Five Basic Mechanisms of Antibiotic Action against Bacterial Cells: Inhibition of Cell Wall Synthesis (most common mechanism) Inhibition of Protein Synthesis (Translation) (second largest class) Alteration of Cell Membranes Inhibition of Nucleic Acid Synthesis
What is the mechanism of action of anti- inflammatory drugs?
Nonsteroidal anti-inflammatory drugs (NSAIDs) produce their therapeutic activities through inhibition of cyclooxygenase (COX), the enzyme that makes prostaglandins (PGs). They share, to a greater or lesser degree, the same side effects, including gastric and renal toxicity. Recent research has shown that there are at least two COX isoenzymes.
What is the mechanism of antibody action?
What are the 4 major mechanisms of antibody action? Complement Activation Destroy microbes by causing phagocytosis, cytolysis and inflammation Neutralization Neutralized toxin. Prevent attachment of antigen to body cells Precipitation Dissolves antigens
What does mechanism of action mean?
mechanism of action noun. The mechanism by which a pharmacologically active substance produces an effect on a living organism or in a biochemical system; as, the mechanism of action of actinomycin involves its binding to DNA. The mechanism of action is usually considered to include an identification of the specific molecular targets to which a pharmacologically active substance binds or whose biochemical action it influences; a general recognition of the broad biochemical pathways (such as ...
What is the mode of action of antibiotics?
Mode of action β-lactam antibiotics are bacteriocidal, and act by inhibiting the synthesis of the peptidoglycan layer of bacterial cell walls. The peptidoglycan layer is important for cell wall structural integrity, especially in Gram-positive organisms, being the outermost and primary component of the wall.
What are the mechanisms of action of antibiotics?
Inhibition of Cell Wall Synthesis (most common mechanism) Inhibition of Protein Synthesis (Translation) (second largest class) Alteration of Cell Membranes. Inhibition of Nucleic Acid Synthesis.
What are the mechanisms in which antibiotics affect bacterial growth?
The biochemical resistance mechanisms used by bacteria include the following: antibiotic inactivation, target modification, altered permeability, and “bypass” of metabolic pathway.
What are the 5 mechanisms of drug resistance?
Mechanisms for Drug ResistanceDrug Modification or Inactivation. ... Prevention of Cellular Uptake or Efflux. ... Target Modification. ... Target Overproduction or Enzymatic Bypass. ... Target Mimicry.
What mechanisms are responsible for antibiotic resistance?
The three fundamental mechanisms of antimicrobial resistance are (1) enzymatic degradation of antibacterial drugs, (2) alteration of bacterial proteins that are antimicrobial targets, and (3) changes in membrane permeability to antibiotics.
What are the 4 classes of antibiotics based on mode of action?
According to their primary actions on sensible cells the antimicrobial antibiotics are divided into four groups: 1. Inhibitors of the biosynthesis of the bacterial cell wall 2. Inhibitors of the bacterial protein synthesis 3. Inhibitors of the nucleic acid metabolism 4.
What are the 4 classes of antibiotics?
Antibiotic class defines a set of related antibiotics. State-level rates of penicillins, macrolides, cephalosporins, and fluoroquinolones are displayed. Also displayed are all antibiotic classes, which include these four classes plus additional classes not available for release at the state level.
What are the mechanisms of antibiotic action?
Mechanisms of Antibiotic Action. Antibiotics are used in medicine and agriculture against bacterial infections and bacterial growth in food. There are several classes of antibiotic, and this article explains the bacteriocidal or bacteriostatic activity of each.
How do tetracyclines inhibit protein synthesis?
Tetracyclines inhibit synthesis of proteins by binding to the 30S ribosome subunit but have a different method of action to aminoglycosides. Instead of preventing proof-reading of the peptide produced, they stop the binding of tRNA to the ribosome, stopping protein synthesis.
What prevents the production of proteins by bacteria?
Preventing the binding of tRNA to the bacterial ribosome effectively prevents proteins being produced by the bacteria, leading to its death.
What are aminoglycosides?
Aminoglycosides. Aminoglycosides are bacteriostatic; they slow down the growth and reproduction of bacteria without killing them. These antibiotics inhibit the synthesis of proteins by binding to the 30S bacterial ribosome subunit. When these subunits bind together, they produce the proteins needed by the cell.
What subunits are ribosomes made of?
