What causes ankylosing spondylitis (AS)?
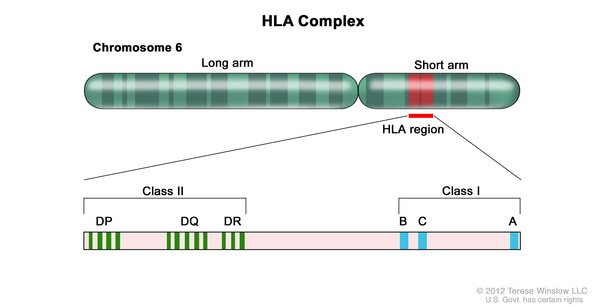
Ankylosing spondylitis has no known specific cause, though genetic factors seem to be involved. In particular, people who have a gene called HLA-B27 are at a greatly increased risk of developing ankylosing spondylitis. However, only some people with the gene develop the condition.
Can a bacterial infection cause spondylitis?
Some evidence indicates that bacterial infections, especially those affecting the gastrointestinal system, may trigger an inflammatory reaction that develops into spondylitis. A similar theory suggests that spondylitis develops when there is an imbalance in the bacteria colonizing the intestines.
Is spondylitis genetic?
For this reason, most researchers agree that genetic and environmental factors both contribute to the cause of spondylitis. More than 60 genes have been identified as playing a role in spondylitis risk. One gene, HLA-B27, is present in many people who are diagnosed with spondylitis.
Can the microbiome help treat ankylosing spondylitis?
The microbiome is a vast frontier about which very little is known. Alteration of the microbiome potentially could be used to treat or prevent many diseases caused by the immune system including ankylosing spondylitis.

What is the root cause of ankylosing spondylitis?
Ankylosing spondylitis has no known specific cause, though genetic factors seem to be involved. In particular, people who have a gene called HLA-B27 are at a greatly increased risk of developing ankylosing spondylitis. However, only some people with the gene develop the condition.
Do probiotics help ankylosing spondylitis?
Probiotic- being the natural product has been found to be effective against many SpA entities, including Ankylosing Spondylitis. It alters gut microflora somehow in such a way that it helps in reducing the predisposition of any factor to SpA.
Does leaky gut cause ankylosing spondylitis?
If the populations of certain microbial species grow too big, and other populations shrink or disappear, the gut's microbiome can become imbalanced. This condition is called dysbiosis. Dysbiosis is associated with rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis, and other autoimmune diseases.
Which pathogen is HLA-B27 related?
HLA-B27-associated ReA is a type of SpA triggered by bacteria such as Campylobacter, Chlamydia, Salmonella, Shigella, and Yersinia, resulting in oligoarthritis of the lower limbs and sometimes with urethritis and conjunctivitis (45).
Can antibiotics help ankylosing spondylitis?
We performed an open-label trial of moxifloxacin, a fluoroquinolone antibiotic, in patients with ankylosing spondylitis. Treatment with moxifloxacin resulted in significant and sustained improvement.
Does ankylosing spondylitis affect the digestive system?
Inflammation of the gastrointestinal tract is common in Ankylosing Spondylitis (AS). Up to 60% of AS patients who have no gastrointestinal symptoms will have microscopic (on biopsy) inflammation in the gut when colonoscopy is performed.
How can I reverse my ankylosing spondylitis naturally?
Natural treatments for ankylosing spondylitisStretching. Stretching helps build flexibility and may reduce pain. ... Heat therapy. To reduce stiffness and pain, apply a hot-water bottle or heating pad to the affected area. ... Cold therapy. ... Acupuncture. ... Massage therapy. ... Movement. ... Exercise. ... Alexander Technique.More items...
How do you reverse ankylosing spondylitis?
There's no cure for ankylosing spondylitis (AS), but treatment is available to help relieve the symptoms. Treatment can also help delay or prevent the process of the spine joining up (fusing) and stiffening.
