What factors can impact afterload?
Factors that affect afterload include : Increased or decreased aortic pressure—when the blood pressure is increased, there is a natural increase in the pressure the ventricle must press against and increased Similarly, when the blood pressure is reduced, there is less force to be pressed against by the ventricles and a reduction in afterload.
What are the main causes of increased afterload?
In short, blood inertia influences afterload in the following ways:
- It increases afterload in early systole. ...
- It decreases afterload in late systole. ...
- Its influence is increased with increased heart rate, which makes logical sense because to accelerate the same mass over a shorter systolic timeframe would require greater force and therefore would ...
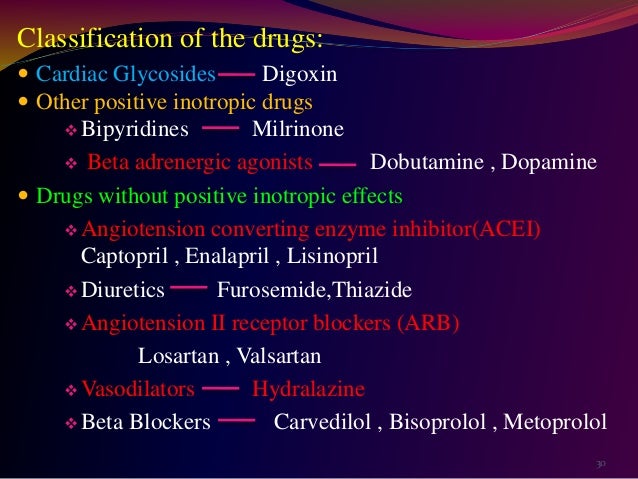
Which drugs decrease preload and afterload?
Premedication with drugs that decrease preload (eg, nitroglycerin [NTG]) and afterload (eg, angiotensin-converting enzyme [ACE] inhibitors) before the administration of loop diuretics can prevent adverse hemodynamic changes. Correspondingly, what medications decrease afterload? A hydralazine and nitrate combination reduces preload and afterload.
What does increased afterload mean?
Afterload. Afterload is a measure of the force resisting the ejection of blood by the heart. Increased afterload (or aortic pressure, as is observed with chronic hypertension) results in a reduced ejection fraction and increased end-diastolic and end-systolic volumes.
What effect does afterload have?
Factors which affect afterload: valve resistance, vascular resistance, vascular impedance, blood viscosity, intrathoracic pressure, and the relationship of ventricular radius and volume. Determinants which are specific to the right and left ventricles.
What affects afterload the most?
Afterload is increased when aortic pressure and systemic vascular resistance are increased, by aortic valve stenosis, and by ventricular dilation. When afterload increases, there is an increase in end-systolic volume and a decrease in stroke volume.
How does afterload affect cardiac output?
During this same period, extensive research demonstrated an inverse relationship between afterload and systolic performance, which is accepted today. This means that cardiac output decreases as the afterload on the heart increases and vice versa.
Does increased afterload increase blood pressure?
Aortic insufficiency (Aortic Regurgitation) increases afterload, because a percentage of the blood that ejects forward regurgitates back through the diseased aortic valve. This leads to elevated systolic blood pressure.
Does afterload affect blood pressure?
Afterload is the pressure against which the heart must work to eject blood during systole (systolic pressure). The lower the afterload, the more blood the heart will eject with each contraction. Like contractility, changes in afterload will raise or lower the Starling curve relating stroke volume index to LAP.
What affects preload and afterload?
Contractility is the intrinsic strength of the cardiac muscle independent of preload, but a change in preload will affect the force of contraction. Afterload is the 'load' to which the heart must pump against. Afterload goes down when aortic pressure and systemic vascular resistance decreases through vasodilation.
What is afterload Why is it important to cardiac function?
1.15. Afterload refers to the pressure that the ventricles must generate to pump blood effectively against the resistance in the vascular system. Any condition that increases resistance requires a greater afterload to force open the semilunar valves and pump the blood.
