- Confusion or decreased alertness.
- Fatigue.
- Impaired growth in children.
- Increased breathing rate.
- Kidney stones.
- Nephrocalcinosis (too much calcium deposited in the kidneys)
- Osteomalacia (softening of the bones)
- Muscle weakness.
What are the signs and symptoms of intrarenal azotemia?
The symptoms of azotemia may include:
- acute renal failure (if azotemia continues to progress over a period of hours or days)
- acute kidney injury
- loss of energy
- not wanting to participate in your usual activities
- loss of appetite
- fluid retention
- nausea and vomiting
How can we use urinalysis to diagnose renal tubular acidosis?
To diagnose RTA, doctors check the acid-base balance in blood and urine samples. If the blood is more acidic than it should be and the urine is less acidic than it should be, the RTA may be the reason, but additional information is needed to rule out other causes.
What are the signs and symptoms of acute renal failure?
Signs of acute kidney failure can include: 3
- Abdominal pain
- Back pain
- Diarrhea
- Vomiting
- Nosebleeds
- Rash
- Fever
What are signs of renal toxicity?
Signs and symptoms of acute kidney failure may include:
- Decreased urine output, although occasionally urine output remains normal
- Fluid retention, causing swelling in your legs, ankles or feet
- Shortness of breath
- Fatigue
- Confusion
- Nausea
- Weakness
- Irregular heartbeat
- Chest pain or pressure
- Seizures or coma in severe cases

Does renal tubular acidosis go away?
Although the underlying cause of proximal renal tubular acidosis may go away by itself, the effects and complications can be permanent or life threatening. Treatment is usually successful.
Is renal tubular acidosis serious?
dRTA happens when the kidneys can't effectively remove the buildup of circulating acids in the blood. The buildup of acids in the blood causes an imbalance known as “acidosis” or “metabolic acidosis”. Metabolic acidosis is a serious health problem and requires prompt medical attention.
What medications cause renal tubular acidosis?
All could lead to acidosis.CA inhibitors (e.g. acetazolamide) 25.Anti-viral/HIV drugs (e.g. lamivudine, stavudine 75 and tenofovir 121– 124). ... Platinum-containing agents (e.g. cisplatin 126, 127) and DNA alkylating agents (e.g. ifosfamide 128– 130) are common proximal tubule toxins. ... Valproic acids (VPAs) 131– 133More items...•
What is the treatment for tubular acidosis?
For all types of RTA, drinking a solution of sodium bicarbonate link or sodium citrate will lower the acid level in your blood. This alkali therapy can prevent kidney stones from forming and make your kidneys work more normally so kidney failure does not get worse.
How do you test for renal tubular acidosis?
Normal kidneys reduce urine pH to < 5.2 within 6 hours of acidosis. Type 2 RTA is diagnosed by measurement of the urine pH and fractional bicarbonate excretion during a bicarbonate infusion (sodium bicarbonate 0.5 to 1.0 mEq/kg/hour [0.5 to 1.0 mmol/L] IV).
When do you suspect renal tubular acidosis?
RTA is often detected incidentally through an abnormal blood workup, but some patients present with clinical features such as poor growth, dehydration, or altered mental state. RTA can be triggered by many causes, from primary renal lesions to secondary disease processes.
Is renal tubular acidosis kidney disease?
Distal renal tubular acidosis is a disease that occurs when the kidneys do not properly remove acids from the blood into the urine. As a result, too much acid remains in the blood (called acidosis).
What removes CO2 from the kidneys?
Blood pH is kept within a narrow range of 7.36 to 7.44 by buffering systems in the body, primarily bicarbonate, or HCO3–, and excretion mechanisms to remove excess volatile acid in the form of carbon dioxide, or CO2, through the lungs and non-volatile acids through the kidneys.
Is renal tubular acidosis a chronic kidney disease?
If renal tubular acidosis persists, it may damage the kidney tubules and progress to chronic kidney disease. Major causes are diabetes and high blood pressure... read more . There are four types of renal tubular acidosis, types 1 through 4.
Is renal tubular acidosis kidney disease?
Distal renal tubular acidosis is a disease that occurs when the kidneys do not properly remove acids from the blood into the urine. As a result, too much acid remains in the blood (called acidosis).