Does ankylosing spondylitis affect teeth?
Ankylosing spondylitis (AS) is a type of arthritis that affects the lower spine. A person with AS may also experience dental issues, including tooth decay, periodontal diseases, ulcers, and infections.
What bacteria causes reactive arthritis?
Reactive arthritis isn't contagious. However, the bacteria that cause it can be transmitted sexually or in contaminated food. Only a few of the people who are exposed to these bacteria develop reactive arthritis....CausesCampylobacter.Chlamydia.Clostridioides difficile.Escherichia coli.Salmonella.Shigella.Yersinia.
Where does HLA-B27 come from?
HLA-B27 is associated with the pustular form of psoriasis and weakly associated with peripheral psoriatic arthritis. In the presence of spondylitis-associated with psoriasis, 60-70% of these cases are HLA-B27 positive.
Is HLA-B27 linked to MS?
Abstract. The prevalence of HLA-B27 in 420 patients with multiple sclerosis (MS) was 43 (10.2%).
How does B27 affect ankylosing spondylitis?
Nearly 40 years ago, a group in Los Angeles and a group in London discovered that the B27 type increased the odds of developing ankylosing spondylitis by about 100 fold. This is a phenomenal clue because most genetic factors increase the risk of developing a complex disease less than two fold. We now know a great deal about the HLA-B27 molecule.
What cofactors are involved in spinal arthritis?
We know that rats that are genetically manipulated to express HLA-B27 along with an important cofactor called beta 2 microglobulin spontaneously develop spinal arthritis that mimics many aspects of ankylosing spondylitis.
What is the overlap between psoriatic arthritis and inflammatory bowel disease?
Psoriatic arthritis and inflammatory bowel disease each have features that overlap with ankylosing spondylitis and many experts believe that each is triggered by a reaction to bacteria.
What is the easiest bacteria to study?
Second, the easiest bacteria to study are those that are present in feces, but the bacteria in the appendix, or the cecum, or the ascending colon might be the critical ones to study.
Is ankylosing spondylitis a disease?
Ankylosing spondylitis clearly is a disease caused by the immune system. For a century we have known that certain bacteria can trigger a reactive arthritis, especially in HLA-B27 positive individuals. Now that we know that intestinal bacteria shape our immune system. Because all HLA molecules affect the immune response, it is highly likely that HLA-B27 helps to determine which bacteria are in our microbiome and that in turn affects the likelihood that we will develop ankylosing spondylitis.
Can a mouse have arthritis?
It is possible to raise a mouse or a rat in a sterile environment such that bacteria never have a chance to grow inside the intestine. Without these bacteria, the immune system never develops. If the HLA-B27 positive rat is raised in this type of “germ free” environment, it develops very little arthritis.
Does B27 cause arthritis?
The B27 positive rat develops reduced arthritis if it receives antibiotics. And this remission is sustained if it swallows a specific strain of lactobacillus but not if it swallows a different strain. Lactobacilli are ingested by millions daily in the form of yogurt.
What are the genes that cause ankylosing spondylitis?
Variations in several additional genes, including ERAP1, IL1A, and IL23R, have also been associated with ankylosing spondylitis.
What causes AS in the body?
What exactly causes AS to develop in the body is generally unknown, although experts believe it is a combination of genetic, environmental, and factors related to the immune system.
How does the microbiome affect the immune system?
The microbiome plays many important roles, including the function of the immune system. Changes in the microbiome can lead to dysfunction in the immune system and have been linked to several autoimmune diseases.4 Many research studies have found that people with AS have an increased incidence of Klebsiella pneumoniae, a bacteria commonly found in the gut. In the gut, Klebsiella does not cause infections, but if it gets into other parts of the body (like the respiratory system), it can cause infections. 4-6
What are environmental factors that affect the immune system?
