What causes resistance in the arteries?
The fundamental cause of increased peripheral resistance is a decrease in lumen diameter. According to Poiseuille's law, resistance varies inversely with the fourth power of the blood vessel radius, so that a small decrease in the lumen markedly increases resistance.
What affects resistance in an artery?
Numerous factors can alter resistance, but the three most important are vessel length, vessel radius, and blood viscosity. With increasing length, increasing viscosity, and decreasing radius, resistance is increased.
What causes increased resistance in blood vessels?
The three most important factors affecting resistance are blood viscosity, vessel length and vessel diameter and are each considered below. Blood viscosity is the thickness of fluids and it affects fluid flow.
What does resistance mean in arteries?
Introduction. Peripheral vascular resistance (systemic vascular resistance, SVR) is the resistance in the circulatory system that is used to create blood pressure, the flow of blood and is also a component of cardiac function. When blood vessels constrict (vasoconstriction) this leads to an increase in SVR.
What has the greatest influence on resistance in blood vessels?
There are three primary factors that determine the resistance to blood flow within a single vessel: vessel diameter (or radius), vessel length, and viscosity of the blood. Of these three factors, the most important quantitatively and physiologically is vessel diameter.
What increases resistance in coronary artery?
An epicardial artery stenosis arising from atherosclerosis increases total coronary resistance and thus reduces maximal CBF. In addition, abnormalities in coronary microcirculatory control can also contribute to causing myocardial ischemia in many patients with a coronary artery stenosis.
How are resistance vessels controlled?
These vessels are highly innervated by autonomic nerves (particularly sympathetic adrenergic), and respond to changes in nerve activity and circulating hormones by constricting or dilating. Therefore, these vessels are referred to as resistance vessels.
What arteries are high resistance?
Arteries that normally show a high-resistance pattern Doppler waveform include arteries that supply primarily skeletal muscle at rest including the iliac, femoral, popliteal, subclavian, and brachial arteries. The external carotid artery (ECA) waveform is relatively high resistance in appearance.
Is vascular resistance normal?
A normal value for pulmonary vascular resistance using conventional units is 0.25–1.6 mmHg·min/l. Pulmonary vascular resistance can also be represented in units of dynes/sec/cm5 (normal = 37-250 dynes/sec/cm5).
Does obesity cause low vascular resistance?
Although often coexisting in the same patient, obesity and essential hypertension exert disparate cardiovascular effects. An excess of adipose tissue augments cardiac output, stroke volume, and left ventricular filling pressure, expands intravascular volume, and lowers total peripheral resistance.
What measures the resistance to blood flow in the arteries?
Systolic blood pressure measures the amount of pressure that blood exerts on vessels while the heart is beating. The optimal systolic blood pressure is 120 mmHg. Diastolic blood pressure measures the pressure in the vessels between heartbeats. The optimal diastolic blood pressure is 80 mmHg.
What measures the resistance to blood flow in the arteries?
Systolic blood pressure measures the amount of pressure that blood exerts on vessels while the heart is beating. The optimal systolic blood pressure is 120 mmHg. Diastolic blood pressure measures the pressure in the vessels between heartbeats. The optimal diastolic blood pressure is 80 mmHg.
What causes decreased vascular resistance?
Passive changes in the diameter of the pulmonary vessels can be induced by increases in flow (right ventricular output) and/or by elevations of left atrial pressure. Therefore, pulmonary vascular resistance tends to fall as flow increases.
What is the treatment for resistant hypertension?
Advanced treatment for resistant hypertension, including a thorough reevaluation of your existing care plan, medication and lifestyle changes, and new minimally invasive treatments.
How to reduce hypertension?
This would include watching your diet and keeping sodium intake low, keeping a home blood pressure log, attending educational workshops, reducing or managing stress, limiting alcohol consumption, giving up smoking.
Does renal denervation restore blood pressure?
By contrast, renal denervation silences a few, targeted nerves to restore healthy blood pressure. It does so with heat energy delivered by a catheter, a thin tube threaded through an artery. This minimally invasive procedure is currently in clinical trials at medical centers nationwide. Our program is the only West Coast participant in this trial.
What Causes Clogged Arteries?
Clogged arteries are caused by a buildup of plaque in your arteries. Plaque is usually made up of a few substances, including minerals like calcium, or fats and cholesterol. High cholesterol levels can lead to this buildup of plaques.
How to keep arteries clear of blockages?
The key to keeping your arteries clear of blockages is to eat a low-fat diet and exercise regularly. Plant-based diets have even been shown to help reverse coronary artery disease in some people. 8
What are the complications of a clogged artery?
