
- 1. Vessel spasm (vasoconstriction)
- 2. Platelet Plug (adheres to damaged wall)
- 3. Clot Formation (fibrin forms meshwork)
- 4.Clot retraction (platelets contast pulling broken vessels together)
- 5.Clot dissolution (fibribolysos removes clot)
- Vessel Spasm. ...
- Formation of Platelet Plug. ...
- Blood Coagulation. ...
- Clot Retraction. ...
- Clot Dissolution (Lysis)
What is the first step in the hemostasis process?
Hemostasis. Vascular spasm is the first response as the blood vessels constrict to allow less blood to be lost. In the second step, platelet plug formation, platelets stick together to form a temporary seal to cover the break in the vessel wall. The third and last step is called coagulation or blood clotting.
What are the 4 stages of hemostasis?
Stages. The mechanism of hemostasis can divide into four stages. 1) Constriction of the blood vessel. 2) Formation of a temporary “platelet plug." 3) Activation of the coagulation cascade. 4) Formation of “fibrin plug” or the final clot.
What are the three steps of haemostasis?
There are three steps to the process: vascular spasm, the formation of a platelet plug, and coagulation (blood clotting). Failure of any of these steps will result in haemorrhage —excessive bleeding. The vascular response and platelet plug formation are referred to as primary haemostasis and coagulation is referred to a secondary haemostasis.
What are the three steps of blood clotting?
Blood clotting involves three steps. First, vascular spasm constricts the flow of blood. Next, a platelet plug forms to temporarily seal small openings in the vessel. Coagulation then enables the repair of the vessel wall once the leakage of blood has stopped.

What are the 5 events of hemostasis?
The mechanism of hemostasis can divide into four stages. 1) Constriction of the blood vessel. 2) Formation of a temporary “platelet plug." 3) Activation of the coagulation cascade. 4) Formation of “fibrin plug” or the final clot.
What is hemostasis and its steps?
Hemostasis is the physiological process by which bleeding ceases. Hemostasis involves three basic steps: vascular spasm, the formation of a platelet plug, and coagulation, in which clotting factors promote the formation of a fibrin clot. Fibrinolysis is the process in which a clot is degraded in a healing vessel.
What is the last step of hemostasis?
Fibrin clot remodeling The last stage of hemostasis is when your body remodels the existing clot into a fibrin clot. Your body does that because blood clots are a temporary patch, not a permanent solution. That removal involves a process called fibrinolysis.
What are the five steps involved in blood clotting?
Here's how the process works:Injury. A cut on the skin or an internal injury creates a small tear in a blood vessel wall, which causes blood flow.Vessel constriction. ... Platelet plug. ... Fibrin clot.
What are the steps of hemostasis quizlet?
Hemostasis is the natural process that stops blood loss when an injury occurs.It involves three steps: (1) vascular spasm (vasoconstriction); (2) platelet plug formation; and (3) coagulation.
What are the types of hemostasis?
Hemostasis can be subdivided into three sequential processes: primary hemostasis, secondary hemostasis, and tertiary hemostasis. In primary hemostasis the interaction of the injured endothelium with von Willebrand factor (VWF), and platelets is crucial for the formation of a platelet plug at the injury site.
What is primary hemostasis?
Primary hemostasis serves to immediately limit bleeding through the formation of a loose platelet plug. Platelets play a key role in the rapid response to blood vessel injury by: Adhering to the endothelial wall at the site of injury. Releasing potent anticoagulant compounds. Aggregating to form a plug.
What is activated first in haemostasis?
Vascular spasm is the first response as the blood vessels constrict to allow less blood to be lost. In the second step, platelet plug formation, platelets stick together to form a temporary seal to cover the break in the vessel wall. The third and last step is called coagulation or blood clotting.
Which of the following occurs first in hemostasis?