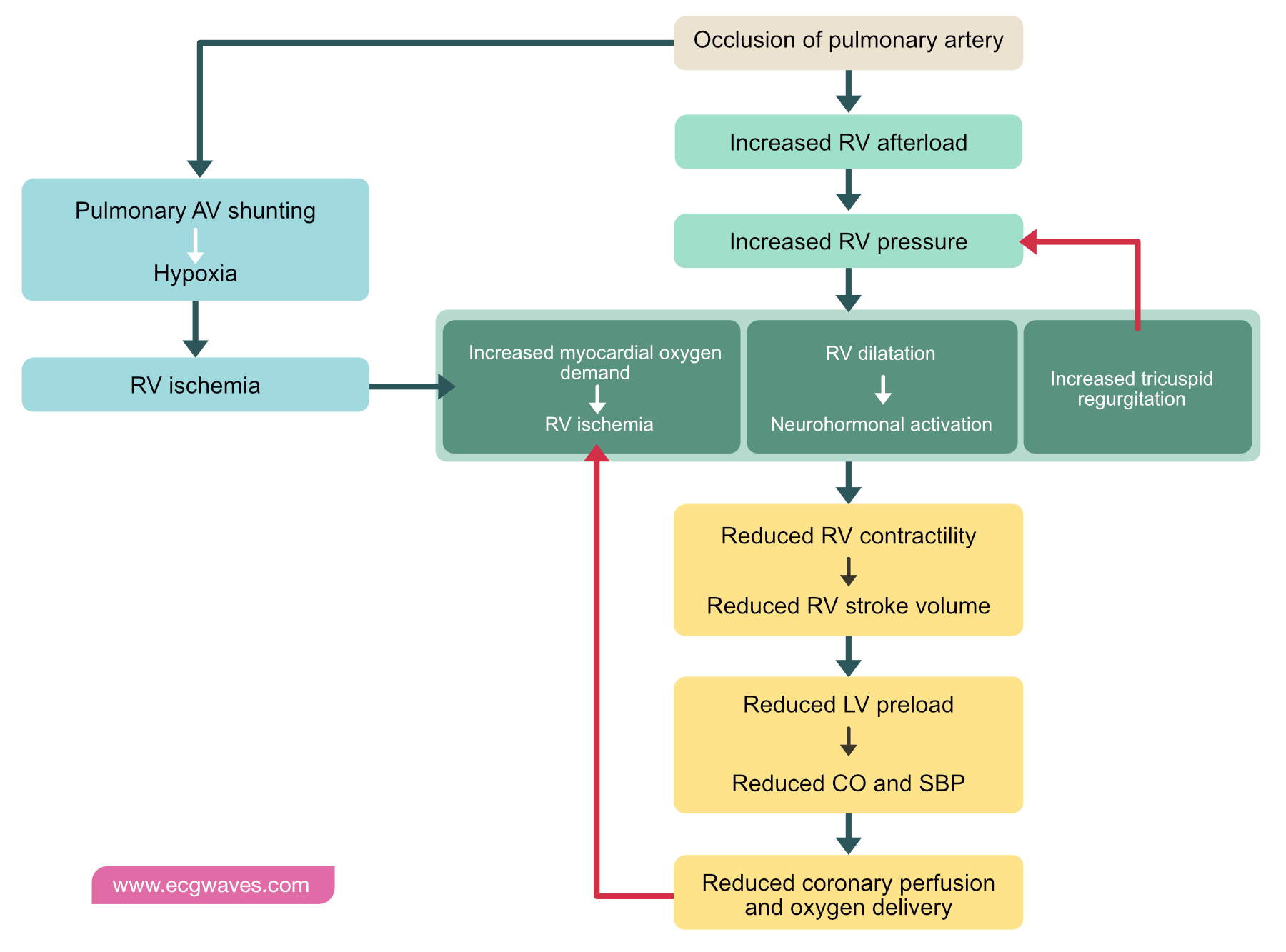
How does increased afterload lead to heart failure?
Afterload is a measure of the force resisting the ejection of blood by the heart. Increased afterload (or aortic pressure, as is observed with chronic hypertension) results in a reduced ejection fraction and increased end-diastolic and end-systolic volumes.
Does afterload affect stroke volume?
