Descent of the testes is a complex event mediated by hormonal and mechanical factors. At present we hypothesize that testicular descent occurs as the result of the secretion of descendin from a normal testicle. Descendin secretion results in selective growth of the gubernacular cells.
What is the descent of the testes?
Descent of the testes – Embryology October 2, 2019medical Between the 3rd month of pregnancy and its end the testes become transferred from the lumbar area (ventro-medial to the mesonephros) into the future scrotum. This transfer is due to a combination of growth processes and hormonal influences (7).
What causes an undescended testicle?
The exact cause of an undescended testicle isn't known. A combination of genetics, maternal health and other environmental factors might disrupt the hormones, physical changes and nerve activity that influence the development of the testicles.
What is an ascending testicle?
The testicle moves to its correct location in the scrotum and stays there permanently. Sometimes the retractile testicle remains in the groin and is no longer movable. When this happens, the condition is called an ascending testicle or an acquired undescended testicle. Testicles form in the abdomen during fetal development.
What is the processus vaginalis during testis descent?
During testis descent, a herniation of the abdominal cavity, the processus vaginalis, develops along the course of the gubernaculum, forming the inguinal ring and canal and descending with the testis into the scrotum. John C. Achermann, Ieuan A. Hughes, in Williams Textbook of Endocrinology (Thirteenth Edition), 2016
See more
What causes descent of testis?
The exact cause of an undescended testicle isn't known. A combination of genetics, maternal health and other environmental factors might disrupt the hormones, physical changes and nerve activity that influence the development of the testicles.
What stimulates the descent of the testes?
Each of the two phases of testis descent is regulated by a hormone secreted by Leydig cells: INSL3 regulates the transabdominal phase, whereas testosterone controls the inguinoscrotal phase [6]. Disrupted production of either hormone is responsible for a disorder called cryptorchidism, or undescended testis.
What causes the testes to ascend?
All males have a cremaster muscle (a thin pouch-like muscle in which a testicle rests). When the cremaster muscle contracts (tightens), it pulls the testicle upward toward the body; this is known as the cremasteric reflex. The cremasteric reflex is brought on by such things as cold, touch, and anxiety.
What does it mean when your balls descend?
As a baby boy grows inside his mother's womb, his testicles form inside his abdomen and move down (descend) into the scrotum shortly before birth. But in some cases, that move doesn't happen, and the baby is born with one or both testicles undescended. The majority of cases are in male babies born prematurely.
At what age does the testes descend?
In most cases no treatment is necessary, as the testicles will usually move down into the scrotum naturally during the first 3 to 6 months of life.
Can undescended testicle cause erectile dysfunction?
Infertility. Men with a history of cryptorchidism may have lower sperm counts, sperm of poorer quality and lower fertility than men with normally-descended testes. The degree to which men are affected, depends on whether one or both testes were undescended and how long they were undescended before being corrected.
Can you get an erection without testes?
Without both testicles, your body won't be able to make as much testosterone as it needs. That might lower your sex drive and make it harder to have erections. You could have hot flashes, lose some muscle mass, and be more tired than usual.
How do you fix a retractile testicle?
Retractile testicles don't require surgery or other treatment. A retractile testicle is likely to descend on its own before or during puberty.
Is retractile testicle painful?
There are typically no issues like pain or trouble urinating associated with a retractile testicle. At times it may appear that the scrotum looks empty and you cannot see the testicle(s).
Why do your balls drop with age?
As you get older, the muscles don't work as well, and your scrotum stays in a more slackened position. Combine that with your skin's natural decline in elasticity, and the sagging gets worse. If you're over 40, a hydrocele can also make your scrotum sag. It happens when fluid builds up around one or both testicles.
How do you tell if my balls have dropped?
How Do I Know There's a Problem? The main sign: You can't see or feel the testicle in the scrotum. When both are undescended, the scrotum looks flat and smaller than you'd expect it to be. Some boys have what's called a retractile testicle.
How long does it take for a man's balls to fill back up?
Your body produces fresh sperm every day, and your sperm supply gets replenished at least every 64 days.
What stimulates the descent of the testes quizlet?