The most concerning complications of clogged arteries are heart attack and stroke. A heart attack can occur when there is blockage in the coronary arteries, which supply blood to the heart. When a blockage affects the brain, this is called an ischemic stroke . This type of stroke can be treated effectively with strong blood thinners.
How do you know if you have a clogged artery?
There are many symptoms of clogged arteries, including numbness and tingling, high blood pressure, cold limbs, and discoloration of the skin.
What is the function of arteries?
Arteries are vessels in the body that carry blood and nutrients to and from each organ and tissue in your body. This complex system works well, but certain conditions and lifestyle choices can cause fat and cholesterol to build up in these vessels, eventually clogging them. When blood can't get through your artery, it can't deliver critical oxygen and nutrients to your organs and body parts.
What is a stent placement?
Stent placement, where tiny pieces of mesh coil are inserted to open the artery and improve blood flow
What is the procedure where a balloon is inflated in the artery to open the blocked area?
Balloon angioplasty, where a small balloon is inflated in the artery to open the blocked area
What is the cause of peripheral arterial disease?
It is primarily caused by the buildup of plaque in the arteries.
How to diagnose arterial disease?
Arterial diseases are usually diagnosed with a combination of physical exam, a review of symptoms and medical history, imaging studies like ultrasound, and other specific tests like cardiac catheterization for arterial diseases affecting the heart.
How many people have peripheral artery disease?
Peripheral artery disease is underdiagnosed and believed to be the most common of all arterial diseases, with at least 15 million Americans having the condition. 21
How is peripheral arterial disease diagnosed?
Peripheral arterial disease is usually diagnosed based on your symptoms, a physical exam, and imaging studies like ultrasound or computed tomography (CT).
What are the risk factors for CAD?
Being overweight, physical inactivity, unhealthy eating, and smoking tobacco are risk factors for CAD. A family history of heart disease also increases your risk for CAD, especially a family history of having heart disease at an early age (50 or younger). 12
Can you check your arteries?
No. There are many arteries in the body, and no single test can check the health of all of them. If your doctor is concerned about arterial disease in a particular area of your body, they may order imaging tests to help pinpoint the problem.
Can arterial disease cause heart attack?
Arterial diseases can often develop with few symptoms, but when one becomes a problem, it can cause serious issues like heart attack or stroke. Talk to your doctor about ways to improve your overall health and what genetic or familial traits you may have that raise your risk of developing an arterial disease.
Why are arterioles considered resistance vessels?
Recall that we classified arterioles as resistance vessels, because given their small lumen, they dramatically slow the flow of blood from arteries. In fact, arterioles are the site of greatest resistance in the entire vascular network. This may seem surprising, given that capillaries have a smaller size. How can this phenomenon be explained?
Why are veins more compliant than arteries?
Veins are more compliant than arteries and can expand to hold more blood. When vascular disease causes stiffening of arteries, compliance is reduced and resistance to blood flow is increased. The result is more turbulence, higher pressure within the vessel, and reduced blood flow. This increases the work of the heart.
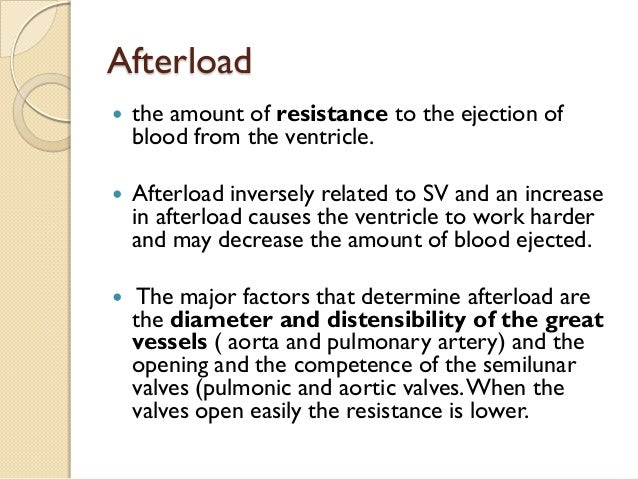
How does blood flow in the arteries affect the heart?
Recall that blood moves from higher pressure to lower pressure. It is pumped from the heart into the arteries at high pressure. If you increase pressure in the arteries (afterload), and cardiac function does not compensate, blood flow will actually decrease. In the venous system, the opposite relationship is true. Increased pressure in the veins does not decrease flow as it does in arteries, but actually increases flow. Since pressure in the veins is normally relatively low, for blood to flow back into the heart, the pressure in the atria during atrial diastole must be even lower. It normally approaches zero, except when the atria contract.
How does viscosity affect flow?