When these subunits bind together, they produce the proteins needed by the cell. Ribosomes in animal cells are 80S, made of subunits of 40S and 60S, while bacterial ribosomes are 70S, so specific modification in bacterial ribosome can be achieved.
When to use cephalosporins?
Cephalosporins antibiotic can, therefore, be used when penicillin is ineffective. β-lactams have R groups modify the antibiotic to give a different spectrum of activity. Cephalosporins have two R groups compared to one group in penicillin, creating more opportunities for chemical modification.
When was penicillin discovered?
Alexander Fleming discovered penicillin in 1928 when he accidentally left bacterial cultures uncovered near an open window. This lead to the contamination of the cultures with mold spores, which produced a compound that killed the bacteria. This compound was later named penicillin by Fleming.
How does mitomycin block replication?
Mitomycin C blocks replication by binding guanine bases that are located in both template strands of DNA [ 5 ].
How do pathogenic microorganisms infect human cells?
Pathogenic microorganisms can infect tissues of human by destroying cellular functions. Microorganisms themselves or their toxins can damage host cells. Microbial infections are treated with antimicrobials by either inhibiting the microbial growth or killing the microorganism. Antibiotics are widely being used not only in the treatment of acute and chronic infections, but also in the prophylactic treatment [ 1 ]. Targets of antimicrobials are cell membrane, cell wall, protein synthesis, nucleic acid synthesis, and biological metabolic compound synthesis ( Figure 1) [ 2 ]. Over usage of antibiotics, mutations in the genes, carrying resistance genes in chromosomes and plasmids, gaining resistance genes carried by transposons, insertion sequences (IS) and conjugation from the same or other species of microorganisms cause bacteria develop resistance to antimicrobials [ 3 ].
What is the -lactamase?
β-lactamase, that is an enzyme synthesized by many species of Gram-positive and Gram-negative bacteria, inactivates β-lactams degrading amide bond of β-lactam ring of β-lactam antibiotics [ 4] (bnm MRSA and MSSA). β-lactamases can be mediated by either plasmids or chromosomes, whereas penicillinases of Staphylococcus aureus are plasmid mediated, many Gram-negative bacteria are chromosomally mediated. β-lactamases that are plasmid mediated have tendency to be transferred between distinct species of bacteria. Chromosomally mediated β-lactamases can be either produced constructively as in the species of Bacteroides and Acinetobacter or induced as in the species of Enterobacter, Citrobacter, and Pseudomonas. Extended-spectrum β-lactamases (ESBLs) that are one class of β-lactamases having distinct ability to hydrolyze β-lactam rings of cefotaxime, ceftazidime, and aztreonam can be seen in a few species of Gram-negative bacteria such as Klebsiella pneumoniae and Escherichia coli [ 4 ].
How is protein translated from mRNA?
Protein is translated from mRNA by tRNA in ribosome. Translation is initiated by the binding of formylmethionine tRNA-aminoacyl-tRNA (fMet-tRNA fMet ), translation initiation region (TIR) of mRNA and initiation factor 2 (IF-2) to P site of 30S subunit of ribosome and the formation of 70S complex as a result of the release of IF-2. Translation continues with the binding of a new aminoacyl tRNA to A site, transferring the polypeptide from tRNA bond to P site to tRNA bond to A site by peptidyl transferase, and translocating of polypeptidyl tRNA from A to P site by elongation factor-G (EF-G), until translation is terminated by termination protein P (Rho) [ 5 ].