An increase in afterload, for example, in individuals with long-standing high blood pressure, generally causes a decrease in stroke volume. [2] In summary, stroke volume may be increased by increasing the contractility or preload or decreasing the afterload.
Does vasodilation increase afterload?
In the setting of systolic failure, judicious vasodilation reduces vascular resistance and, potentially, afterload, allowing stroke volume to increase.
Does afterload increase during exercise?
The increase in arterial pressure (increased ventricular afterload) that normally occurs during exercise tends to diminish the reduction in end-systolic volume; however, the large increase in inotropy is the dominate factor affecting end-systolic volume and stroke volume.
What increases left ventricular afterload?
Thus, left ventricular afterload is increased by left ventricular dilatation and reduced by left ventricular hypertrophy. The transmural left ventricular pressure gradient, and therefore afterload, is increased by high systemic vascular resistance, high arterial blood pressure, and a noncompliant aorta.
What effect does vasodilation have on the afterload?
Vasodilation is when the blood vessels dilate (circumference gets larger) which causes a drop in blood pressure. When this occurs it will affect the afterload by increasing the amount of work placed on the heart due to increased outgoing blood flow from the arterial end of the heart.
What does decreased afterload mean?
Decreased afterload—anything that enhances the ejection of blood out of the heart will decrease both the end-systolic ventricular volume and the end-diastolic ventricular volume. This decreases the preload. Decreased ventricular compliance—anything that makes the heart less stretchy, such as ventricular hypertrophy or impairment ...
How does preload and afterload affect heart failure?
This relationship between preload and afterload is used in the management of heart failure. Drugs like vasodilators will decrease arterial pressure, which will increase stroke volume and reduce the ventricular preload. The left ventricle will be able to eject more blood volume, which leaves less blood in the ventricle after each beat. The ventricle will be able to generate less pressure before it can open the aortic valve and the velocity of ejection will be increased; more blood can be ejected during systole.
How does an afterload reducer work?
An afterload reducer, on the other hand, will attempt to cause afterload reduction by reducing the systemic vascular resistance. This decreases the “load” on the heart, which improves cardiac output. An added advantage to this approach is that many of these drugs will improve renal blood flow, which enhances urinary output and may reduce preload as well.
What is the afterload of the left ventricle?
The afterload is the amount of vascular resistance that must be overcome by the left ventricle to allow blood to flow out of the heart. It is also referred to as the systemic ...
What is the preload of a drug?
The preload is the amount of stretch or pressure left in the left ventricle at the end of diastole—when the heart is the most relaxed. It is also referred to as the left ventricular end-diastolic pressure ...
Why is preload important?
The concepts of preload and afterload are very important to the understanding of cardiovascular medicine and to knowing how to care for patients with compromised hearts due to heart failure. Even so, the two terms can be confusing when it comes to understanding how the heart functions. Let’s take a look at what these terms mean, which things change these values, and which drugs can be used to affect the preload and afterload.
What causes the left ventricle to fill faster?
Decreased heart rate —the slower the heart rate, the greater is the left ventricular filling time with more blood flowing into the heart per diastolic period. Increased pressure in the aorta—this increases the afterload, which will increase the amount of blood left over after contracting the left ventricle.
What is Afterload?
Afterload can be thought of as the "load" that the heart must eject blood against. In simple terms, the afterload of the left ventricle is closely related to the aortic pressure. To appreciate the afterload on individual muscle fibers, afterload is often expressed as ventricular wall stress (σ), where
What is the interaction between afterload and preload?
The interaction between afterload and preload is utilized in the treatment of heart failure , in which vasodilator drugs are used to augment stroke volume by decreasing arterial pressure (afterload), and at the same time reduce ventricular preload.
How does afterload affect ESV?
The effects of afterload on ventricular ESV and EDV can be illustrated using pressure-volume loops (see figure). If afterload is decreased by decreasing arterial pressure as in the example discussed above, the ventricle needs to generate less pressure before the aortic valve opens. The ejection velocity after the valve opens is increased because decreased afterload increases the velocity of cardiac fiber shortening as described by the force-velocity relationship. More blood is ejected (increased stroke volume), which decreases the ventricular ESV as shown in the pressure-volume loop. Because end-systolic volume is decreased, there is less blood within the ventricle to be added to the venous return, which decreases EDV. Ordinarily, in the final steady-state (after several beats), the decrease in EDV is less than the decrease in ESV so that the difference between the two, the stroke volume, is increased (i.e., the width of the pressure-volume loop is increased).