Some environmental factors seem to turn on certain mechanisms in the immune system, causing a change in how the immune system functions. 2. Changes in the microbiome are also believed to play a role in how AS develops. The microbiome is the collection of different microorganisms, like bacteria, fungi, and viruses, ...
Is smoking a risk factor for spinal cord damage?
Smoking: Smoking is a major environmental risk factor. It also worsens the severity of the disease. Studies have shown that it can double the risk for spinal damage.
Is ankylosing spondylitis a risk factor?
In addition, there are several risk factors that have been identified.
How old do you have to be to have ankylosing spondylitis?
Symptoms typically appear between the ages of 17 and 45 but may develop in younger children or older adults. Some people have persistent pain, while others experience milder symptoms. Symptoms may flare up (worsen) and improve (go into remission) off and on. If you have ankylosing spondylitis, you may experience:
What type of surgery is needed for ankylosing spondylitis?
Surgery: A small number of people with ankylosing spondylitis may need surgery. Joint replacement surgery implants an artificial joint. Kyphoplasty corrects a curved spine.
What is the condition that affects the spine?
Ankylosing spondylitis may affect more than the spine. The disease may inflame joints in the pelvis, shoulders, hips and knees, and between the spine and ribs. People with AS are more prone to spinal fractures (broken vertebrae). Other complications include: Fused vertebrae (ankylosis).
What is the name of the arthritis that inflames the spine?
Ankylosing spondylitis (pronounced ankle-oh-sing spon-dill-eye-tiss) is a form of arthritis that causes chronic (long-term) spine inflammation. Ankylosing spondylitis (AS) inflames the sacroiliac joints located between the base of the spine and pelvis. This inflammation, called sacroiliitis, is one of the first signs of AS. Inflammation often spreads to joints between the vertebrae, the bones that make up the spinal column. This condition is known as spondylitis.
What is the name of the arthritis that causes lower back pain?
Ankylosing Spondylitis (AS) Ankylosing spondylitis is a type of arthritis that causes lower back pain. Symptoms, including hip pain and a stiff back that may come and go. Over time, vertebrae in the spinal column may fuse and become rigid (ankylosis).
What is the first sign of a spondylitis?
This inflammation, called sacroiliitis, is one of the first signs of AS. Inflammation often spreads to joints between the vertebrae, the bones that make up the spinal column. This condition is known as spondylitis. Some people with AS experience severe, persistent back and hip pain and stiffness. Others have milder symptoms that come and go.
What is the protein that increases the risk of a disease?
About 95% of people who have AS have a variation of the human leukocyte antigen-B gene (HLA-B). This changed, or mutated, gene produces a protein called HLA-B27 that increases disease risk. However, most people with a mutated HLA-B gene don’t get AS.
What is ankylosing spondylitis 2021?
AS and IBD. Traditional treatment. Alternative treatment. Summary. Ankylosing spondylitis (AS) is a rare type of inflammatory arthritis that primarily affects the spine, lower back, and sacroiliac joints.
What percentage of people have spondylitis?
For reference, the Spondylitis Association of America (SAA) note the percentage of people with AS in populations around the world varies, with the lowest — 0.02% — in people in sub-Saharan Africa, and a higher — 0.35% — in the Northern Arctic.
What is the condition that causes pain and swelling in the spine?
Ankylosing spondylitis (AS) is a rare type of inflammatory arthritis that primarily affects the spine, lower back, and sacroiliac joints. The condition can cause new bone growth, pain, and swelling.
What causes Crohn's disease and ulcerative colitis?
The gut bacteria and resulting immune system reactions that trigger AS may also play a part in causing Crohn’s disease and ulcerative colitis, which are inflammatory bowel diseases (IBDs).
What causes AS?
While researchers do not exactly know what causes AS, they have identified that certain genes increase the risk of developing the condition.
Do bacteria affect the immune system?
According to some experts, the bacteria that humans share their bodies with have major effects on the immune system.
What are the causes of spondylitis?