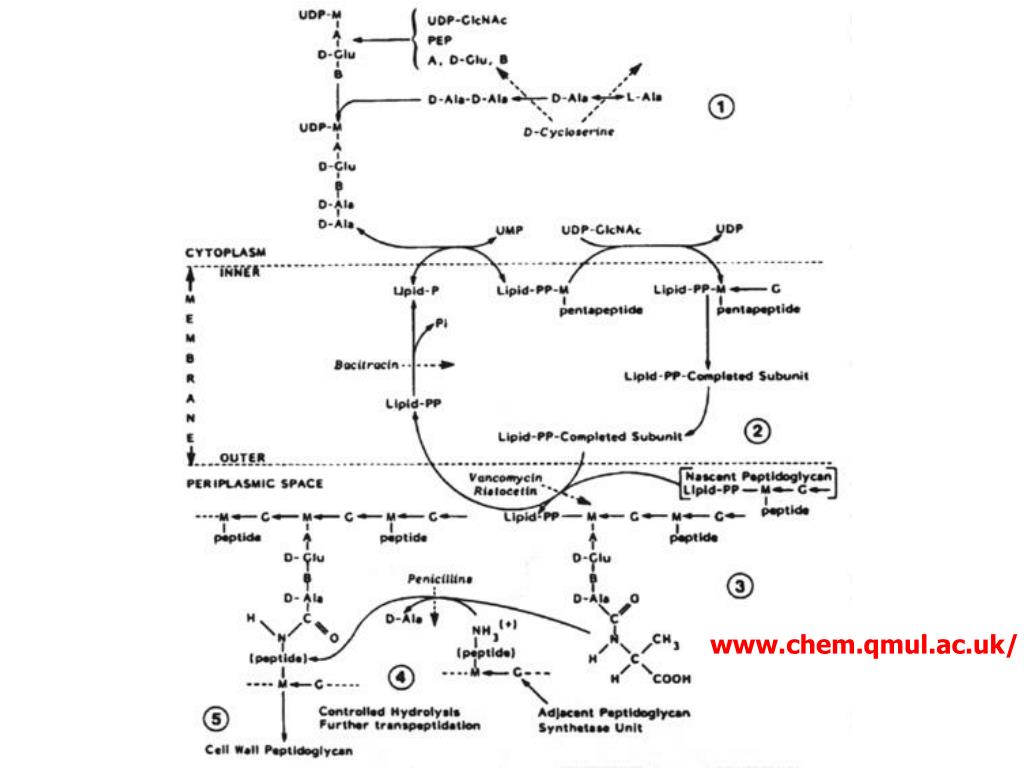
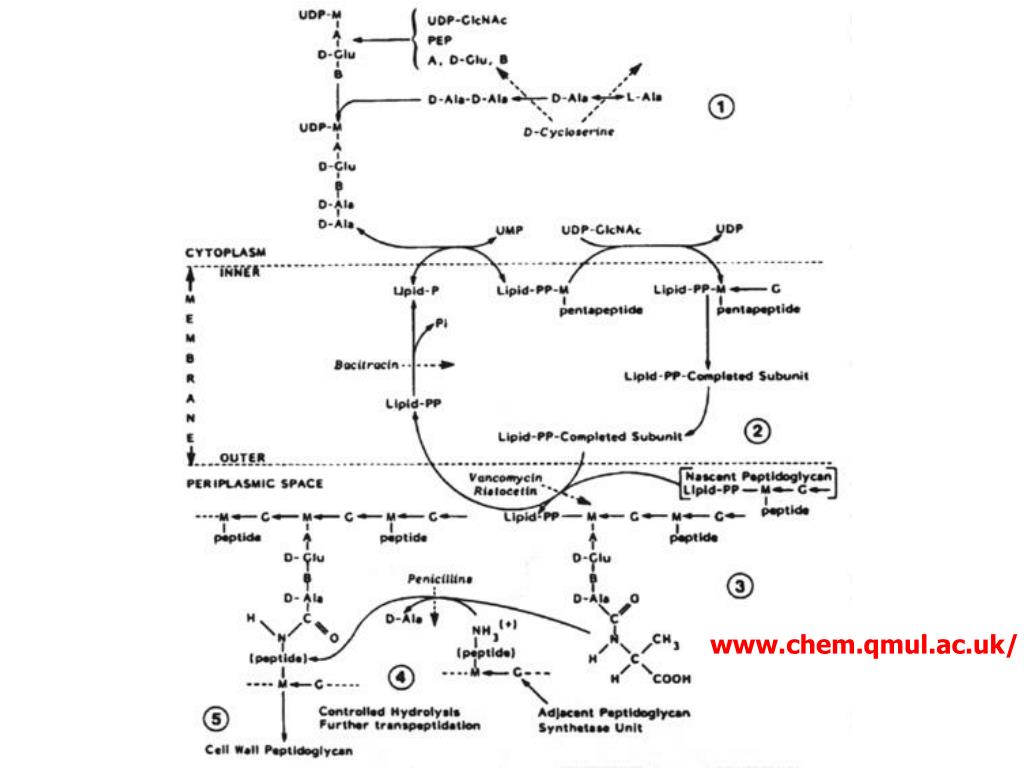
What is the cell wall of microorganisms?