How does afterload affect stroke volume?
As shown in the figure, an increase in afterload shifts the Frank-Starling curve down and to the right (from point A to B), which decreases stroke volume (SV) and at the same time increases left ventricular end-diastolic pressure (LVEDP). The basis for this is found in the force-velocity relationship for cardiac myocytes. Briefly, an increase in afterload decreases the velocity of fiber shortening. Because the period of time available for ejection is finite (~200 msec), a decrease in fiber shortening velocity reduces the rate of volume ejection so that more blood is left within the ventricle at the end of systole (increased end-systolic volume ). In contrast, a decrease in afterload shifts the Frank-Starling curve up and to the left (A to C), which increases SV and at the same time reduces LVEDP.
What happens to afterload when aortic pressure is increased?
When afterload increases, there is an increase in end-systolic volume and a decrease in stroke volume.
Why does the velocity of the ejection of a valve increase after opening?
The ejection velocity after the valve opens is increased because decreased afterload increases the velocity of cardiac fiber shortening as described by the force-velocity relationship . More blood is ejected (increased stroke volume), which decreases the ventricular ESV as shown in the pressure-volume loop.
Does heart rate affect EDV?
Increased heart rate, by reducing filling time, will further decrease in EDV and tend to attenuate the stroke volume increase produced by reducing the afterload. Increased inotropy would tend to further reduce the ESV, further increase the SV, and further reduce EDV.
What is afterload in a muscle?
The afterload of any contracting muscle is defined as the total force that opposes sarcomere shortening minus the stretching force that existed before contraction. Applying this definition to the heart, afterload can be most easily described as the "load" against which the heart ejects blood. The load on individual fibers can be expressed as left ventricular wall stress, which is proportional to [(LV Pressure x LV Radius)/ LV wall thickness], or [(P x r)/h]. However, the true equation is complex because it depends on the shape of the cardiac chamber, which is affected by several factors that are changing over time. Therefore, afterload cannot be represented by a single numerical value or described only regarding pressure. Arterial pressure (diastolic, mean, or systolic) is frequently used as a surrogate measure, but perhaps the best available techniques involve measuring systemic arterial resistance by various invasive and noninvasive methods. Several mathematical models have been developed using arterial impedance and pressure-flow relationships to characterize afterload better, but these are complex and less often utilized in practice. The inverse relationship between afterload and cardiac output is important in understanding the pathophysiology and treatment of several diseases, including aortic stenosis, systemic hypertension, and congestive heart failure. [1][2][3]
How does afterload affect cardiac output?
The relationship between afterload and cardiac output is somewhat intuitive as one would expect the flow to increase as the load against which the heart contracts decreases . Several researchers during the 1960s and 1970s sought to develop this understanding at the cellular level. Experiments by Sonnenblick on isolated cat papillary muscle strips demonstrated that the extent and velocity of muscle shortening decrease as the load on the muscle is increased. A major limitation of this study was its basic design employing the use of isolated muscle strips. Monroe and French overcame this by using isolated whole-preparation dog hearts to show an inverse relationship between peak aortic flow and arterial impedance. Ross et al. took this one step further and examined the effects of changing LV afterload in anesthetized dogs by injecting or withdrawing blood from the aorta between systolic contractions. They reported similar findings to the previous studies giving further support for an inverse relationship between afterload and cardiac output due to alterations in sarcomere shortening. Figure 1 is a graphic representation of the effect of increases or decreases in afterload on the cardiac output, which is illustrated by shifting the baseline Frank-Starling curve downward or upward, respectively. [6][7][8]
How do afterload reduction agents work?