When do you suspect renal tubular acidosis?
RTA is often detected incidentally through an abnormal blood workup, but some patients present with clinical features such as poor growth, dehydration, or altered mental state. RTA can be triggered by many causes, from primary renal lesions to secondary disease processes.
What do you mean by renal tubular acidosis?
In renal tubular acidosis, the kidney tubules malfunction, resulting in excess levels of acid in the blood. The tubules of the kidneys that remove acid from the blood are damaged when a person takes certain drugs or has another disorder that affects the kidneys.
What is renal tubular acidosis?
Renal tubular acidosis (RTA) occurs when the kidneys do not remove acids from the blood into the urine as they should. The acid level in the blood then becomes too high, a condition called acidosis. Some acid in the blood is normal, but too much acid can disturb many bodily functions.
What are the signs and symptoms of RTA?
The major signs of type 1 RTA and type 2 RTA are low levels of potassium and bicarbonate—a waste product produced by your body—in the blood. The potassium level drops if your kidneys send too much potassium into your urine instead of returning it to the blood.
What happens if you have a high potassium level?
In people with type 4 RTA, high levels of potassium in the blood can lead to muscle weakness 7 or heart problems , such as slow or irregular heartbeats#N#NIH external link#N#and cardiac arrest#N#NIH external link#N#. 8
Do diuretics decrease potassium?
certain diuretics used to treat congestive heart failure that do not decrease potassium in the blood
What is renal tubular acidosis?
Renal tubular acidosis refers to the electrolytic disturbances caused due to impaired excretion of renal Hydrogen ions or impaired bicarbonate resorption or abnormal production of aldosterone. This condition leads to a chronic metabolic acidosis with a gap in an anion. Usually, hyperchloremia or excess of chlorine in blood may be present. Other features may be with electrolytes of Potassium and Calcium. Chronic renal tubular acidosis is associated with damages of renal tubules in your kidneys. If ignored or not diagnosed at the right time, this condition may lead to chronic kidney diseases.
What supplements are used for renal tubular acidosis?
To treat type 1 renal tubular acidosis, Sodium bicarbonate or Sodium citrate is administered in stipulated dosages. To treat type 2 renal tubular acidosis, dietary changes are suggested such that bicarbonate replacement exceeds the acid load. Also, Sodium bicarbonate may be used as a substitute for citrate salts for increased tolerance. Additional Potassium supplements may also be prescribed.#N#To treat type 4 renal tubular acidosis, volume expansion of extracellular fluid is required. Also, frequent alkalization may be needed. Your urologist may also recommend mineralocorticoid replacement therapy, in which 0.1 to 0.2 mg of fludrocortisone is administered once a day to treat the condition. However, care needs to be exercised in this method, because the process could exacerbate the existing conditions of hypertension, edema or cardiac arrest.
Is renal tubular acidosis asymptomatic?
Generally, renal tubular acidosis is asymptomatic, meaning that it causes no symptoms or signs. It is rare for a severe electrolyte imbalance to happen, but in case it does, your situation could be life-threatening. Some symptoms of renal tubular acidosis are:
Why does renal tubular acidosis occur?
One of the causes of this type of renal tubular acidosis is deficiency of aldosterone due to malfunctioning of the adrenal glands, congenital adrenal hyperplasia, or aldosterone synthase deficiency. Another cause is hyporeninemic hypoaldosteronism, a condition that develops due to diseases, like HIV and renal dysfunctioning; or use of drugs, ...
What is the treatment for renal tubular acidosis?
Proximal renal tubular acidosis is mainly treated with oral bicarbonate. This compensates the loss of bicarbonates through urine, but the amount of bicarbonate supplements should be large enough to reverse the high acid content of the blood and bone demineralization.
What is the cause of RTA?
Type 4 RTA is caused by low levels of the hormone aldosterone (hypoaldosteronism), which directs the kidneys to regulate the levels of sodium, potassium, and chloride in the blood. The kidneys excrete excess amounts of sodium, potassium, and chloride, through urine. It may also be caused when the kidneys do not respond to this hormone. Hyperkalemic RTA is characterized by high levels of potassium in the blood or hyperkalemia. One of the causes of this type of renal tubular acidosis is deficiency of aldosterone due to malfunctioning of the adrenal glands, congenital adrenal hyperplasia, or aldosterone synthase deficiency.