Cell walls of microorganisms are constructed by peptidoglycan. Glycan polysaccharide strands are linked by crosslink that bind polypeptides bound to N-acetyl muromic acid (NAM) of each polysaccharide strands.
What is the role of the plasma membrane in cellular transport?
Plasma membrane of microorganism that has selective permeability contributes active transport to gain energy as ATP. Cytoplasmic content and gradient such as micro and macromolecules and ions are controlled by active transportation via integral transporter proteins. When selective membrane permeability is disrupted by antimicrobials, ions are lost and cellular ion gradient is distorted, so, the organism undergoes cellular damage and death [ 4 ].
What are some examples of drugs inhibiting the synthesis of metabolic biological compounds?
Sulfanilamide and 3,4,5-trimethoxybenzylpyrimidine are the examples of drugs inhibiting synthesis of metabolic biological compounds. Sulfonamides (Sulfa drugs) have been used in many infections such as urinary tract infections. Sulfonamide is widely used in combination with other compounds.
What is the mechanism of antibiotic resistance?
This section describes common antibiotic resistance mechanisms in bacteria. Antibiotics disrupt essential structures or processes in bacteria. This in turn either kills the bacteria or stops them from multiplying. Bacteria have in turn evolved many antibiotic resistance mechanisms to withstand the actions of antibiotics.
How do antibiotics stop interacting with the target?
Camouflage the target. Changes in the composition or structure of the target in the bacterium (resulting from mutations in the bacterial DNA) can stop the antibiotic from interacting with the target. Alternatively, the bacteria can add different chemical groups to the target structure, in this way shielding it from the antibiotic.
What happens if a bacteria does not have a cell wall?
Some bacteria are naturally resistant to certain antibiotics. Imagine for example an antibiotic that destroys the cell wall of the bacteria. If a bacterium does not have a cell wall, the antibiotic will have no effect. This phenomenon is called intrinsic resistance. When a bacterium that was previously susceptible to an antibiotic evolves resistance it is called acquired resistance.
What is the new penicillin binding protein?
The new penicillin-binding protein has low affinity to β-lactam antibiotics and is thus resistant to the drugs, and the bacteria survive treatment. This type of resistance is the basis in MRSA (methicillin-resistant Staphylococcus aureus ). Reprogram target.
How do bacteria withstand antibiotics?
There are two main ways for bacteria to withstand the effects of an antibiotic: To stop the antibiotic from reaching its target at a high enough concentration. To modify or bypass the target that the antibiotic acts on. Over time bacteria have evolved many different antibiotic resistance strategies to accomplish this.
What changes in the bacterial membrane make it more difficult to pass through?
Decrease permeability of the membrane that surrounds the bacterial cell. Certain changes in the bacterial membrane make it more difficult to pass through. In this way, less of the antibiotic gets into the bacteria.
What is ESBL in antibiotics?
In later years, bacteria that produce extended-spectrum β-lactamases, so called ESBL-producing bacteria, have become a major problem. They can degrade a wide spectrum of β-lactam antibiotics, sometimes also the last resort drugs available for infections with these bacteria. Modify the antibiotic.
What are the different types of antibiotics?
the β-lactam antibiotics (e.g. the penicillins and cephalosporins), vancomycin, the aminoglycosides (e.g. gentamycin), and the fluoroquinolones (e.g.ciprofloxacin).
What is broad spectrum antibiotic?
A broad spectrum antibiotic is one which is active against a wide range of bacteria - usually both gram positive and gram negative bacteria.
What antimicrobials should be used in patients with impaired hepatic function?
antimicrobial agents, including erythromycin, azithromycin, chloramphenicol, lincomycin, and clindamycin should be used with caution in patients with impaired hepatic function.
What is the MIC of a drug?
Most commonly the inhibitory concentrations have been used to quantitate the activity of an agent against an organism - referred to as the Minimal Inhibitory Concentration (MIC) even though a drug may be bacteriocidal in nature.
Which antibiotics are effective against Gram positive bacteria?
are the older penicillins (penG), the macrolides , and vancomycin (only effective against gram positive bacteria).
What drugs are included in the erythromycin list?
include the macrolids (e.g. erythromycin), clindamycin, sulfamethoxazole, trimethoprim, the tetracyclines, and chloramphenicol.
What does it mean to change the pharmacokinetic properties?
to change the pharmacokinetic properties - i.e. have a longer half-life thus increasing the time between doses or have better CSF penetration.