
The approved PQRS measures are the four anesthesia specific measures:
- #30 – Perioperative Care: Timely Administration of Prophylactic Parenteral Antibiotics
- #44 – Coronary Artery Bypass Graft: Preoperative Beta-Blocker in patients with isolated CABG surgery
- #76 – Prevention of Catheter-Related Bloodstream Infections
- #193 – Perioperative Temperature Management
Full Answer
What is PQRS and why is it important?
The Physician Quality Reporting System (PQRS) has been using incentive payments, and will begin to use payment adjustments in 2015, to encourage eligible health care professionals (EPs) to report on specific quality measures. Why PQRS . PQRS gives participating EPs the opportunity to assess the quality of care they are providing to their
What is PQRS and why should I participate?
3 rows · The Physician Quality Reporting System (PQRS) was a reporting program of the Centers for Medicare ...
How to pass PQRS?
Formerly known as the Physician Quality Reporting Initiative (PQRI), the Physician Quality Reporting System (PQRS) was a voluntary reporting program that provided a financial incentive for certain health care professionals, including psychologists, who participated in Medicare to submit data on specified quality measures to the Centers for Medicare and Medicaid Services …
What are the types of quality measures?
This document contains general guidance for the 2016 Physician Quality Reporting System (PQRS) Individual Measure Specifications and Measure Flows for claims and registry reporting. The individual measure specifications are detailed descriptions of the quality measures and are intended to be utilized by individual eligible professionals reporting individual measures via …
What is PQRS in healthcare?
Physician Quality Reporting System (PQRS) The Physician Quality Reporting System (PQRS) was a reporting program of the Centers for Medicare and Medicaid Services (CMS). It gave eligible professionals (EPs) the opportunity to assess the quality of care they were providing to their patients, helping to ensure that patients get the right care at ...
Who is eligible for PQRS?
EPs include Medicare physicians (Doctors of Medicine), Practitioners (Nurse Practitioners), and Therapists (Physical Therapists).
What is the most common method of reporting nuclear medicine?
The most common method the Nuclear Medicine community has for reporting measures is individual measures reporting. The three mechanisms that can be used to report these measures are described below:
Is PQRS mandatory?
Participating in the PQRS is not mandatory, it is voluntary. However, the program used a combination of incentive payments and payment adjustments to promote reporting of quality information by EPs. Those who participated and successfully met the measure reporting criteria of the program receive incentive payments (bonus).
What is PQRS in medical terms?
What is the Physician Quality Reporting System ? Formerly known as the Physician Quality Reporting Initiative (PQRI), the Physician Quality Reporting System (PQRS) was a voluntary reporting program that provided a financial incentive for certain health care professionals, including psychologists, who participated in Medicare to submit data on ...
When did PQRS end?
PQRS ended as a stand-alone program on Dec. 31. 2016; the PQRS quality measures became part of the Merit-based Incentive Payment System (MIPS) in 2017.
How many measures are required for a psychologist to report?
If a psychologist reports on one to eight measures, or nine measures across fewer than three domains, their claims will automatically be reviewed by CMS under the Measure Validation Process (MAV) so that CMS can determine if additional measures should have been reported.
Is PQRS a Medicare program?
PQRS is not run by the Medica re Administrative Contractors. The CMS Office of Clinical Standards and Quality administers several quality improvement programs for the agency, including PQRS.
Do psychologists get VM?
No, psychologists’ payments are not subject to the VM at this time. The VM is currently being applied only to payments for physicians. Nonphysicians, solo practitioners and small group practices will not be impacted by the VM until 2018.
Can you start a bonus claim early?
No, but you should not take too long to decide. Because you must report on 50 percent of the applicable cases during the 12-month reporting period, failure to start early could prevent you from reaching this threshold and make you ineligible for the bonus payment.
Can you report PQRS as an individual?
If the practice has signed up to report under the group reporting option, you cannot choose to separately report PQRS measures as an individual because your National Provider Identification (NPI) number is linked to the TIN used by the group.