For this reason, most researchers agree that genetic and environmental factors both contribute to the cause of spondylitis. More than 60 genes have been identified as playing a role in spondylitis risk. One gene, HLA-B27, is present in many people who are diagnosed with spondylitis.
What is spondylitis axspa?
Article written by. Kelly Crumrin. Spondylitis (also called spondyloarthritis or axSpA) is an autoimmune disease in which the immune system mistakenly attacks the joints and other tissues in the same way it would normally fight viruses or bacteria.
How much risk of spondylitis is there for a parent?
If you have a parent or sibling with spondylitis, your risk for developing spondylitis is three times higher than for someone with no relatives who have spondylitis. The risk for the general population to develop spondylitis is only 1 percent, so the risk of someone with a close family member with spondylitis is still only 3 percent.
When does spondylitis start?
People under age 45 are more likely to develop spondylitis than those older. Onset is most often in the 20s or 30s.
Does genetics cause spondylitis?
Most researchers do not believe that genetics alone determine who gets spondylitis. However, research has not yet identified which environmental factors play a role in causing the disease. Some evidence indicates that bacterial infections, especially those affecting the gastrointestinal system, may trigger an inflammatory reaction that develops into spondylitis. A similar theory suggests that spondylitis develops when there is an imbalance in the bacteria colonizing the intestines. Smoking is also theorized to increase the risk for developing spondylitis.
Does spondylitis have a correlation?
It is important to note that while science is good at finding correlations, or apparent relationships, between factors and disease, correlation does not prove that the risk factor causes the disease.
Can you get spondylitis if you test positive for HLA-B27?
Testing positive for HLA-B27 does not mean that you will definitely develop spondylitis. Only about 2 percent of those with the gene are diagnosed with axSpA. Read more about spondylitis diagnosis. Men are twice as likely as women to develop axSpa. Women with spondylitis tend to have a milder disease course than men.
What is ankylosing spondylitis?
Ankylosing spondylitis (AS) is a chronic inflammatory disease characterized by inflammation of axial joints and the pelvis. It is known that intestinal dysbiosis may exert direct pathogenic effects on gut homeostasis and may act as a triggering factor for the host innate immune system to activate and cause inflammation in extraintestinal sites in the so-called “gut-joint axis”, contributing to AS pathogenesis. However, although the intestinal microbiota’s influence on the clinical manifestation of AS is widely accepted, the mechanisms mediating the cross-talk between the intestinal lumen and the immune system are still not completely defined. Recent evidence suggests that the metabolism of microbial species may be a source of metabolites and small molecules participating in the complex network existing between bacteria and host cells. These findings may give inputs for further research of novel pharmacological targets and pave the way to applying dietary interventions to prevent the onset and ameliorate the clinical presentation of the disease. In this review, we discuss the role of some of the biological mediators of microbial origin, with a particular focus on short-chain fatty acids, tryptophan and vitamin B derivatives, and their role in barrier integrity and type 3 immunity in the context of AS.
What is axial spondyloarthritis?
Axial spondyloarthritis (AxSpA) is a chronic inflammatory disease belonging to spondylarthritis (SpA), characterized by inflammation of the axial joint [7]. Multiple studies demonstrate subclinical gut inflammation in up to 60% of patients affected by AxSpA [8,9]. Intestinal inflammation seems invariably linked to the dysfunction of the epithelial gut barrier, leading to a condition named “leaky gut” [8,10,11]. The inefficient separation of the intestinal lumen with the subepithelial space is associated with the aberrant activation of mucosal resident immune cells that, recirculating, may transfer the inflammation to the joint, establishing a pathogenic gut-joint axis [12,13,14,15]. The mucosal barrier alteration is part of a vicious circle involving the genetic predisposition, particularly HLA-B27, environmental factors, and altered intestinal dysbiosis [9,16]. Although the initial trigger of the dysbiosis is still not fully explained, multiple animal and human studies demonstrated an active role for the microbiota in the initiation and perpetuation of the inflammatory pathways behind the intestinal inflammation observed in AxSpA and in SpA more in general [8,17,18]. The study of the bacterial metabolic pathways and their bioproducts could offer another key to interpreting the maladaptive cross-talk existing between intestinal epithelial cells and mucosa immune cells and their immunometabolism which could be deeply helpful in deciphering the etiopathogenesis of these conditions.