Hemostasis includes three steps that occur in a rapid sequence: (1) vascular spasm, or vasoconstriction, a brief and intense contraction of blood vessels; (2) formation of a platelet plug; and (3) blood clotting or coagulation, which reinforces the platelet plug with fibrin mesh that acts as a glue to hold the clot ...
What is the first stage of homeostasis quizlet?
The first step in hemostasis is: platelet plug formation.
What is the difference between homeostasis and Haemostasis?
Hemostasis and homeostasis are two different things. Hemostasis is the stopping of bleeding from a wound, which is often the first stage of wound healing. Homeostasis is the body's state of balance, or it's tendency to maintain a constant, stable state in the body.
What is hemostasis in biology?
Abstract. Physiological hemostasis is an intricate biological system, where procoagulant and anticoagulant forces interplay and preserves blood fluidity when blood vessels are intact, or trigger clot formation to prevent excessive bleeding when blood vessels are injured.
What is hemostasis in biology?
Abstract. Physiological hemostasis is an intricate biological system, where procoagulant and anticoagulant forces interplay and preserves blood fluidity when blood vessels are intact, or trigger clot formation to prevent excessive bleeding when blood vessels are injured.
What's the meaning of haemostatic?
retarding or stopping the flow of blood within/ (ˌhiːməʊˈstætɪk, ˌhɛm-) / adjective. retarding or stopping the flow of blood within the blood vessels. retarding or stopping bleeding.
What is hemostasis PDF?
Haemostasis means “arrest of bleeding”. During haemostasis several mechanisms. interact to slow blood flow, block the vessel wall defect with a platelet plug. (primary haemostasis), convert fibrinogen to a jelly like fibrin clot (coagulation. of blood) and later re-establish the flow of blood through a mechanism of ...
What is the cause of hemostasis?
Hemostasis occurs when blood is present outside of the body or blood vessels. It is the innate response for the body to stop bleeding and loss of blood. During hemostasis three steps occur in a rapid sequence. Vascular spasm is the first response as the blood vessels constrict to allow less blood to be lost.
What is hemostasis?from my.clevelandclinic.org
Hemostasis is your body’s normal reaction to an injury that causes bleeding. This reaction stops bleeding and allows your body to start repairs on the injury. This capability is essential to keep you alive, particularly with significant injuries. However, in uncommon cases, the processes that control hemostasis can malfunction, causing potentially serious — or even dangerous — problems with bleeding or clotting.
How does hemostasis work?from my.clevelandclinic.org
Hemostasis combines the terms “hemo” (meaning “blood”) and “stasis” (meaning “standing still”). In this context, it’s the term for how your body stops bleeding. Rather than being just a single process, hemostasis is actually a collection of several processes. Though they look like separate processes, these all happen at the same time when your body forms a blood clot.
What causes hemostasis?from my.clevelandclinic.org
Without normal hemostasis, even minor injuries could cause dangerous blood loss. An example of this is hemophilia, a condition where hemostasis doesn't work properly and blood can't clot effectively. Any break in your skin is also a risk for germs to enter your body. Clots help reduce that risk by sealing the injury.
How are hemostasis problems diagnosed?from my.clevelandclinic.org
A healthcare provider — such as a hematologist — can diagnose blood clotting problems based on your symptoms and blood tests that analyze the clotting-related components in a sample of your blood.