What is the treatment for RTA?
The treatment for this form of RTA includes mineralocorticoid for aldosterone deficiency and fludrocortisone for hyporeninemic hypoaldosteronism.
How does the kidneys work?
These acids circulate in the blood, and it is the function of the kidneys to remove the excess acid from the blood and excrete it through urine. This filtration task is mainly done by the tubules of the nephron, which is the functional unit of the kidneys. There are around 800,000 to one million nephrons in a human kidney. In people affected with renal tubular acidosis (RTA), this function of the kidneys gets impaired, due to various reasons. This condition results in a rise in the acid content of the blood. The high levels of acid in blood is called metabolic acidosis, but RTA specifically refers to the condition in which the kidneys fail to remove the acids and expel them from the body, through urine.
What are the symptoms of a kidney stone?
The symptoms include severe rickets in children, loin pain, and hematuria (red blood cells in urine) caused by kidney stones. Sometimes, distal RTA may lead to renal failure and death.
Why is bicarbonate not as severe as RTA?
The bicarbonate levels of the urine also rises. This form is not as severe as the distal RTA, because in this case, the distal intercalated cells function normally.
What is renal tubular acidosis?
Renal Tubular Acidosis (RTA) is a type of medical condition that is characterized by accumulation of acids in the body caused by failure or inability of the kidneys to acidify the urine appropriately. When the kidney filters the blood, the filtrate is passed through the nephron’s tubules which allow the exchange of acid equivalents, salts as well as other solutes before it passes off into bladder as urine. This metabolic acidosis which results from renal tubular acidosis might be either caused by a failure to recover the alkaline bicarbonate ions from filtrate in early parts of the nephron or proximal tubule or by an insufficient secretion of the acid hydrogen ions in the latter parts of the nephron or distal tubule.
What causes hyperkalemic renal tubular acidosis?
Hyperkalemic renal tubular acidosis. Hyperkalemic RTA is mainly caused by aldosterone-related conditions, certain drug reactions as well as health conditions that alter the structure of the kidney. The common underlying factors for this condition include: HIV/AIDS. Amyloidosis.
What is the classical form of RTA?
Distal RTA or dRTA is said to be the classical form of the condition. It is characterized by failure to secrete acid by alpha intercalated cells that make up the cortical collecting duct of distal nephron.
What are the differential diagnoses of RTA?
The differential diagnoses of RTA include conditions like: Azotemia. Lactic Acidosis. Renal glycosuria.
How to treat type 4 RTA?
Patients having the Type 4 RTA can be treated by alkaline agents that might help in correcting the symptoms of acidosis. Medications to lower the levels of blood potassium can be prescribed by a doctor.
How to diagnose RTA?
The diagnosis of RTA is carried out by evaluating the blood chemistries and the arterial blood gas which may suggest electrolyte imbalances or metabolic acidosis, and show lower levels of potassium and/or bicarbonate. Other tests that are conducted to evaluate this condition include:
What is the cause of nephrocalcinosis?
Nephrocalcinosis, which can be both a sign as well as a cause, and is related to the calcium-induced damage of cortical collecting duct. Autoimmune diseases, such as the classic Sjögren’s syndrome, rheumatoid arthritis, systemic lupus erythematosus and hypergammaglobulinemia.
What is renal tubular acidosis?
The term renal tubular acidosis (RTA) describes any one of a number of disorders, in which the excretion of fixed acid (distal RTA) or the reabsorption of filtered bicarbonate (proximal RTA) is impaired to a degree that is disproportionate to any existing impairment of the glomerular filtration rate. [1]
What are the characteristics of a hyperkalemic RTA?
Defining characteristics of hyperkalemic (type IV) distal RTA are clinically significant hyperkalemia and the absence of the normal negative urine anion gap.
What is the cause of classic distal RTA?
Inherited (primary) classic distal RTA (type I) most often results from mutations of the genes for the renal apical membrane H-ATPase proton pump or the basolateral membrane anion exchanger AE1 gene.
What is the name of the condition where the kidneys lose substances that are normally reabsorbed by the kidney?
