triad of narcosis, analgesia, and muscle relaxation. This activity outlines the indications, mechanism of action, methods of administration, important adverse effects, contraindications, monitoring, and toxicity of NMBAs, so providers can direct patient therapy to optimal outcomes in anesthesia and other conditions where NMBA have therapeutic benefit.
How does NMDA work?
When administered, instead of causing depolarization of the motor plate at the NMJ, they block acetylcholine from binding to the motor plate at the NMJ, an action achieved by competing for the binding site on the alpha subunit of the nicotinic receptors. As the concentration of non-depolarizing NMBA builds up at the junction, relative to ACh, it establishes a neuromuscular blockage. [12]
What is a non depolarizing NMBA?
This action makes the motor endplate refractory to the action of ACh. An example of non-depolarizing NMBA is succinylcholine. Succinylcholine or suxamethonium has a quick onset of action and rapidly metabolizes via the enzymatic action of pseudocholinesterase. The continued disruption of the effect of ACh causes muscular fasciculation and twitching. The onset of action is about 1 minute, and the duration is about 6 minutes.[11] It is the only depolarizing NMBA in clinical use.
Where does the NMBA act?
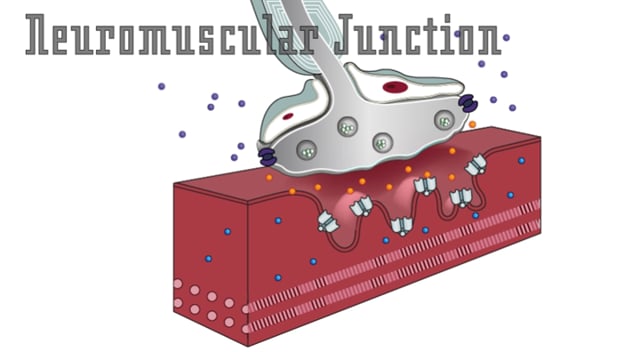
NMBA act at the neuromuscular junction (NMJ). The NMJ consists of three parts
How many structural classes are there in the NMBA?
There are two major structural classes of non-depolarizing NMBA.
Is NMBA intravenous or intramuscular?
The administration of neuromuscular blocking agent is most effective via an intravenous or intramuscular route. NMBAs are poorly absorbed if administered orally.[15] The route of administration is dependent on the patient’s clinical condition, desired speed of action, and duration of clinical effect. In most instances, NMBA administration is intravenous. Dose administration can be as boluses or continuous infusion. Continuous infusion is usually administered in the intensive care unit setting where prolonged paralysis might be necessary or in instances where the surgical procedures will dictate a significant amount of time.
Where does the presynaptic nerve terminal come from?
The presynaptic nerve terminal consists of motor neurons originating from the ventral horn of the spinal cord. The motor neuron loses its myelin sheath as it embeds in the muscle tissue. Motor neuron secretes trophic and growth factors.
What is neuromuscular blocker?
Neuromuscular blockers are a class of medications that prevent acetylcholine from acting at the neuromuscular junction, which prevents the triggering of skeletal muscle contractions. Okay, first things first.
How long does it take for neuromuscular blockers to work?
Gradually, in about 40 to 90 minutes, these muscles start recovering in ...
What are the parts of the neuromuscular junction?
The neuromuscular junction has three main parts: a presynaptic membrane, which is the membrane of an axon terminal; a postsynaptic membrane, which is the membrane of a skeletal muscle fiber and is also called a motor end-plate; and a synaptic cleft, which is the gap between the presynaptic and postsynaptic membranes.
Which neuron activates the lower motor neuron?
The upper motor neuron then activates a lower motor neuron in the spinal cord.
Do neuromuscular blockers bind to acetylcholine?
So, non-depolarizing neuromuscular blockers can bind to the same binding sites on the receptor as acetylcholine, but they don’t trigger the opening of ion channels. So when administered, they compete for these binding sites on the receptors, which leads to decreased depolarization of the muscle fiber and weaker contraction.
What are Neuromuscular blocking agents?
Neuromuscular blocking agents are potent muscle relaxants typically only used during surgery to prevent muscle movement. They are structurally related to acetylcholine (the main neurotransmitter in the body) and they cause muscle relaxation by binding to acetylcholine receptors postsynaptically (which prevents acetylcholine from binding).
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
What is neuromuscular blocking agent?
Neuromuscular blocking agents are used to facilitate intermittent positive-pressure ventilation (IPPV) as part of a balanced anesthetic technique or as part of an anesthetic technique for animals undergoing intensive care mechanical ventilation. Neuromuscular blockade will help to prevent respiratory dyssynchrony, stop spontaneous respiratory efforts and muscle movement, improve gas exchange, and facilitate inverse ratio ventilation. 1 Neuromuscular blocking agents may also be useful in managing increased intracranial pressure and the muscle spasms of tetanus, drug overdose, or seizures. 1 Their use in surgery is to enhance skeletal muscle relaxation, to facilitate control of respiratory efforts during intrathoracic surgery, to immobilize the eye for ocular surgery, and to facilitate difficult intubation. 2
What are the two classes of neuromuscular blocking drugs?