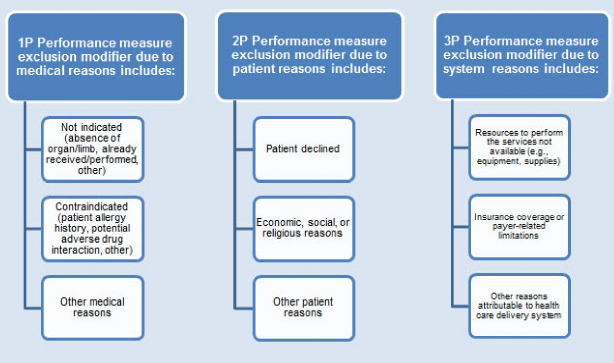
What is the second component of a PQRS measure?
The second component is the numerator describing the specific clinical action required by the measure for performance. EPs may use the codes present in the numerator to report the outcome of the action as indicated by the measure. PQRS measure numerators are quality-data codes (QDCs) consisting of specified non-payable CPT Category II codes and/or temporary G-codes. For GPRO Web Interface and electronic reporting using an EHR, other clinical coding sets may be included such as SNOMED, LOINC, or RxNorm in order to capture a specific quality action, test, or value.
What is the first measure component?
The first measure component is the denominator , which describes the eligible cases for a measure or the eligible patient population. Physician Quality Reporting measure denominators are identified by ICD-10-CM , ICD-10-PCS, CPT Category I, and HCPCS codes, as well as patient demographics (age, gender, etc.), and place of service (if applicable). For GPRO Web Interface and electronic reporting using an EHR, other clinical coding sets may be included such as SNOMED, LOINC, or RxNorm.
What is a PQRS negative payment adjustment?
A quality reporting program that uses negative payment adjustments to promote reporting of quality information by individual eligible professionals (EPs) and group practices. Those who do not satisfactorilyreport data on quality measures for covered Medicare Physician Fee Schedule (MPFS) services furnished to Medicare Part B beneficiaries (including Railroad Retirement Board, Medicare Secondary Payer, and Critical Access Hospitals [CAH] method II) will be subject to a negative payment adjustment under PQRS. Medicare Part C–Medicare Advantage beneficiaries are not included.
What is PFS in Medicare?
Provides differential payment to a physician or group of physicians under the Medicare Physician Fee Schedule (PFS) based upon the quality of care furnished compared to the cost of care during a performance period.
What is CMS collaborating with?
CMS is collaborating with specialty societies to ensure that the measures represented within Specialty Measure Sets accurately illustrate measures associates within a particular clinical area (suggested, NOT required); the following were established in 2015:
What is Lindsey's job?
Lindsey works with healthcare providers and hospitals to advance the use of electronic health records (EHR) to improve patient care and health outcomes. She consults with physician practices and hospitals to successfully implement and meaningfully use EHRs, including assistance associated with vendor products, hardware, software and system configuration and troubleshooting, staffing considerations, workflow analysis, EHR utilization, security and privacy, and quality data reporting from EHR systems.
What is a VBM?
The Value Based Modifier (VBM) program will assess the PQRS quality data and Medicare cost data to calculate a provider’s overall VBM score and apply an upward, downward or neutral payment adjustment that will reflect payments in 2017.
What is a measure group?
Measures groups are a subset of four or more PQRS measures that have a particular clinical condition or focus in common. All applicable measures within a group must be reported for each patient within the sample that meets the required criteria (such as age or gender). G Codes are reported by the Registry.
What is a G8442?
Patient not eligible for pain assessment for documented reasons. G8442: Documentation that patient is not eligible for a pain assessment. Pain assessment documented, follow-up plan not documented, patient not eligible/appropriate.
Is elder maltreatment documented?
Elder maltreatment screen not documented, reason not given. G8536: No documentation of an elder maltreatment screen, reason not given. Elder maltreatment screen documented as positive, follow-up plan not documented, reason not given.