When should I call a doctor about problems with clotting?from my.clevelandclinic.org
Hypercoagulability can happen with a variety of different symptoms depending on where and when an abnormal clot develops . Examples of this include:
How do platelets form a plug?from en.wikipedia.org
This process is regulated through thromboregulation. Plug formation is activated by a glycoprotein called Von Willebrand factor (vWF), which is found in plasma. Platelets play one of major roles in the hemostatic process. When platelets come across the injured endothelium cells, they change shape, release granules and ultimately become ‘sticky’. Platelets express certain receptors, some of which are used for the adhesion of platelets to collagen. When platelets are activated, they express glycoprotein receptors that interact with other platelets, producing aggregation and adhesion. Platelets release cytoplasmic granules such as adenosine diphosphate (ADP), serotonin and thromboxane A2. Adenosine diphosphate (ADP) attracts more platelets to the affected area, serotonin is a vasoconstrictor and thromboxane A2 assists in platelet aggregation, vasoconstriction and degranulation. As more chemicals are released more platelets stick and release their chemicals; creating a platelet plug and continuing the process in a positive feedback loop. Platelets alone are responsible for stopping the bleeding of unnoticed wear and tear of our skin on a daily basis. This is referred to as primary hemostasis.
How do platelets stick together?from hemostasis.com
This process is regulated through thromboregulation. Platelets play one of the biggest factors in the hemostatic process. Being the second step in the sequence they stick together (aggregation) to form a plug that temporarily seals the break in the vessel wall. As platelets adhere to the collagen fibers of a wound they become spiked and much stickier. They then release chemical messengers such as adenosine diphosphate (ADP), serotonin and thromboxane A2. These chemicals are released to cause more platelets to stick to the area and release their contents and enhance vascular spasms. As more chemicals are released more platelets stick and release their chemicals; creating a platelet plug and continuing the process in a positive feedback loop. Platelets alone are responsible for stopping the bleeding of unnoticed wear and tear of our skin on a daily basis.
What is the role of coagulation in hemostatic hemostasis?
Coagulation reinforces the platelet plug with fibrin threads that act as a “molecular glue”. Platelets are a large factor in the hemostatic process. They allow for the creation of the “platelet plug” that forms almost directly after a blood vessel has been ruptured.
What is the first response to a vascular spasm?
Vascular spasm is the first response as the blood vessels constrict to allow less blood to be lost. In the second step, platelet plug formation, platelets stick together to form a temporary seal to cover the break in the vessel wall. The third and last step is called coagulation or blood clotting.
How do clots form?
3. Blood coagulation – Clots form upon the conversion of fibrinogen to fibrin, and its addition to the platelet plug ( secondary hemostasis ). Coagulation: The third and final step in this rapid response reinforces the platelet plug. Coagulation or blood clotting uses fibrin threads that act as a glue for the sticky platelets. As the fibrin mesh begins to form the blood is also transformed from a liquid to a gel like substance through involvement of clotting factors and pro-coagulants. The coagulation process is useful in closing up and maintaining the platelet plug on larger wounds. The release of Prothrombin also plays an essential part in the coagulation process because it allows for the formation of a thrombus, or clot, to form. This final step forces blood cells and platelets to stay trapped in the wounded area. Though this is often a good step for wound healing, it has the ability to cause severe health problems if the thrombus becomes detached from the vessel wall and travels through the circulatory system; If it reaches the brain, heart or lungs it could lead to stroke, heart attack, or pulmonary embolism respectively. However, without this process the healing of a wound would not be possible.
How do platelets help with hemostatic process?
This process is regulated through thromboregulation. Platelets play one of the biggest factors in the hemostatic process. Being the second step in the sequence they stick together (aggregation) to form a plug that temporarily seals the break in the vessel wall.
How does hemostasis occur?
Hemostasis occurs when blood is present outside of the body or blood vessels. It is the instinctive response for the body to stop bleeding and loss of blood. During hemostasis three steps occur in a rapid sequence. Vascular spasm is the first response as the blood vessels constrict to allow less blood to be lost. In the second step, platelet plug formation, platelets stick together to form a temporary seal to cover the break in the vessel wall. The third and last step is called coagulation or blood clotting. Coagulation reinforces the platelet plug with fibrin threads that act as a “molecular glue”. Platelets are a large factor in the hemostatic process. They allow for the creation of the “platelet plug” that forms almost directly after a blood vessel has been ruptured. Within seconds of a blood vessel’s epithelial wall being disrupted platelets begin to adhere to the sub-endotheliumsurface. It takes approximately sixty seconds until the first fibrin strands begin to intersperse among the wound. After several minutes the platelet plug is completely formed by fibrin. Hemostasis is maintained in the body via three mechanisms:
Why do people develop hemostasis?