Viscosity is the thickness of fluids that affects their ability to flow. Clean water, for example, is less viscous than mud. The viscosity of blood is directly proportional to resistance and inversely proportional to flow; therefore, any condition that causes viscosity to increase will also increase resistance and decrease flow. For example, imagine sipping milk, then a milkshake, through the same size straw. You experience more resistance and therefore less flow from the milkshake. Conversely, any condition that causes viscosity to decrease (such as when the milkshake melts) will decrease resistance and increase flow.
What is the process of ejecting blood into the major arteries?
Ventricular contraction ejects blood into the major arteries, resulting in flow from regions of higher pressure to regions of lower pressure, as blood encounters smaller arteries and arterioles, then capillaries, then the venules and veins of the venous system.
What is hydrostatic pressure?
As noted earlier, hydrostatic pressure is the force exerted by a fluid due to gravitational pull, usually against the wall of the container in which it is located . One form of hydrostatic pressure is blood pressure, the force exerted by blood upon the walls of the blood vessels or the chambers of the heart.
Why is compliance important in arteriosclerosis?
This helps promote blood flow. In arteriosclerosis, compliance is reduced, and pressure and resistance within the vessel increase.
Why is vascular resistance important?
Vascular resistance is used to maintain organ perfusion. In certain disease states, such as congestive heart failure, there is a hyper-adrenergic response, causing an increase in peripheral vascular resistance. Prolonged increases in blood pressure affect several organs throughout the body. In conditions such as shock, there is a decrease in vascular resistance thus causing decreased organ perfusion which leads to organ malfunction. Peripheral vascular resistance is mediated locally by metabolites, and over a distance on a neuro-hormonal level, therefore, many different components may become altered leading to changes in peripheral vascular resistance.
What happens to the resistance of a vessel as the vessel dilates?
As the vessel dilates (radius increases), the resistance is divided by the change to the fourth power; this goes for a decrease in radius as well, such as during an adrenergic state (e.g., exercise) when blood pressure must increase. Related Testing.
How does shock affect blood pressure?
In conditions such as shock, there is a decrease in vascular resistance thus causing decreased organ perfusion which leads to organ malfunction.
What is peripheral vascular resistance?
Peripheral vascular resistance (systemic vascular resistance, SVR) is the resistance in the circulatory system that is used to create blood pressure, the flow of blood and is also a component of cardiac function. When blood vessels constrict (vasoconstriction) this leads to an increase in SVR.
Where does central dictation of peripheral vascular resistance occur?
Cellular. The central dictation of peripheral vascular resistance occurs at the level of the arterioles. The arterioles dilate and constrict in response to different neuronal and hormonal signals.
Which molecules cause vasoconstriction?
Other molecules that cause vasoconstriction on a cellular level include thromboxane, endothelin, angiotensin II, vasopressin, dopamine, AT P. [1][2][3]
Which equation expresses the mechanism of peripheral vascular resistance?
The basis for the mechanism of peripheral vascular resistance is expressed by the Hagen-Poiseuille equation:
How does volume affect vascular resistance?
Alveolar pressures and volumes greatly influence pulmonary vascular resistance. The effect of lung volume depends on the type of vessel. Extra-alveolar vessels run through the lung parenchyma. These vessels have smooth muscle and elastic tissue, which inherently reduces vessel circumference by counteracting distension. As the lung expands, the diameter of these vessels increases via radial traction of the vessel walls. Therefore, vascular resistance is low at large lung volumes. During lung collapse, there is increased resistance through the vessels due to the unopposed action of vessel elasticity. Critical opening pressure represents the air pressure needed to allow blood flow through extra-alveolar capillaries. This concept is applicable when modeling vascular resistance in a collapsed lung.
What is pulmonary vascular resistance?
Pulmonary vascular resistance is the resistance against blood flow from the pulmonary artery to the left atrium. It is most commonly modeled using a modification of Ohm’s law (figure 1). Pulmonary vascular resistance is the resistance against blood flow from the pulmonary artery to the left atrium. It is most commonly modeled using ...
How does pulmonary vascular resistance change with exercise?
As cardiac input increases, for example, during exercise, the pulmonic circulation must adapt to accommodate this increased forward flow. Therefore, pulmonary intravascular pressure and pulmonary vascular resistance are inversely related. Experiments have shown that increasing the pulmonary arterial pressure while holding left atrial pressure constant results in a decrease in pulmonary vascular resistance. This decrease occurs via two mechanisms: capillary recruitment and capillary distension.
Why is the pulmonary circulation low?
