At least 16 systemic diseases have been linked to periodontitis. These systemic diseases are associated with periodontal disease because they generally contribute to either a decreased host resistance to infections or dysfunction in the connective tissue of the gums, increasing patient susceptibility to inflammation-induced destruction.
What are the side effects of periodontal disease?
The side effects of periodontal disease usually include:
- Changes in the fit of partial dentures
- Changes in the way your teeth fit together when you bite
- Gums pulling away from the teeth
- Loose teeth
- Painful chewing
- Persistent bad breath or a bad taste in the mouth
- Red/swollen gums
- Sensitive teeth
- Tender/bleeding gums
Is it possible to cure periodontal disease?
The good news is that it is possible to cure periodontal disease. Below are some of the aspects of periodontal disease treatment that can be expected. Behavior Change. This is one of the first things the dentist will recommend as part of your treatment. Because plaque is the root cause of periodontal disease, it is essential that it is removed every day.
Is periodontal disease linked to other diseases?
While a causal relationship has not been conclusively established, research suggest that periodontal disease may contribute to the progression of other diseases. People with diabetes are more likely to have periodontal disease than people without diabetes, probably because people with diabetes are more susceptible to contracting infections.
Is periodontal diseases easily treated?
f you’ve been diagnosed with periodontal (gum) disease, the good news is that it often can be treated successfully. The first nonsurgical step usually involves a special cleaning, called “scaling and root planing,” to remove plaque and tartar deposits on the tooth and root surfaces. This procedure helps gum tissue

What is one example of a systemic condition that can increase a patient's susceptibility to periodontal gum disease?
The number one systemic condition that increases susceptibility to periodontal disease is diabetes. Multiple risk factors do not increase the risk in an additive manner, but rather in an exponential manner.
What is a local and systemic risk factors for periodontal disease?
Initiation and progression of periodontal infections are affected by local and systemic conditions. The local factors include dental plaque and plaque retentive areas such as dental calculus and defective restorations. Systemic risk factors include poorly controlled diabetes mellitus and tobacco smoking.
What are systemic diseases that affect oral health?
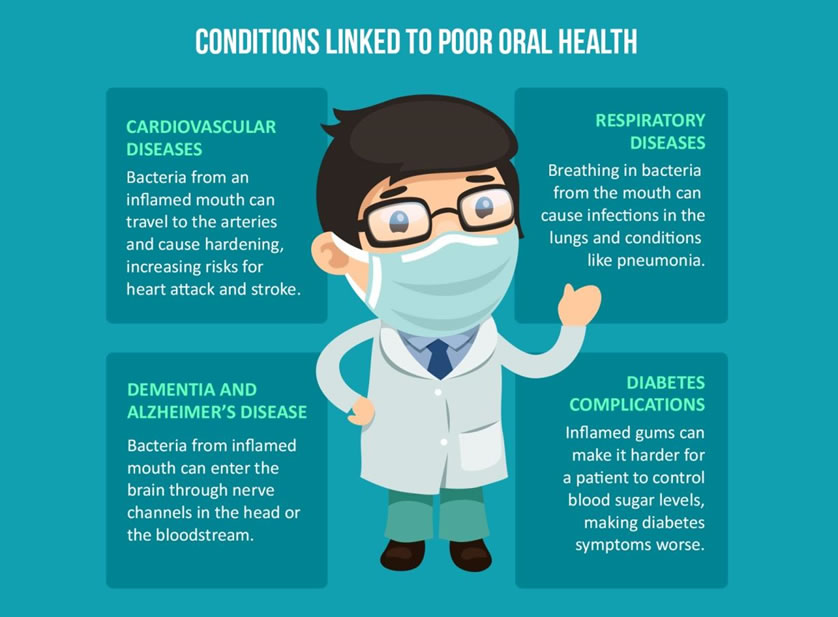
Significant associations between oral health status and a number of systemic diseases have been established, including, but not limited to, cardiovascular diseases, Alzheimer's disease and dementia, obesity, diabetes and metabolic disorders, rheumatoid arthritis, and several cancers.
Can periodontal disease cause other health problems?
The long-term inflammation caused by untreated periodontal disease can lead to a number of increased health risks, including high blood pressure, high cholesterol, and an increased risk of heart disease, heart attacks, and strokes.
What type of systemic conditions can have a negative influence of periodontal treatment?