Hemostasis disorders can develop for many different reasons. They may be congenital, due to a deficiency or defect in an individual’s platelets or clotting factors. A number of disorders can be acquired as well.
What are the steps of hemostasis?
Hemostasis has three major steps: 1) vasoconstriction, 2) temporary blockage of a break by a platelet plug, and 3) blood coagulation, or formation of a fibrin clot. These processes seal the hole until tissues are repaired.
Where does clotting factor III come from?
Endothelium. Clotting factors III and VIII originate from the endothelial cells while the clotting factor IV comes from the plasma. [2][3]Factor III, IV, and VIII all undergo K dependent gamma-carboxylation of their glutamic acid residues, which allows for binding with calcium and other ions while in the coagulation pathway. [4]
What is the mechanism that leads to cessation of bleeding from a blood vessel?
Introduction. Definition. Hemostasis is the mechanism that leads to cessation of bleeding from a blood vessel. It is a process that involves multiple interlinked steps. This cascade culminates into the formation of a “plug” that closes up the damaged site of the blood vessel controlling the bleeding. It begins with trauma to the lining of the blood ...
What is hemostasis in physiology?
Physiology, Hemostasis - StatPearls - NCBI Bookshelf. Definition. Hemostasis is the mechanism that leads to cessation of bleeding from a blood vessel. It is a process that involves multiple interlinked steps.
What is the hemostatic cascade?
The hemostatic cascade is meant to control hemorrhage and be a protective mechanism. At times, this process is triggered inadvertently while the blood is within the lumen of the blood vessel and without any bleeding.[1]
What is the process of hemostasis?
It begins with trauma to the lining of the blood vessel. Definition. Hemostasis is the mechanism that leads to cessation of bleeding from a blood vessel. It is a process that involves multiple interlinked steps. This cascade culminates into the formation of a “plug” that closes up the damaged site of the blood vessel controlling the bleeding.
What to monitor after cardiac stenting?
For patients after cardiac stenting or stroke to monitor the activity of the antiplatelet agents
What is NCBI bookshelf?
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
How do platelets bind to collagen?
In the second step, platelets, which normally float free in the plasma, encounter the area of vessel rupture with the exposed underlying connective tissue and collagenous fibers. The platelets begin to clump together, become spiked and sticky, and bind to the exposed collagen and endothelial lining. This process is assisted by a glycoprotein in the blood plasma called von Willebrand factor, which helps stabilize the growing platelet plug. As platelets collect, they simultaneously release chemicals from their granules into the plasma that further contribute to hemostasis. Among the substances released by the platelets are: 1 adenosine diphosphate (ADP), which helps additional platelets to adhere to the injury site, reinforcing and expanding the platelet plug 2 serotonin, which maintains vasoconstriction 3 prostaglandins and phospholipids, which also maintain vasoconstriction and help to activate further clotting chemicals, as discussed next
How does blood clotting work?
Blood clotting involves three steps. First , vascular spasm constricts the flow of blood. Next, a platelet plug forms to temporarily seal small openings in the vessel. Coagulation then enables the repair of the vessel wall once the leakage of blood has stopped.
What is the role of platelets in hemostasis?
Platelets are key players in hemostasis, the process by which the body seals a ruptured blood vessel and prevents further loss of blood. Although rupture of larger vessels usually requires medical intervention, hemostasis is quite effective in dealing with small, simple wounds. There are three steps to the process: vascular spasm, ...
Why administer a thrombolytic agent?
Explain why administration of a thrombolytic agent is a first intervention for someone who has suffered a thrombotic stroke. In a thrombotic stroke, a blood vessel to the brain has been blocked by a thrombus, an aggregation of platelets and erythrocytes within a blood vessel.