Does a microbial composition affect the immune system?
Alterations of microbial composition have been demonstrated in patients with SpA, and those alterations may contribute to the shaping of intestinal immune response which in some cases is mirrored by the increased recirculation of immune cells expressing markers of intestinal homing [27,28]. More recently, Klingberg et al. analyzed the cecal microbiota composition in 150 patients with AxSpA, 18 patients with ulcerative colitis (UC), and 17 healthy controls (HC) with GA-map™ Dysbiosis Test, which also indicates the degree of deviation of the microbiota composition compared with healthy control populations. Dysbiosis was found in 87% of AxSpA patients [29].
Where are defensins produced?
Defensins are mainly produced by Paneth cells (PCs) at the bottom of the intestinal crypts and play an important role in the host defense against microbes. In AS patients with subclinical gut inflammation, PCs function is altered, leading to an overexpression of PC-related peptides, especially human α-defensin 5 (HD-5) [57].
Does SCFA affect neutrophils?
In mice, neutrophils treated with SCFAs are more sensitive to apoptosis , have decreased killing activity [69] and decreased chemotaxis [70]; these effects are seemingly mediated by SCFA-GPR43 interaction. Surprisingly, however, GPR43 deficient mice appear to suffer from more severe acute colitis but are protected from chronic colitis [71]. Chang et al. demonstrated that butyrate has an immunomodulatory effect on macrophages. Murine bone marrow-derived and intestinal lamina propria macrophages were stimulated with LPS and either butyrate, acetate, or propionate. They found that levels of nitric oxide, IL-6, and IL-12p40 were strongly decreased in the presence of butyrate in a dose-dependent manner, and this effect was attained through HDAC inhibition [72].
What is ankylosing spondylitis?
Ankylosing spondylitis (AS) is probably produced by repeated episodes of Klebsiella-reactive arthritis, usually in HLA-B27-positive individuals. This concept is based on immunological, microbiological and serological considerations. Immunological studies based on anti-B27 tissue typing sera and anti-B27 monoclonal antibodies indicate that HLA-B27 cross-reacts with antigens found in Klebsiella, Salmonella, Shigella and Yersinia micro-organisms. Salmonella, Shigella and Yersinia gut infections are associated with a reactive arthritis that occurs predominantly in HLA-B27-positive individuals. However, microbiological studies indicate that only Klebsiella, but not Salmonella, Shigella or Yersinia, can be isolated in faecal cultures obtained from AS patients. Furthermore, serological studies involving a number of different techniques demonstrate that only antibodies against Klebsiella, but not against Salmonella, Shigella or Yersinia, can be identified in active AS patients. The evidence is sufficiently extensive to warrant long-term studies involving Klebsiella reduction in the bowel flora of AS patients, in an attempt to reduce the severity and modify the development of the disease. It would appear that Klebsiella-reactive arthritis is the precursor stage occurring in the early and active phases of AS. Only future studies can determine whether this disease will remain a taxonomic curiosity or provide guidelines for therapeutic sequelae which will be of benefit to AS patients.
Does B27 cross-react with Yersinia?
Immunological studies based on anti-B27 tissue typing sera and anti-B27 monoclonal antibodies indicate that HLA-B27 cross-reacts with antigens found in Klebsiella, Salmonella, Shigella and Yersinia micro-organisms. Salmonella, Shigella and Yersinia gut infections are associated with a reactive arthritis that occurs predominantly in HLA-B27-positive ...