Afterload reduction agents are an essential component in treating congestive heart failure with reduced ejection fraction as these patients have elevated systemic resistance due to the neurohormonal response to the decreased cardiac output. They are also frequently used in the management of systemic hypertension. These drugs typically act by dilating the arterial system, which reduces the total load on the contracting heart and increases systolic performance. The arterial dilators fall under the broader category of vasodilators, consisting of arterial, venous, and mixed-acting drugs. Venous dilators reduce preload by pooling blood in the highly compliant venous system and are an important part of treating angina. The preload reducing properties of venodilators lead to a reduction in cardiac output and arterial pressure. Most drugs have mixed arterial and venous action, and the relative balance between these determines the effect on cardiac output. [11]
How does dihydropyridine affect the heart?
They act by inhibiting the movement of calcium ions into the vascular smooth muscle cells. This has a vasodilatory effect on the vessels leading to a decrease in the systemic vascular resistance of the heart. [13]
What are the independent effects of preload?
Independent Effects of Preload. To examine the independent effects of preload, assume that aortic systolic and diastolic pressure ( afterload ), and inotropy are held constant. The left ventricle is filled with blood from the pulmonary veins. If pulmonary venous flow is increased, the ventricle will fill to a greater extent ...
What happens to the ventricle when the preload is increased?
When muscle preload length is increased, the contracting muscle shortens to the same minimal length as found before the preload was increased (see Effects of Preload on Cardiac Fiber Shortening ). If pulmonary venous flow decreases, then the ventricle will fill to a smaller end-diastolic volume (decreased preload; green loop in figure).
Why is stroke volume reduced?
Stroke volume is reduced because increased afterload reduces the velocity of muscle fiber shortening and the velocity at which the blood is ejected ( see force-velocity relationship ). A reduced stroke volume at the same end-diastolic volume results in reduced ejection fraction. If afterload is reduced by decreasing aortic pressure, ...
Why is the isovolumetric contraction phase prolonged?
If afterload is increased by increasing aortic pressure, the isovolumetric contraction phase is prolonged because the ventricle will need to generate a higher pressure to overcome the elevated aortic diastolic pressure. Therefore, ejection begins at a higher aortic diastolic pressure. If preload (end-diastolic volume) and inotropy are held ...
How does inotropy affect muscle fibers?
Increasing inotropy increases the velocity of muscle fiber shortening at any given preload and afterload (see force-velocity relationship ). This enables the ventricle to increase the rate of pressure development and ejection velocity, which leads to an increase in stroke volume and ejection fraction, and a decrease in end-systolic volume (red loop in figure). In PV loop diagrams, increased inotropy increases the slope of the end-systolic pressure-volume relationship (ESPVR; upper dashed lines in figure), which permits the ventricle to generate more pressure at a given LV volume. Decreasing inotropy has the opposite effects; namely, increased end-systolic volume and decreased stroke volume and ejection fraction (green loop in figure).
Why are PV loops important?
Ventricular pressure-volume (PV) loops are an excellent tool for visualizing changes in ventricular function in response to changes in preload, afterload and inotropy. These ventricular changes can be complex because preload, afterload and inotropy are interdependent variables, meaning that when one variable is changed, the other variables change.
Why does end diastolic volume increase?
For example, increasing end-diastolic volume leads to a small increase in end-systolic volume because of increased wall stress (afterload) at end-diastole.
What happens to afterload in animals?
As aortic and pulmonary pressures increase, the afterload increases on the left and right ventricles respectively. Afterload changes to adapt to the continually changing demands on an animal's cardiovascular system. Afterload is proportional to mean systolic blood pressure and is measured in millimeters of mercury (mm Hg) .
What is afterload in hemodynamics?
Hemodynamics. Afterload is a determinant of cardiac output. Cardiac output is the product of stroke volume and heart rate. Afterload is a determinant of stroke volume (in addition to preload, and strength of myocardial contraction ). Following Laplace's law, the tension upon the muscle fibers in the heart wall is the pressure within ...
What is afterload in cardiac imaging?
Afterload can also be described as the pressure that the chambers of the heart must generate to eject blood from the heart, and this is a consequence of aortic pressure (for the left ventricle) and pulmonic pressure or pulmonary artery pressure (for the right ventricle). The pressure in the ventricles must be greater than the systemic and pulmonary pressure to open the aortic and pulmonic valves, respectively. As afterload increases, cardiac output decreases. Cardiac imaging is a somewhat limited modality in defining afterload because it depends on the interpretation of volumetric data.