Fanconi syndrome is characterized by a generalized dysfunction of the renal proximal tubule that results in the urinary loss of substances normally reabsorbed by the kidney at this site. The substrates lost include bicarbonate, glucose, amino acids, phosphate, small proteins and peptides, and organic acids and bases.
Can you give fludrocortisone if you have hyperkalemic distal RTA?
If hyperkalemic distal RTA is due to mineralocorticoid deficiency, fludrocortisone can be given unless it is contraindicated due to the presence of fluid overload or uncontrolled hypertension.
Is a low pH in the urine a proximal RTA?
Urine pH is also low in hyperkalemic distal RTA. Proximal RTA (type II) occurs most often as a component of Fanconi syndrome, which is characterized by generalized dysfunction of the proximal tubule, with the resultant urinary loss of bicarbonate, calcium, phosphate, urate, amino acids, glucose, and other organic acids and bases.
What is the imbalance of acid in the blood?
The imbalance of too much acid in the blood is known as “acidosis” or “metabolic acidosis”. It can lead to many health problems and can vary in severity. In order to lessen (or buffer) the excess of serum protons (from circulating acids in the blood), the body can mobilize calcium and buffers such as bicarbonate and phosphate out of the bone. However, this process involves calcium leaching out of the bones. The loss of calcium from the bones can lead to thinning (osteoporosis) or bending (rickets) of the bones, kidney stones, and calcium deposits (nephrocalcinosis) in the kidneys. In addition, potassium levels in the blood can fall causing fatigue, muscle pain and cramps, and in the most severe cases, temporary paralysis and heart rhythm changes.
What are the signs and symptoms of dRTA?
Primary dRTA can cause a wide range of signs and symptoms. Symptoms can begin in infants or as late as adulthood. Not everyone will experience the same symptoms as they can vary depending on such factors related to the specific gene change, level of acidosis (acid in the blood), age of the individual, and even how advanced the disease is. Secondary dRTA usually happens later in life.
What happens in people living with dRTA?
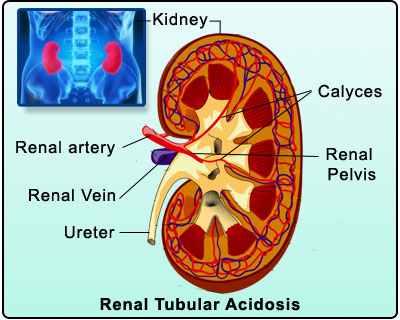
There are two kidneys, each about the size of a fist, located on either side of the spine at the lowest level of the rib cage. Each kidney contains up to a million functioning units called nephrons. A nephron consists of a filtering unit of tiny blood vessels called a glomerulus attached to a tubule.
How is dRTA diagnosed?
dRTA is diagnosed using a combination of tests, including a physical exam looking for signs and symptoms of the disease, along with blood and urine tests. If primary dRTA runs in your family, your healthcare team may take a detailed family history to help identify at-risk family members. Genetic testing may be offered to help confirm the diagnosis.
What is the role of the kidneys in maintaining a balance between acid and base?
One of them is to maintain a balance between acid and base (opposite of acid) by removing and filtering acids from the blood and through the urine. dRTA happens when the kidneys can’t effectively remove the buildup of circulating acids in the blood. The buildup of acids in the blood causes an imbalance known as “acidosis” or “metabolic acidosis”.
Is metabolic acidosis the same as renal tubular acidosis?
Metabolic acidosis is a serious health problem and requires prompt medical attention. dRTA can also cause kidney stones, brittle bones, hearing loss, digestive problems, and other medical problems. Not all people living with dRTA will experience the same health problems. dRTA is part of a class of disorders known as renal tubular acidoses (or renal tubular disease). There are four (4) types of renal tubular acidoses, with primary dRTA identified as the most common type.
Can drta cause kidney stones?
Mineral imbalances caused by dRTA can also lead to the formation of kidney stones. If kidney stones keep coming back after they are removed (recurrent) it can increase the risk of chronic kidney disease (CKD) and impact the filtering ability of your kidneys. Although considered uncommon, people with dRTA may be at higher risk of developing kidney failure, which would ultimately require dialysis or a kidney transplant.