What happens when platelets float in the plasma?
In the second step, platelets, which normally float free in the plasma, encounter the area of vessel rupture with the exposed underlying connective tissue and collagenous fibers. The platelets begin to clump together, become spiked and sticky, and bind to the exposed collagen and endothelial lining.
How many clotting factors are there?
The 12 clotting factors are numbered I through XIII according to the order of their discovery. Factor VI was once believed to be a distinct clotting factor, but is now thought to be identical to factor V. Rather than renumber the other factors, factor VI was allowed to remain as a placeholder and also a reminder that knowledge changes over time.
How does a vascular spasm occur?
When a vessel is severed or punctured, or when the wall of a vessel is damaged, vascular spasm occurs. In vascular spasm, the smooth muscle in the walls of the vessel contracts dramatically. This smooth muscle has both circular layers; larger vessels also have longitudinal layers. The circular layers tend to constrict the flow of blood, whereas the longitudinal layers, when present, draw the vessel back into the surrounding tissue, often making it more difficult for a surgeon to locate, clamp, and tie off a severed vessel. The vascular spasm response is believed to be triggered by several chemicals called endothelins that are released by vessel-lining cells and by pain receptors in response to vessel injury. This phenomenon typically lasts for up to 30 minutes, although it can last for hours.
What is the process of hemostasis?
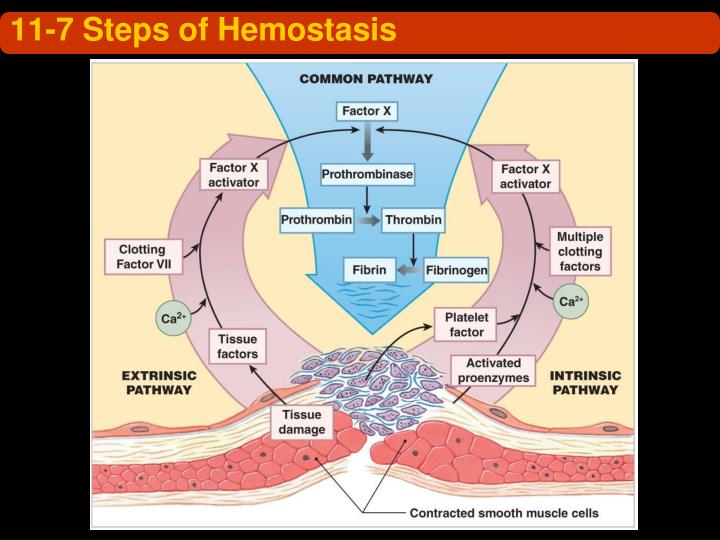
Figure 5.5.1. Haemostasis. (a) An injury to a blood vessel initiates the process of haemostasis. Blood clotting involves three steps. First, vascular spasm slows the flow of blood. Next, a platelet plug forms to temporarily seal small openings in the vessel. Coagulation then enables the repair of the vessel wall once the leakage of blood has stopped. (b) The synthesis of fibrin in blood clots involves both an intrinsic pathway and an extrinsic pathway, both of which lead to a common pathway. (credit a: Kevin MacKenzie).
What is the role of platelets in hemostasis?
Platelets are key players in haemostasis, the process by which the body seals a ruptured blood vessel and prevents further loss of blood. Although rupture of larger vessels usually requires medical intervention, haemostasis is quite effective in dealing with small, simple wounds and small internal bleeds. There are three steps to the process: vascular spasm, the formation of a platelet plug, and coagulation (blood clotting). Failure of any of these steps will result in haemorrhage —excessive bleeding. The vascular response and platelet plug formation are referred to as primary haemostasis and coagulation is referred to a secondary haemostasis.
What are plasma proteins called?