Why does systolic hypertension increase afterload?
Systolic hypertension (HTN) (elevated blood pressure) increases the left ventricular (LV) afterload because the LV must work harder to eject blood into the aorta. This is because the aortic valve won' t open until the pressure generated in the left ventricle is higher than the elevated blood pressure in the aorta.
Why does aortic regurgitation increase afterload?
Aortic insufficiency (Aortic Regurgitation) increases afterload, because a percentage of the blood that ejects forward regurgitates back through the diseased aortic valve. This leads to elevated systolic blood pressure. The diastolic blood pressure in the aorta falls, due to regurgitation.
Why does the left ventricle have a higher afterload?
Thus, in the long-term, increased afterload (due to the stenosis) results in hypertrophy of the left ventricle to account for the increased work required.
How to calculate afterload?
Quantitatively, afterload can be calculated by determining the wall stress of the left ventricle, using the Young–Laplace equation: EDP is end diastolic pressure in the left ventricle, which is typically approximated by taking pulmonary artery wedge pressure ,
What factors affect afterload?
Factors which affect afterload: valve resistance, vascular resistance, vascular impedance, blood viscosity, intrathoracic pressure, and the relationship of ventricular radius and volume. Determinants which are specific to the right and left ventricles.
What is afterload in a heart?
Afterload can be defined as the resistance to ventricular ejection - the "load" that the heart must eject blood against. It consists of two main sets of determinant factors: P, the ventricular transmural pressure, which is the difference between the intrathoracic pressure and the ventricular cavity pressure.
What are the components of afterload?
The two main components of afterload overlap in the territory of pressure, specifically the aortic pressure to which the ventricle is exposed when the aortic valve opens in systole. At this stage, ventricular chamber pressure and aortic pressure are approximately equal, and their pressure/time waveforms are essentially superimposable (well, allowing for some resistance from the ventricular outflow tract). This combined "aortoventricular" pressure is a major determinant of ventricular wall stress, and is in turn determined by the factors which govern aortic input impedance. Thus, the hydraulic definition of afterload can be turned into one of the components of the Laplace definition, provided we avert our gaze from certain elements which do not fit this narrative (eg. pulsatile flow).
Why does intrapleural pressure decrease afterload?
Positive intrapleural pressure decreases afterload because of a decreased LV transmural pressure (it is subtracted from the intra-LV pressure)
Does stiffness affect the aorta?
Increased stiffness is not only a phenomenon which affects the aorta. Distal peripheral arteries can also become stiffened and contribute to afterload, but they do so by a different mechanism. Decreased peripheral arterial compliance causes an increase in the pulse wave velocity, which means that the reflected wave from the distal circulation arrives too early - during systole - and contributes to the afterload.
Is Laplace inadequate to describe afterload?
For lots of reasons other than the non-spherical shape of a ventricle, the Laplace definition is by istelf inadequate to describe afterload. To quote Milnor (1975),
Does inertia increase afterload?
It increases afterload in early systole. Inertia is a force which opposes the acceleration of blood flow, which is maximal during early systole. At the beginning of systole, during isovolumetric contraction, the stroke volume is at rest, and so is the mass of blood in the aorta.
What happens when the afterload is elevated?
Chronic elevation of the afterload leads to pathologic cardiac structural changes including left ventricular hypertrophy. Eventually this results in diastolic dysfunction and symptoms of diastolic congestive heart failure.
What is afterload in a hemodynamics?
Afterload is the hemodynamic parameter that reflects the force that the left ventricle has to overcome to eject blood through the aortic valve. The most common pathologic process that increases afterload is systemic hypertension. Other situations that increase afterload include aortic stenosis (including subvalvular and supravalvular), aortic ...
What is the hemodynamic parameter that reflects the force that the left ventricle has to overcome to eject?
Afterload is the hemodynamic parameter that reflects the force that the left ventricle has to overcome to eject blood through the aortic valve.
