
Symptoms
Warning signs of a medical emergency include:
- Vomiting blood
- Vomiting substances that look like coffee grounds
- Severe rectal bleeding and/or bloody stools
- Sudden, severe pain in the upper abdominal area with or without evidence of bleeding
- Cold, clammy skin
- Rapid heartbeat
- Fainting 2
Causes
Peptic ulcer
- Overview. Peptic ulcers are open sores that develop on the inside lining of your stomach and the upper portion of your small intestine.
- Symptoms. The most common peptic ulcer symptom is burning stomach pain. ...
- Causes. ...
- Risk factors. ...
- Complications. ...
- Prevention. ...
Prevention
such as stomach ulcers.” It says your GP should arrange for you to see a specialist if you have symptoms that could be due to stomach cancer. Some of the early signs are similar to signs caused by other conditions, but should be checked nonetheless.
Complications
Ulcers can also cause severe symptoms such as vomiting blood, change in stool appearance – dark blood – and appetite changes, which usually result in weight loss. Burning retrosternal or epigastric pain – top middle part of your abdomen – is a sign you may have an ulcer.
What is the most serious complication of an ulcer?
How do you know if you have a stomach ulcer?
What are the signs of an ulcer?
Do ulcers make you throw up?

How to reduce the risk of peptic ulcers?
Use caution with pain relievers. If you regularly use pain relievers that increase your risk of peptic ulcer, take steps to reduce your risk of stomach problems. For instance, take your medication with meals. Work with your doctor to find the lowest dose possible that still gives you pain relief.
What causes peptic ulcers?
The most common causes of peptic ulcers are infection with the bacterium Helicobacter pylori (H. pylori) and long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve). Stress and spicy foods do not cause peptic ulcers. However, they can make your symptoms worse.
What is a peptic ulcer?
Overview. A peptic ulcer is a sore on the lining of your stomach, small intestine or esophagus. A peptic ulcer in the stomach is called a gastric ulcer. A duodenal ulcer is a peptic ulcer that develops in the first part of the small intestine (duodenum). An esophageal ulcer occurs in the lower part of your esophagus.
How to tell if you have a peptic ulcer?
Feeling of fullness, bloating or belching. Intolerance to fatty foods. Heartburn. Nausea. The most common peptic ulcer symptom is burning stomach pain. Stomach acid makes the pain worse, as does having an empty stomach. The pain can often be relieved by eating certain foods that buffer stomach acid ...
Where does a peptic ulcer occur?
An esophageal ulcer occurs in the lower part of your esophagus. Peptic ulcers are open sores that develop on the inside lining of your stomach and the upper portion of your small intestine. The most common symptom of a peptic ulcer is stomach pain. Peptic ulcers include: Gastric ulcers that occur on the inside of the stomach.
Can peptic ulcers cause black stools?
Many people with peptic ulcers don't even have symptoms. Less often, ulcers may cause severe signs or symptoms such as: Vomiting or vomiting blood — which may appear red or black. Dark blood in stools, or stools that are black or tarry.
Can NSAIDs cause peptic ulcers?
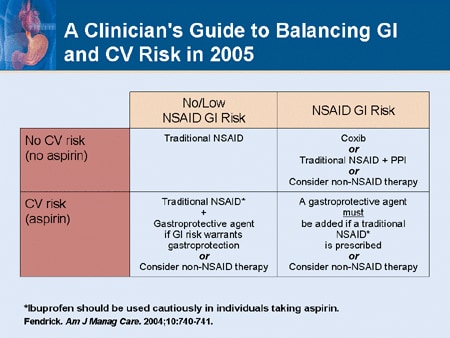
If you need an NSAID, you may need to also take additional medications such as an antacid, a proton pump inhibitor, an acid blocker or cytoprotective agent. A class of NSAIDs called COX-2 inhibitors may be less likely to cause peptic ulcers, but may increase the risk of heart attack. By Mayo Clinic Staff.
Who is at greatest risk for pressure ulcers?
People at the greatest risk of developing pressure ulcers are those who are immobile. Once a person loses the ability to move and becomes inactive, the risk of developing bedsores increases.
Why are pressure ulcers painful?
Also known as bedsores, pressure ulcers are a common problem for palliative care patients as mobility decreases and patients spend more time in bed. Pressure ulcers are painful and can be difficult to treat. Preventing pressure ulcers is critical to maintaining comfort and treating them promptly is essential.
Why is it important to take steps to prevent pressure ulcers?
As a person ages, the skin becomes thinner and more fragile, increasing the risk of skin breakdown. If your loved one has any of these risk factors, it's important for you to take steps to prevent a pressure ulcer from developing.