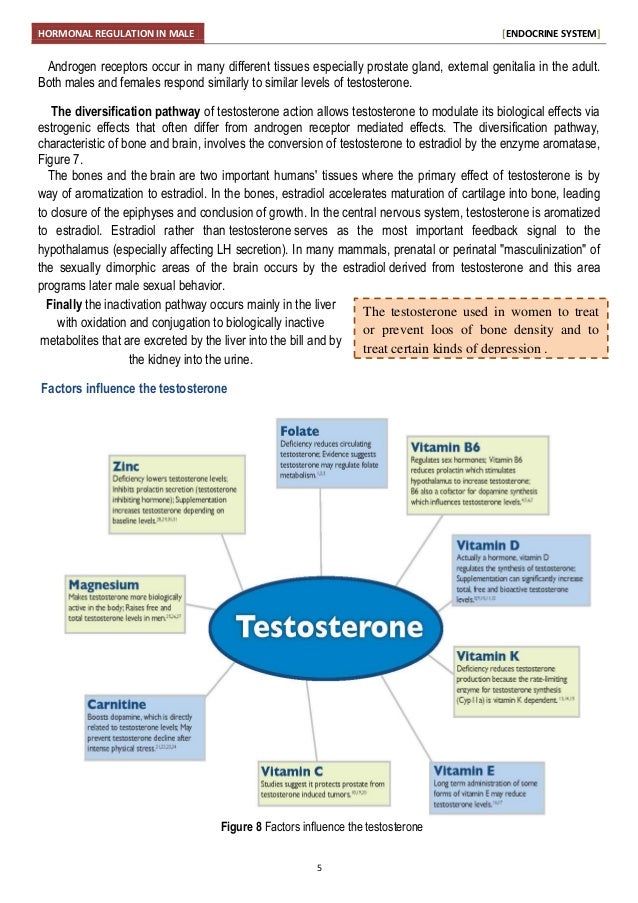
Testosterone stimulates the development of the male reproductive organs and causes the testes to descend. It is responsible for the development and maintenance of male secondary sex characteristics.
What is stimulated when testosterone is produced in the testes?
Luteinizing hormone (LH) stimulates testosterone production. If too much testosterone is produced, the hypothalamus alerts the pituitary gland to make less LH, which tells the testes to decrease testosterone levels.
How do pituitary hormones affect the function of testes?
FSH acts on the Sertoli cells of the testis. It stimulates the primary spermatocytes to undergo the first meiotic division.
What is a Cremasteric reflex?
The cremasteric reflex is a superficial reflex found in human males that is elicited when the inner part of the thigh is stroked. Stroking of the skin causes the cremaster muscle to contract and pull up the ipsilateral testicle toward the inguinal canal.
Why do testes descend outside the body cavity?
The descent of the testes outside the body cavity is necessary because effective spermatogenesis requires temperatures that are 2-3°C lower than body temperature.
Where do the testes come from?
The testes are innervated by autonomic nerves. Parasympathetic, visceral afferent fibers, and sympathetic fibers come from the testicular plexus (T10) found nearby the testicular artery. Therefore, the autonomic nervous plexus travels to the testes within the spermatic cord.
How many seminiferous tubules are there in the testis?
Each of the 200-300 lobules of the testis are filled with one to four highly convoluted seminiferous tubules which each course towards the mediastinum testis. Before entering the mediastinum, they change to a straight course, so in this segment, each convoluted tubule becomes a straight seminiferous tubule. Straight tubules enter the mediastinum, and by interconnecting they form a collecting chamber called rete testis .
Where is the head of the epididymis?
The head of the epididymis is where the efferent ductules merge. The true epididymis is a coiled tubular continuation of the head. It extends inferiorly as the body of the epididymis and at the inferior pole of the testis enlarges and forms the tail of the epididymis.
What are the two sides of the testis?
Anatomy. On the testis, we can observe two sides (medial and lateral) that are separated by two edges (anterior and posterior). We can also observe superior and inferior poles since it is an ovoid organ. On the posterior edge and superior pole of the testis is a structure called the epididymis.