There are two broad classes of neuromuscular blocking drugs: non-depolarizing agents, of which the prototype is curare (for example, d-tubocurarine, atracurium, metocurine, mivacurium, pancuronium, rocuronium, vecuronium) and depolarizing blockers, such as suxamethonium. This monograph is largely concerned with the former; suxamethonium is the subject of a separate monograph.
How do nondepolarizing NMBs block neuromuscular transmission?
Nondepolarizing NMBs block neuromuscular transmission predominantly by competitive antagonism of ACh at the postjunctional receptor . The effect of this competitive antagonism depends on the relative concentrations of NMB and ACh and the comparative affinities of each for the AChR. Under normal conditions, acetylcholinesterase rapidly cleaves ACh in the synaptic cleft, thereby improving the competitive advantage of the NMB to bind to the receptor. If an inhibitor of acetylcholinesterase is added to the mix, the concentration of ACh in the cleft remains high and there is a shift in favor of ACh binding to the receptor. The NMBs compete with ACh at the two binding sites of the AChR. Therefore only one molecule of NMB is needed to prevent activation of the receptor, whereas two ACh molecules are needed for activation. This biases the competition strongly in favor of the antagonist (NMB) drug.
What are the two classes of NMBAs?
NMBAs can broadly be divided into two separate classes based on their mechanism of action. Depolarizing agents such as succinylcholine mimic the action of acetylcholine at the neuromuscular junction and activate or depolarize the muscle, whereas nondepolarizing agents such as pancuronium or rocuronium block the effects of acetylcholine at the neuromuscular junction, acting as competitive antagonists.
What is NMBA in ARDS?
Neuromuscular blocking agents (NMBAs) are commonly used to facilitate MV during ARDS; but, despite wide acceptance, there are few data and as yet no consensus available for when these agents should be used. Gainnier and associates (2004) were the first to report the effects of a 48-hour NMBA infusion on gas exchange in patients with early ARDS. All patients were ventilated according to the ARDSNet protocol. Significant improvements in oxygenation and ability to lower PEEP occurred in the NMBA group and were sustained beyond the 48-hour infusion period. Although it remains to be elucidated why muscle paralysis improves oxygenation, NMBAs are thought to decrease oxygen consumption, promote patient-ventilator interface, and increase chest wall compliance.
What is non depolarizing neuromuscular blocking agent?
Non-depolarizing neuromuscular blocking agents compete with acetylcholine for receptors at the neuromuscular junction and clinical relaxation begins when 80–85% of the receptors on the motor end-plate are blocked. They do not produce depolarization themselves and, by blocking access to the receptors, prevent the normal acetylcholine- induced depolarization. Flaccid paralysis ensues. Their action terminates when acetylcholine again gains access to the receptors, due to diffusion of the relaxant molecules away from the neuromuscular junction. This may be hastened by greatly increasing the number of acetylcholine molecules at the motor end-plate by giving an anticholinesterase such as neostigmine. In contrast, the depolarizing blockers first depolarize the motor end-plate and then prevent further depolarization.
Why do we need NMBs?
All NMBs cause profound muscle weakness , but agents vary greatly in duration of action. If neuromuscular blockade is necessary and continuous EEG recording is not being performed, a single dose of a short-acting, nondepolarizing agent should be administered; it is impossible to ascertain clinically whether seizure activity is continuing in the presence of neuromuscular blockade. Anticonvulsant treatment should continue as outlined earlier, and EEG monitoring should be strongly considered. If a long-acting agent is used or if multiple doses of a short-acting agent are given, continuous EEG monitoring is mandatory to prevent unrecognized SE. All patients receiving NMBs should be intubated.
Why are neuromuscular blocking agents important?
Neuromuscular blocking agents (NMBAs) play an important role in the management of a large number of hospital patients. In addition to their routine use in surgical anesthesia, NMBAs may be valuable in many new and evolving critical care situations. Therefore, it is essential for the hospital pharmacist to become familiar with ...
What is NMBA used for?
Surgical: NMBAs have been a staple of anesthesiology and surgery since the introduction of succinylcholine in 1952. 3-7 The choice of agent and dosing varies widely depending on the surgical procedure and also on the use of alternative agents, including general anesthetics, local anesthetics, and IV sedation medications. Of primary concern in the surgical use of NMBAs is to achieve appropriate levels of muscular blockade without inducing cardiovascular side effects or lengthening the total duration of blockade beyond the time frame of the surgical procedure. 4 Although a full discussion of agent selection and dosing for surgical indications is beyond the scope of this article, the clinical reversal of these effects will be addressed. Clinical monitoring of a patient who has received an intermediate- to long-acting NMBA during a surgical procedure should include peripheral nerve stimulation (PNS) testing (discussed later). 1,4
What are depolarizing NMBAs?