A growing body of literature suggests that there is a link between periodontitis and systemic diseases. These diseases include cardiovascular disease, gastrointestinal and colorectal cancer, diabetes and insulin resistance, and Alzheimer's disease, as well as respiratory tract infection and adverse pregnancy outcomes.
What are some systemic conditions?
Systemic means affecting the entire body, rather than a single organ or body part. For example, systemic disorders, such as high blood pressure, or systemic diseases, such as the flu, affect the entire body. An infection that is in the bloodstream is called a systemic infection.
What is a systemic condition in dentistry?
Impact of oral diseases on general health and quality of life. Oral health means much more than beautiful teeth. It means freedom from chronic oral-facial pain, oral. and throat cancers, oral soft tissue lesions, birth defects such as cleft lip and palate, and other diseases.
Can gum disease cause systemic inflammation?
Based on well-designed epidemiological studies, it has been shown that people with periodontal diseases present a higher risk for systemic inflammation (12, 56). Periodontal disease is a chronic inflammatory condition that shares common mechanistic pathways with other systemic inflammatory diseases.
What are systemic risk factors?
Systemic risk is the risk that a company- or industry-level risk could trigger a huge collapse. Systematic risk is the risk inherent to the entire market, attributable to a mix of factors including economic, socio-political, and market-related events.
Which of the following is a local contributing factor to periodontal disease?
Inadequate oral hygiene and the lack of professional dental cleanings are the single most common reasons for periodontal disease.
What systemic factor contributes to periodontal breakdown?
Periodontal disease is increased by several risk factors: cigarette smoking; systemic diseases; medications such as steroids, anti-epilepsy drugs and cancer therapy drugs; ill-fitting bridges; crooked teeth and loose fillings; pregnancy; and oral contraceptive use.
What factors cause periodontal disease?
2. Risk Factors of Periodontal DiseaseMicroorganisms and Periodontal Disease. The oral bacterial microbiome includes over 700 different phylotypes, with approximately 400 species found in subgingival plaque [12, 13]. ... Tobacco Smoking. ... Diabetes Mellitus. ... Cardiovascular Disease. ... Drug-Induced Disorders. ... Stress. ... Obesity.
What is periodontal disease?
Periodontal diseases comprise a number of infectious and inflammatory conditions brought about by the interaction between supragingival and subgingival biofilms and the host inflammatory response.
Is smoking a risk factor for periodontal disease?
The current evidence supports some of these interactions, such as smoking as a risk factor for periodontal disease and diabetes mellitus, as both influenced by and influencing inflammatory changes in the periodontal tissue.
Is periodontal disease a systemic disease?
Periodontal diseases should be considered systemic conditions. This means that they are both modulated by the body's systems ...
How does periodontal disease affect the body?
About one in two adults in the United States has periodontal disease. Chronic periodontitis is an oral disease affecting the supporting structures of the teeth leading to progressive loss of the attachment apparatus and bone around teeth.
What is the term for a disease that affects the attachment apparatus and bone around teeth?
Chronic periodontitis is an oral disease affecting the supporting structures of the teeth leading to progressive loss of the attachment apparatus and bone around teeth. It is characterized by gingival pocket formation and/or gingival recession. The disease is initiated by bacteria and their components like lipopolysaccharide ...
What is gingival pocket?
It is characterized by gingival pocket formation and/or gingi …. About one in two adults in the United States has periodontal disease. Chronic periodontitis is an oral disease affecting the supporting structures of the teeth leading to progressive loss of the attachment apparatus and bone around teeth. It is characterized by gingival pocket ...
What causes osteoclastic activity?
The disease is initiated by bacteria and their components like lipopolysaccharide and causes a heightened host inflammatory response. This cascade of inflammatory response ultimately leads to an increased osteoclastic activity and bone loss.
Why is periodontal disease important?
The same studies suggest that managing periodontal disease is an effective preventive measure to manage or prevent erectile dysfunction. Obesity – Gum inflammation and periodontal disease may be linked to adults ...
What diseases are linked to gum disease?
Systemic Diseases Linked to Gum Disease. Cardiovascular Diseases – Bacterial plaque from the oral cavity can make its way into a person’s bloodstream through the open area of infection and blood flow just under the gumlines. The plaque then travels through the arterial system and can become lodged in arterial plaque or find its way into the heart.
Why do gums recede?
Antibodies sent through bloodstream to infected area of gums. Gum recession – Loss of tissue attachment in areas of oral infection can cause the gums to recede, making teeth appear longer and exposing sensitive root surfaces.
What does it mean when you have gingiva?