In the coagulation cascade, plasma proteins called clotting factors (or coagulation factors) prompt reactions that activate still more coagulation factors. The process is complex, but is initiated along two basic pathways:
How does a clot contract?
The stabilised clot undergoes contraction via the action of contractile proteins within platelets. As these proteins contract, they pull on the fibrin threads, bringing the edges of the clot more tightly together, somewhat as we do when tightening loose shoelaces. This process also wrings out of the clot a small amount of fluid called serum, which is blood plasma without its clotting factors.
What is the role of platelets in blood vessel damage?
In the second step, platelets, which normally float free in the plasma, encounter exposed underlying connective tissue and collagenous fibres at the site of blood vessel damage. The platelets bind (adhesion) to the exposed collagen and become activated. Activated platelets are spiked and sticky and bind to other activated platelets (aggregation) and the endothelial lining. Platelet adhesion is assisted by a glycoprotein released from neighbouring endothelial cells called von Willebrand factor, which helps stabilise the growing platelet plug. Platelet aggregation is aided by the plasma protein, fibrinogen, which forms bridges between adjacent platelets at the site of bleed vessel damage. As platelets collect, they simultaneously release chemicals from their granules into the plasma that further contribute to haemostasis. Among the substances released by the platelets are:
What is the process of coagulation?
Those more sophisticated and more durable repairs are collectively called coagulation, the formation of a blood clot. The process is sometimes characterised as a cascade, because one event prompts the next as in a multi-level waterfall. The result is the production of a gelatinous but robust clot made up of a mesh of fibrin —an insoluble filamentous protein derived from fibrinogen, the plasma protein introduced earlier—in which platelets and blood cells are trapped. Figure 5.5.1 summarises the three steps of haemostasis.
How does fibrinolysis work?
Like coagulation, fibrinolysis involves a fairly complicated series of protein catabolising reactions. During this process, the inactive protein plasminogen, released by endothelial cells around the site of blood vessel damage, is converted into the active enzyme plasmin, which gradually breaks down the fibrin of the clot. Additionally, bradykinin, a vasodilator, released from damaged tissues as a pain signal, reverses the effects of the serotonin and prostaglandins secreted by the platelets. This allows the smooth muscle in the walls of the vessels to relax and helps to restore the circulation.
What is hemostasis?from my.clevelandclinic.org
Hemostasis is your body’s normal reaction to an injury that causes bleeding. This reaction stops bleeding and allows your body to start repairs on the injury. This capability is essential to keep you alive, particularly with significant injuries. However, in uncommon cases, the processes that control hemostasis can malfunction, causing potentially serious — or even dangerous — problems with bleeding or clotting.
How does hemostasis work?from my.clevelandclinic.org
Hemostasis combines the terms “hemo” (meaning “blood”) and “stasis” (meaning “standing still”). In this context, it’s the term for how your body stops bleeding. Rather than being just a single process, hemostasis is actually a collection of several processes. Though they look like separate processes, these all happen at the same time when your body forms a blood clot.
What causes hemostasis?from my.clevelandclinic.org
Without normal hemostasis, even minor injuries could cause dangerous blood loss. An example of this is hemophilia, a condition where hemostasis doesn't work properly and blood can't clot effectively. Any break in your skin is also a risk for germs to enter your body. Clots help reduce that risk by sealing the injury.
How are hemostasis problems diagnosed?from my.clevelandclinic.org
A healthcare provider — such as a hematologist — can diagnose blood clotting problems based on your symptoms and blood tests that analyze the clotting-related components in a sample of your blood.
When should I call a doctor about problems with clotting?from my.clevelandclinic.org
Hypercoagulability can happen with a variety of different symptoms depending on where and when an abnormal clot develops . Examples of this include:
How do stabilized clots work?from pressbooks-dev.oer.hawaii.edu
The stabilized clot is acted upon by contractile proteins within the platelets. As these proteins contract, they pull on the fibrin threads, bringing the edges of the clot more tightly together, somewhat as we do when tightening loose shoelaces (see [link] a ). This process also wrings out of the clot a small amount of fluid called serum, which is blood plasma without its clotting factors.