Generally, the pulmonary circulation has a low vascular tone; this is due to pulmonary vessels having proportionately less smooth muscle compared to vessels of similar diameter in other organs. Compared to systemic vessels, the smooth muscle tissue in pulmonary vessels is distributed less evenly in the tunica intima. The pulmonary veins are also more compliant than systemic arteries due to lack of tissue around small vessels, reduced elastin and collagen fibers, and reduced smooth muscle content. A phenomenon that is demonstrated by the pressure gradient observed between the right and left ventricles. [2][8]
What is the output pressure of pulmonary vascular resistance?
Total blood flow represents the cardiac output (5 to 6 L/min). A normal value for pulmonary vascular resistance using conventional units is 0.25–1.6 mmHg·min/l. Pulmonary vascular resistance can also be represented in units of dynes/sec/cm5 (normal = 37-250 dynes/sec/cm5). [1]
Where does the most of the vascular resistance in the pulmonary circuit reside?
Most of the total vascular resistance and distribution of blood flow in the pulmonary circuit resides in the capillaries rather than the vessels that are involved in active vasoconstriction. However, approximations generally divide pulmonary resistance equally between arteries, capillaries, and veins.
Which mechanism is responsible for maintaining low PVR?
Capillary distension is the second mechanism and involves the widening of the capillaries to accommodate increased blood flow. The Ovular vessels become more circular, which is the predominant mechanism for maintaining low PVR at higher pulmonary arterial pressures. [1]
Do insulin resistant blood vessels open up?
The animals' insulin-resistant arteries develop plaques that are twice the size of those on normal arteries. Insulin-resistant blood vessels don't open up as well, and levels of a protein known as VCAM-1 go up in them, too. VCAM-1 belongs to a family of adhesion molecules, Rask-Madsen explained.
Is atherosclerosis a problem for diabetics?
After all, atherosclerosis is responsible for many of diabetes' worst complications -- heart disease, stroke, and leg amputations among them.
Does insulin harden arteries?
And what insulin does in our arteries sends a signal that helps prevent the buildup of fatty plaques that can cause arteries to harden, new research in mice shows. Earlier studies showed that in the context of systemic insulin resistance, blood vessels become resistant, too.
Can insulin resistance affect your arteries?
Your arteries may be suffering insulin resistance, too. In people with insulin resistance or full-blown diabetes, an inability to keep blood sugar levels under control isn't the only problem by far. A new report shows that our arteries suffer the effects of insulin resistance, too, just for entirely different reasons.
What are the factors that affect vascular resistance?
There are many factors that alter the vascular resistance. Vascular compliance is determined by the muscle tone in the smooth muscle tissue of the tunica media and the elasticity of the elastic fibers there, but the muscle tone is subject to continual homeostatic changes by hormones and cell signaling molecules that induce vasodilation and vasoconstriction to keep blood pressure and blood flow within reference ranges .
What is the resistance offered by blood vessels that must be overcome to push blood through them and create flow?
Vascular resistance is the resistance offered by blood vessels that must be overcome to push blood through them and create flow.
What unit is used to measure vascular resistance?
Units for measuring vascular resistance are dyn ·s·cm −5, pascal seconds per cubic metre (Pa·s/m 3) or, for ease of deriving it by pressure (measured in mmHg) and cardiac output (measured in L/min), it can be given in mmHg·min/L. This is numerically equivalent to hybrid resistance units (HRU), also known as Wood units (in honor of Paul Wood, an early pioneer in the field), frequently used by pediatric cardiologists. The conversion between these units is:
What is the cause of vasodilation?
Adenosine causes vasodilation in the small and medium-sized resistance arterioles (less than 100 μm in diameter). When adenosine is administered it can cause a coronary steal phenomenon, where the vessels in healthy tissue dilate as much as the ischemic tissue and more blood is shunted away from the ischemic tissue that needs it most. This is the principle behind adenosine stress testing. Adenosine is quickly broken down by adenosine deaminase, which is present in red cells and the vessel wall.
What is the regulator of vascular resistance?
The major regulator of vascular resistance in the body is regulation of vessel radius. In humans, there is very little pressure change as blood flows from the aorta to the large arteries, but the small arteries and arterioles are the site of about 70% of the pressure drop, and are the main regulators of SVR. When environmental changes occur (e.g. exercise, immersion in water), neuronal and hormonal signals, including binding of norepinephrine and epinephrine to the α1 receptor on vascular smooth muscles, cause either vasoconstriction or vasodilation. Because resistance is inversely proportional to the fourth power of vessel radius, changes to arteriole diameter can result in large increases or decreases in vascular resistance.
How is blood flow resistance regulated?