Gingiva in a person with a compromised immune system may exhibit a combination of the following symptoms: Bleeding gums – Elevated immune responses in the body send antibodies throughout the bloodstream to areas that are infected with bacterial infections.
Why is it important to understand the risk factors associated with your specific health condition?
Understanding the risk factors associated with your specific health condition allows you to be better aware of whether or not you are managing it effectively. The fact is that having a systemic health disease will in and of itself be a risk factor in developing gum infections like periodontal disease or other oral health problems.
What is the most serious complication associated with gum disease?
The most serious complication associated with gum disease is not the loss of teeth, it is the increased likelihood of suffering from more aggressive systemic health conditions. Ultimately, many health concerns have been shown to have a direct correlation with the oral health status of a person. The more severe their oral health, ...
What happens when you have advanced gum disease?
Also, when advanced gum disease is difficult to manage due to poor health, unmanageable bacterial levels will result in bone loss around the teeth. Tooth mobility and loss are imminent when bone loss is severe.
Why are periodontal diseases associated with periodontal disease?
These systemic diseases are associated with periodontal disease because they generally contribute to either a decreased host resistance to infections or dysfunction in the connective tissue of the gums , increasing patient susceptibility to inflammation-induced destruction.
What is the classification of periodontitis?
Periodontitis as a manifestation of systemic diseases is one of the seven categories of periodontitis as defined by the American Academy of Periodontology 1999 classification system and is one of the three classifications of periodontal diseases and conditions within the 2017 classification.
What is the role of coordination in periodontal treatment?
For those patients with periodontitis as a manifestation of hematologic disorders, coordination with the patient's physician is instrumental in planning periodontal treatment.
Does diabetes cause periodontitis?
Recent evidence suggests that, similar to diabetes mellitus, individuals with impaired fasting glucose have higher degree of periodontal inflammation. For those patients with periodontitis as a manifestation of hematologic disorders, coordination with the patient's physician is instrumental in planning ...
What is the major factor in periodontal disease?
Dental plaque is the major factor in periodontal disease.
What are the risk factors that alter the body's response to bacteria that are present in the mouth?
There are also other risk factors alter the body's response to bacteria that are present in the mouth.?) and or (?Smoking, Diabetes mellitus, Poor oral hygiene, Osteoporosis, HIV/AIDS, Stress, Medications, or Local factor?)
What is the leading cause of tooth loss in adults?
Periodontal disease is the leading cause of tooth loss in adults.
What is the extension of the inflammatory process from the gingiva into the connective tissue and alveolar bone that?
Periodontitis is the extension of the inflammatory process from the gingiva into the connective tissue and alveolar bone that supports the teeth. The progression of periodontitis involves the destruction of connective-tissue attachment at the most apical portion of a periodontal pocket.
What is periodontal disease?
Periodontal diseases are mainly the result of infections and inflammation of the gums and bone that surround and support the teeth. In its early stage, called gingivitis, the gums can become swollen and red, and they may bleed. In its more serious form, called periodontitis, the gums can pull away from the tooth, bone can be lost, and the teeth may loosen or even fall out. Periodontal disease is mostly seen in adults. Periodontal disease and tooth decay are the two biggest threats to dental health.
How many people have periodontal disease?
47.2% of adults aged 30 years and older have some form of periodontal disease . Periodontal disease increases with age, 70.1% of adults 65 years and older have periodontal disease. This condition is more common in men than women (56.4% vs 38.4%), those living below the federal poverty level (65.4%), those with less than a high school education ...
What happens when bacteria in your mouth is on your teeth?
Bacteria in the mouth infect tissue surrounding the tooth, causing inflammation around the tooth leading to periodontal disease. When bacteria stay on the teeth long enough, they form a film called plaque, which eventually hardens to tartar, also called calculus.
How to treat gingivitis?
Gingivitis can be controlled and treated with good oral hygiene and regular professional cleaning. More severe forms of periodontal disease can also be treated successfully but may require more extensive treatment. Such treatment might include deep cleaning of the tooth root surfaces below the gums, medications prescribed to take by mouth or placed directly under the gums, and sometimes corrective surgery.
How to get rid of gum disease?
Brush and floss every day to remove the bacteria that cause gum disease.
What is the most serious form of tooth decay?
In its more serious form, called periodontitis, the gums can pull away from the tooth, bone can be lost, and the teeth may loosen or even fall out. Periodontal disease is mostly seen in adults. Periodontal disease and tooth decay are the two biggest threats to dental health.