Where do pressure ulcers develop?
on December 11, 2020. There are several risk factors for pressure ulcers, the skin sores that typically develop over bony areas, such as the lower spine, hips, and elbows.
Can you feel pressure ulcers without sensory loss?
Patients who have experienced loss of sensation as the result of spinal cord injury or neurological disease have an increased risk of developing pressure ulcers. 1 A person without sensory loss can feel pain and will generally feel uncomfortable after spending a lot of time in one position. When the sensory loss occurs, a person may not feel ...
Does incontinence cause skin breakdown?
Incontinence. As above, incontinence of bowel movements and urine create moisture on the skin and increase the risk of breakdown. Fecal incontinence has the added risk of damage to the skin from bacteria and enzymes in the stool and also increases the risk of infection.
What are the complications of a stomach ulcer?
Some of the complications of stomach ulcers are as follows: INTERNAL BLEEDING: It is the most common problem which occurs when the ulcer forms at the site of a blood vessel. Bleeding can either be slow and long-term leading to anemia or rapid and severe causing a person to pass blood in vomit or stools.
What are the different types of ulcers?
TYPES OF ULCERS are: PEPTIC ULCERS: These develop on the inside lining of the stomach and the upper portion of the small intestine or esophagus. They form when digestive juices damage the lining of the stomach or intestine.
Why do duodenal ulcers develop in O blood groups?
This is because people of this blood group are unable to produce certain substances on the surface of blood cells that protect the lining of the duodenum.
What is the difference between a duodenal ulcer and an esophageal ulcer?
Ulcers are breaks or holes in the protective lining of the stomach or duodenum. Duodenal ulcers are more common than stomach ulcers. Comparatively rare, esophageal ulcers, which forms in the esophagus ( swallowing tube) are often the result of alcohol abuse or exposure to medications like certain anti-inflammatory drugs and antibiotics.
Why do I have ulcers on my stomach?
Causes of ulcers are as follows: Stomach Ulcers are more likely to develop in people having a sedentary lifestyle or poor eating habits. Oesophageal ulcers often result from exposure to medications such as certain antibiotics or anti-inflammatories and alcohol abuse.
What are the symptoms of an inflamed stomach ulcer?
Symptoms are: Repeated vomiting with large particles of undigested food particles. Persistent feeling of bloating or fullness.
What is the most common type of ulcer on the leg?
Arterial ulcers appear as red, yellow or black with hairless skin and leg pain. VENOUS ULCERS: It is the most common type of leg ulcers and is often formed on the leg, below the knee, and on the inner area of the ankle.
What are the signs of pressure ulcers?
reddened areas of skin that blanch when light pressure is applied).
Why do patients with poor mobility have increased risk of developing pressure ulcers?
Poor mobility/immobility: Patients who are unable to independently change position are at increased risk of developing a pressure ulcer, due to pressure exerted over bony prominences which results in reduced blood flow to the tissues and subsequent hypoxia.
Why is pressure ulcer risk assessment important?
Pressure ulcer risk assessment is crucial to the prevention of pressure ulcers. There are many factors which put certain patients at higher risk of developing these painful injuries that increase health care costs and lead to prolonged hospitalization, and sometimes death.
Why are pressure ulcers more likely to develop at the extremes of age?
Age: At the extremes of age, patients may be at higher risk for the development of pressure ulcers due to inability to move/change position independently. Very young infants are unable to change position by themselves; the elderly may be similarly unable to change position due to other health problems limiting movement.
Can a poor nutritional status cause ulcers?
Poor nutritional status: Although there are few studies to support this idea, it is widely accepted (based on anecdotal evidence) that patients who are compromised nutritionally are at higher risk for the development of pressure ulcers; for this reason, patients with poor nutritional status may benefit from a dietary consult.
How to tell if you have a peptic ulcer?
What are the symptoms of a peptic ulcer? 1 bloating 2 burping 3 feeling sick to your stomach 4 poor appetite 5 vomiting 6 weight loss
How long does it take for a peptic ulcer to come and go?
comes and goes for several days, weeks, or months. Less common symptoms may include. bloating. burping. feeling sick to your stomach. poor appetite. vomiting. weight loss. Even if your symptoms are mild, you may have a peptic ulcer.
How do NSAIDs help with peptic ulcers?
To understand how NSAIDs cause peptic ulcer disease, it is important to understand how NSAIDs work. Nonsteroidal anti-inflammatory drugs reduce pain, fever, and inflammation, or swelling. Everyone has two enzymes that produce chemicals in your body’s cells that promote pain, inflammation, and fever. NSAIDs work by blocking or reducing the amount of ...
What does it mean when your stomach hurts?
A dull or burning pain in your stomach is the most common symptom of a peptic ulcer. You may feel the pain anywhere between your belly button and breastbone. The pain most often. happens when your stomach is empty—such as between meals or during the night. stops briefly if you eat or if you take antacids.