Depolarizing NMBAs act as agonists at nicotinic receptors. 1 They hold open the ion-gated channels, leading to muscular fasciculation until the ion potential is depleted, and then to paralysis. 2 Succinylcholine is the only depolarizing NMBA available. Nondepolarizing NMBAs are competitive antagonists at nicotinic receptors, blocking acetylcholine at the motor endplate. 1 This prevents the action potential from spreading, thereby rendering muscle cells insensitive to motor nerve impulses. Muscle paralysis occurs sequentially, beginning with small, fast-twitch muscles in the eyes and larynx and progressing to the limbs, trunk, airway, intercostal muscles, and diaphragm. Recovery from neuromuscular blockage occurs in the reverse order. 2
How does NMBA affect oxygen consumption?
18 By controlling shivering , NMBAs may decrease total oxygen consumption. Although this has not been studied in critical care, these physiologic changes have been demonstrated in surgical patients undergoing hypothermia during cardiopulmonary bypass. 19,20 In a retrospective study of 111 patients who underwent therapeutic hypothermia (18 with NMBA vs. 93 without), there was an improvement in hospital survival ( P = .004) that remained significant after multivariate analysis of potential baseline confounders (95% CI, 1.56-33.38). 21 A trend toward improvements in lactate clearance and functional outcomes was also noted in patients receiving continuous NMBA.
What are the effects of NMBAs?
As a result, side effects such as tachycardia and bradycardia, hypertension and hypotension, and bronchodilation and bronchospasm have been seen with their use ( TABLE 1 ).
What is the effect of acetylcholine on muscle fibers?
Acetylcholine binds to nicotinic receptors at the endplate, resulting in the release of Na+ ( sodium) into muscle fibers , which triggers the muscular action potential. Calcium ions are then released into the sarcoplasmic reticulum, provoking the binding of myosin to actin.
Is there a trial for neuromuscular blockade?
There are no trials providing specific guidance on the management of unintentional awareness during neuromuscular blockade. Regardless, it is considered standard practice to establish and maintain appropriate levels of analgesia and deep sedation prior to and during neuromuscular blockade. 1.
Where are neuromuscular blockers used?
Current Use of Neuromuscular Blocking Agents in Intensive Care Units
What are neuromuscular blocking agents?
Neuromuscular blocking agents can be used for purposes such as eliminating ventilator-patient dyssynchrony, facilitating gas exchange by reducing intra-abdominal pressure and improving chest wall compliance, reducing risk of lung barotrauma, decreasing contribution of muscles to oxygen consumption by preventing shivering and limiting elevations in intracranial pressure caused by air way stimulation in patients supported with mechanical ventilation in intensive care units. Adult Respiratory Distress Syndrome (ARDS), status asthmaticus, increased intracranial pressure and therapeutic hypothermia following ventricular fibrillation-associated cardiac arrest are some of clinical conditions that can be sustained by neuromuscular blockade. Appropriate indication and clinical practice have gained importance considering side effects such as ICU-acquired weakness, masking seizure activity and longer durations of hospital and ICU stays. We mainly aimed to review the current literature regarding neuromuscular blockade in up-to-date clinical conditions such as improving oxygenation in early ARDS and preventing shivering in the therapeutic hypothermia along with summarising the clinical practice in adult ICU in this report.
How are neuromuscular blockers reversed?
Originally, all neuromuscular blockers were reversed via acetylcholinesterase inhibitors (neostigmine, edrophonium, pyridostigmine).[13] . The reversal occurs by these agents blocking acetylcholinesterase enzymes present in the synaptic cleft and function to break down ACh.
What is a non depolarizing neuromuscular blocker?
Non-depolarizing neuromuscular blockers are often administered to assist endotracheal intubations and provide adjuvant therapy in the perioperative maintenance of anesthesia and care of the critically ill patient. These drugs paralyze muscles and make it difficult to breathe.
What is a nnmb?
Primarily nNMBs (rocuronium, vecuronium, pancuronium, atracurium, cisatracurium, mivacurium) are used to facilitate airway management and decrease the risk of laryngeal injury during regular and emergent intubations . [1] nNMBs can reduce hoarseness secondary to intubation via decreasing the incidence of vocal cord injuries.[2] .
What is the primary drug interaction to monitor?
The primary drug interaction to monitor is the co-administration of nNMBs and inhaled anesthetics (desflurane, sevoflurane, isoflurane, enflurane, halothane, NO). Inhaled anesthetics augment nNMB activity so that the dosing of nNMB must be reduced to accommodate. If there is no reduction in dosing, then the risk of a residual blockade and ensuing pulmonary distress increases.[1] Other categories of drug interactions are differentiated by either augmenting or eliciting resistance of activity[9]:
What is the administration route for NNMBS?
nNMBs administration is via the IV route. All agents have individualized dosing[8]:
How does hypothermia prolong blockade?
Hypothermia: Prolongs blockade by decreasing metabolism and elimination
Does neostigmine cause parasympathetic dysfunction?
Giving only neostigmine, clinically the most relevant of the acetylcholinesterase inhibitors, causes increased parasympathetic effects, the most worrisome of these effects being bronchospasm and laryngeal collapse. Glycopyrrolate, an anti-muscarinic agent, was added to this regimen to alleviate these effects.