The blood flow resistance in a vessel is mainly regulated by the vessel radius and viscosity when blood viscosity too varies with the vessel radius. According to very recent results showing the sheath flow surrounding the plug flow in a vessel, the sheath flow size is not neglectible in the real blood flow velocity profile in a vessel. The velocity profile is directly linked to flow resistance in a vessel. The viscosity variations, according to Thurston, are also balanced by the sheath flow size around the plug flow. The secondary regulators of vascular resistance, after vessel radius, is the sheath flow size and its viscosity.
What is the basic tenet of calculating resistance?
The basic tenet of calculating resistance is that flow is equal to driving pressure divided by flow rate.
What factors influence pulmonary vascular resistance?
Increased blood flow results in decreases pulmonary vascular resistance in order for pulmonary arterial pressure to remain stable. A biphasic process (rapid immediate vasoconstriction over minutes, then a gradual increase in resistance over hours)
How to determine resistance in pulmonary circulation?
Resistance in the pulmonary circulation is determined by: Proportions of laminar and turbulent flow. For turbulent flow, resistance cannot be determined by standard equations, only to say that it increases non-linearly as flow increases. Most flow in healthy pulmonary arteries is laminar.
Why is the pulmonary blood flow in the diagram lower than would be expected?
The pulmonary blood flow in the diagram is lower than would be expected (the scale only goes up to 800ml/min) because the data were collected from an isolated lung belonging to one 26-kg dog, held upright in a plethysmograph box, being perfused by the venous blood of another dog.
Why does pulmonary vasoconstriction increase at high volumes?
At low lung volumes, it increases due to the compression of larger vessels. At high lung volumes, it increases due to the compression of small vessels. Hypoxic pulmonary vasoconstriction. A biphasic process (rapid immediate vasoconstriction over minutes, then a gradual increase in resistance over hours)
Why are pulmonary vessels elastic?
Elastic distension of pulmonary vessels occurs in response to increased blood flow. They are sufficiently elastic that they can just blow up like balloons. Sobin et al (1972) got a bunch of cat lungs, perfused them with a silicon polymer at different pressures, and then catalytically hardened the silicon mixture to preserve the lung vasculature just as it was. Slices of the lung were then examined to see how the vessel diameter changed with different pressures. Nothing would say this better than the original microphotograph of the sliced cat lung:
How much does pulmonary arterial pressure fluctuate?
One's cardiac output may fluctuate from 3-4 L/min at rest to something like 25L/min with exercise . With these fluctuations in flow, pulmonary arterial pressure remains quite stable ( Kovacs et al, 2012 ). Because pressure is the product of flow and resistance, this means that pulmonary arterial resistance must vary depending on pulmonary blood flow. In a viva scenario or written SAQ answer, one could potentially skirt around having an in-depth understanding of this subject by reproducing this graph:
Which nerve fibres innervate the pulmonary arteries?
Pulmonary arteries have both α 1 and β 2 receptors. They are innervated by both the sympathetic nerve fibres arising from the thoracic spine and by the vagus nerve (M 3 receptors). The density of these receptors favours α 1 neurotransmission, and they seem to be distributed mainly around the larger pulmonary arteries.
Arterial Anatomy Function and Risk Factors
Types of Arterial Diseases
- There are several categories of arterial disease, including:3 1. Aneurysms:A bulge in the wall of the artery 2. Atherosclerosis: When fats and minerals—called plaque—build up on the inside of the vessels causing hardening, narrowing, and even blockages 3. Clots:A collection of blood cells or other materials than can create blockages in vessels 4. V...
Frequently Asked Questions
- Is there a test to screen for arterial diseases?
No. There are many arteries in the body, and no single test can check the health of all of them. If your doctor is concerned about arterial disease in a particular area of your body, they may order imaging tests to help pinpoint the problem. - Are arterial diseases reversible?
Not really. Although some studies have shown success in stopping or even reversing coronary artery disease with a plant-based diet,20prevention is often the best strategy for avoiding arterial diseases.
Summary
- Arterial diseases affect the arteries in your body, which send oxygen-rich blood from your heart and lungs to other parts of your body. When the arteries become blocked, the supply of oxygen and nutrients is cut off, resulting in various problems. Arterial diseases can occur in any part of your body. The best way to treat them is to prevent them by following a healthy lifestyle and kee…
A Word from Verywell
- Without your arteries, your heart and lungs could not feed the body’s tissues and organs with the oxygen and nutrients they need to function. Prevention is key: Exercising, quitting smoking, reducing your fat and cholesterol intake, and controlling chronic conditions like high blood pressure and diabetes can help you avoid arterial disease. Arterial diseases can often develop w…