Can a peptic ulcer get worse?
You should see your doctor to talk about your symptoms. Without treatment, your peptic ulcer can get worse. A dull or burning pain in your stomach is the most common symptom of peptic ulcers.
Can H. pylori cause peptic ulcers?
Once H. pylori have damaged the mucous coating, powerful stomach acid can get through to the sensitive lining. Together, the stomach acid and H. pylori irritate the lining of the stomach or duodenum and cause a peptic ulcer.
How to prevent stomach ulcers?
Prevention of stomach ulcers. To prevent the spread of bacteria that might cause a stomach ulcer, wash your hands with soap and water on a regular basis. Also, be sure to properly clean all of your food and to cook it thoroughly as needed.
What is a stomach ulcer?
Stomach ulcers are a type of peptic ulcer disease. Peptic ulcers are any ulcers that affect both the stomach and small intestines. Stomach ulcers occur when the thick layer of mucus that protects your stomach from digestive juices is reduced. This allows the digestive acids to eat away at the tissues that line the stomach, causing an ulcer.
What is the treatment for a stomach ulcer caused by H. pylori?
Nonsurgical treatment. If your stomach ulcer is the result of H. pylori, you’ll need antibiotics and drugs called proton pump inhibitors (PPIs). PPIs block the stomach cells that produce acid. In addition to these treatments, your doctor may also recommend: H2 receptor blockers (drugs that also block acid production) stopping use of all NSAIDs.
Why is it important to take care of a stomach ulcer?
It’s important to get a stomach ulcer taken care of because without treatment, ulcers and H. pylori can cause: bleeding from the ulcer site that can become life-threatening. penetration, which occurs when the ulcer goes through the wall of the digestive tract and into another organ, such as the pancreas.
How to diagnose a stomach ulcer?
To diagnose a stomach ulcer, your doctor will review your medical history along with your symptoms and any prescription or over-the-counter medications you’re taking. To rule out H. pylori infection, a blood, stool, or breath test may be ordered.
How long does it take for a stomach ulcer to go away?
Typically, the pain will be more intense when your stomach is empty, and it can last for a few minutes to several hours. Other common signs and symptoms of ulcers include: dull pain in the stomach. weight loss. not wanting to eat because of pain.
What is the name of the condition that causes stomach ulcers?
Rarely, a condition known as Zollinger-Ellison syndrome can cause stomach and intestinal ulcers by increasing the body’s production of acid.
How to prevent ulcerative colitis?
The best way to avoid ulcerative colitis from causing complications is to treat the disease effectively . That does mean working with a gastroenterologist and, usually, taking medication (s). Stopping medications suddenly, even when feeling better, is not typically recommended.
What are the risk factors for colon cancer?
Other risk factors include if a patient also has a liver disease associated with ulcerative colitis called primary sclerosing cholangitis and if there is a family history of colorectal cancer. After eight to 10 years of having ulcerative colitis, the risk of colon cancer starts to increase.
How long does it take to get a colonoscopy for ulcerative colitis?
For these reasons, continuing treatment for ulcerative colitis is important, as is regular screening for colorectal cancer. After eight to 10 years of having ulcerative colitis, a yearly colonoscopy might be recommended to check for polyps or colon cancer.
Does ulcerative colitis cause bone loss?
Bone Loss. People with ulcerative colitis may develop vitamin deficiencies, including a vitamin D deficiency. Vitamin D is the "helper" vitamin for calcium, and an appropriate amount of calcium is needed to keep bones healthy.
Can ulcerative colitis cause shortness of breath?
Anemia. One of the hallmark symptoms of ulcerative colitis is blood in the stool. In severe cases, there may be a significant amount of bleeding. The body can’t replace this blood as fast as it is being lost. This results in anemia, which can cause fatigue, weakness, chest pain, shortness of breath, and dizziness.
Is colon cancer a concern?
It is a valid concern because the risk of colon cancer is higher in people who are diagnosed with ulcerative colitis than it is in people who do not live with the disease. It’s important to note that more than 90% of people diagnosed with IBD will never develop colon cancer.
Can colitis cause diarrhea?
Ulcerative colitis can cause signs and symptoms such as diarrhea, blood in the stool, nausea, fatigue, and abdominal pain. One of the goals of treatment is to stay on top of the inflammation that may contribute to these symptoms.
Overview
Symptoms
Causes
Risk Factors
Complications
- There is no clear evidence to suggest that the stress of modern life or a steady diet of fast food causes ulcers in the stomach and small intestine, but they are nonetheless common in our society: About one out of every 10 Americans will suffer from the burning, gnawing abdominal pain of a peptic (or gastric) ulcer at some point in life.
Prevention