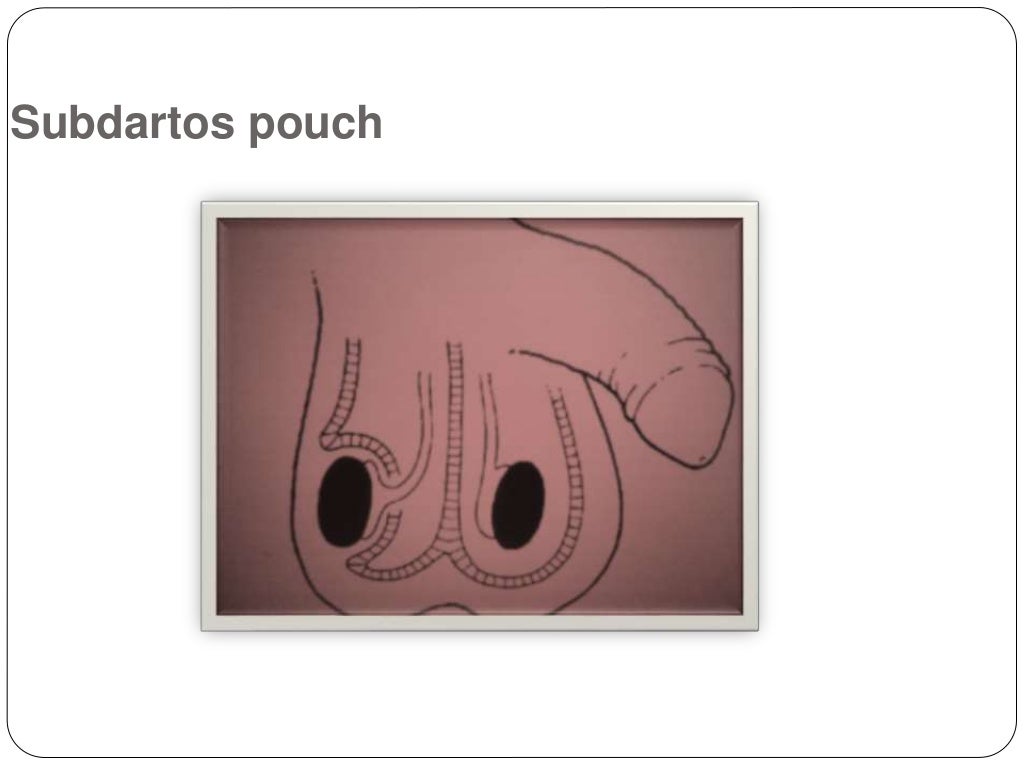
What is the scrotal sac?
Scrotum is a cutaneous (skin) sac that protects the testes. It consists of two layers: most superficially is the skin, and deeper is the dartos fascia. The dartos fascia contains muscle fibers that contract when it is cold, which results in wrinkling of the scrotal skin and brings the testes closer to the body.
What hormones are produced by the male ovaries?
Testes in males are analogous to the female ovaries. They produce sex hormones called androgens (primarily testosterone) in the process of steroidogenesis and are the place of spermatogenesis, the production of sperm.
Overview
A retractile testicle is a testicle that may move back and forth between the scrotum and the groin. When the retractile testicle is residing in the groin, it might be easily guided by hand into its proper position in the scrotum — the bag of skin hanging behind the penis — during a physical exam.
Symptoms
Testicles form in the abdomen during fetal development. During the final months of development, the testicles gradually descend into the scrotum. If this descent isn't completed at birth, the testicle usually descends within a few months.
Causes
An overactive muscle causes a testicle to become a retractile testicle. The cremaster muscle is a thin pouch-like muscle in which a testicle rests. When the cremaster muscle contracts, it pulls the testicle up toward the body. The cremaster reflex can be stimulated by rubbing a nerve on the inner thigh and by emotion, such as fear and laughter.
Complications
Retractile testicles are generally not associated with complications, aside from a greater risk of the testicle becoming an ascending testicle.
Where do testicles form?
Testicles form in the abdomen during fetal development. During the last couple of months of normal fetal development, the testicles gradually descend from the abdomen through a tube-like passageway in the groin (inguinal canal) into the scrotum. With an undescended testicle, that process stops or is delayed.
Why is my son's testicle not abnormal?
This is not abnormal and is due to a muscle reflex in the scrotum. An ascending testicle, or acquired undescended testicle, that has "returned" to the groin and can't be easily guided by hand into the scrotum. If you notice any changes in your son's genitals or are concerned about his development, talk to your son's doctor.
What are the factors that increase the risk of an undescended testicle in a newborn?
Factors that might increase the risk of an undescended testicle in a newborn include: Low birth weight. Premature birth. Family history of undescended testicles or other problems of genital development. Conditions of the fetus that can restrict growth, such as Down syndrome or an abdominal wall defect.