How do platelets stick together?from hemostasis.com
This process is regulated through thromboregulation. Platelets play one of the biggest factors in the hemostatic process. Being the second step in the sequence they stick together (aggregation) to form a plug that temporarily seals the break in the vessel wall. As platelets adhere to the collagen fibers of a wound they become spiked and much stickier. They then release chemical messengers such as adenosine diphosphate (ADP), serotonin and thromboxane A2. These chemicals are released to cause more platelets to stick to the area and release their contents and enhance vascular spasms. As more chemicals are released more platelets stick and release their chemicals; creating a platelet plug and continuing the process in a positive feedback loop. Platelets alone are responsible for stopping the bleeding of unnoticed wear and tear of our skin on a daily basis.
What happens when a blood clot forms?
Once the clot is formed, the platelets gradually contract and ooze out the serum. This leads to shrinkage of the clot with clear fluid on the surface. As the clot retracts (shrinks) the edges of damaged blood vessel tissue are pulled together leading to the closure of the hole.
What is the process of breaking down a blood clot?
Fibrinolysis. This is a healing process of the damaged blood vessel. This phase begins with the breakdown of the clot. The clot is broken down by the enzyme plasmin which is an activated form of plasminogen. This plasmin converts insoluble fibrin to soluble form which is removed byphagocytosis.
How long does it take for a thrombocyte to form a platelet plug?
Many thrombocytes arrive at the injured site due to a positive feedback system to form a platelet plug or seal. This plug formation occurs in 6 minutes and prevents further leakage of blood from the injured site.
What is the function of serotonin in platelets?
This serotonin constricts the blood vessel intended to slow the flow of blood. Besides this, the damaged vessel tissue also releases other vasoconstricting agents like thromboxane.
Which enzyme converts fibrinogen into insoluble fibrin threads?
This prothrombin activator activates the enzyme thrombin which converts fibrinogen into insoluble fibrin threads.
How many factors are involved in the formation of prothrombin?
This process involves 12 factors that go on to the formation of a prothrombin activator. The factors are termed clotting factors and are listed below.
Why does the injured blood vessel's channel get narrow?
In these stages, the injured blood vessel’s channel gets narrow so as to minimize the blood flow.
Introduction
Mechanism
- Hemostasis occurs when blood is present outside of the body or blood vessels. It is the instinctive response for the body to stop bleeding and loss of blood. During hemostasis three steps occur in a rapid sequence. Vascular spasm is the first response as the blood vessels constrict to allow less blood to be lost. In the second step, platelet plug f...
Function
- 2. Platelet plug formation Platelets adhere to damaged endothelium to form platelet plug (primary hemostasis) and then degranulate. This process is regulated through thromboregulation. Platelets play one of the biggest factors in the hemostatic process. Being the second step in the sequence they stick together (aggregation) to form a plug that temporarily seals the break in th…
Pathophysiology
- The second stage of hemostasis involves platelets that move throughout the blood. When the platelets find an exposed area or an injury, they begin to form what is called a platelet plug. The platelet plug formation is activated by a glycoprotein called the Von Willebrand factor (vWF), which are found in the bodys blood plasma. When the platelets in the blood are activated, they t…
Clinical significance
- DISORDERS The bodys hemostasis system requires careful regulation in order to work properly. If the blood does not clot sufficiently, it may be due to bleeding disorders such ashemophilia; this requires careful investigation. Over-active clotting can also cause problems; thrombosis, where blood clots form abnormally, can potentially causeembolisms, where blood clots break off and s…
Causes
- Hemostasis disorders can develop for many different reasons. They may be congenital, due to a deficiency or defect in an individuals platelets or clotting factors. A number of disorders can be acquired as well.