What is glycogen storage disease type 1?
Glycogen storage disease type I (also known as GSDI or von Gierke disease) is an inherited disorder caused by the buildup of a complex sugar called glycogen in the body's cells. The accumulation of glycogen in certain organs and tissues, especially the liver, kidneys, and small intestines, impairs their ability to function normally.
What are the causes of glycogen storage disease (GSDI)?
Causes Type I glycogen storage disease is associated with abnormalities in two genes. Mutations in the G6PC gene result in a deficiency in the glucose-6-phosphatase (G6Pase) enzyme and account for approximately 80% of GSDI.
What are the signs and symptoms of glycogen storage disease I?
Mar 29, 2022 · April 15, 2022. Type I glycogen storage disease (GSD I), also known as von Gierke’s disease, is the most common form of glycogen storage disease, accounting for 25% of all cases. It is an inherited disorder that affects the metabolism – the way the body breaks food down into energy. After we eat, excess glucose is stored in the liver as glycogen to maintain normal …
What is the treatment for Type I glycogen storage disease?
Glycogen storage disease type 1 is an autosomal recessive disorder caused by defects in the glucose 6-phosphatase (G6Pase) complex, which catalyzes the terminal steps of both hepatic gluconeogenesis and glycogenolysis, the hydrolysis of glucose 6-phosphate to glucose and inorganic phosphate. Deficiency of G6Pase activity in liver, kidney, and intestine results in the …
What causes glycogen storage disease?
Glycogen storage disease is passed down from parents to children (hereditary). It happens because both parents have an abnormal gene (gene mutation) that affects a specific way that glycogen is stored or used. Most GSDs occur because both parents pass on the same abnormal gene to their children.
What causes glycogen storage disease type XI?
Glycogen storage disease type XI (GSD-XI) is an autosomal recessive disorder of glycogen metabolism. GSD-XI is caused by mutations in the LDHA gene, which encodes lactate dehydrogenase. Molecular characterization of genetic mutation in human lactate dehydrogenase-A (M) deficiency.
What causes Pompe's disease?
Mutations in the GAA gene cause Pompe disease. The GAA gene provides instructions for producing an enzyme called acid alpha-glucosidase (also known as acid maltase). This enzyme is active in lysosomes , which are structures that serve as recycling centers within cells.May 20, 2021
How common is glycogen storage disease?
How common are they? A glycogen storage disorder occurs in about one in 20,000 to 25,000 babies. The most common types of GSD are types I, II, III, and IV, with type I being the most common. It is believed that nearly 90% of all patients with GSD have types I through IV.Aug 2, 2019
How is Shay disease?
Overview. Gaucher (go-SHAY) disease is the result of a buildup of certain fatty substances in certain organs, particularly your spleen and liver. This causes these organs to enlarge and can affect their function.Apr 17, 2020
What is the average life expectancy for a child with Pompe disease?
They have characteristic heart (cardiac) problems (dysfunction due to heart enlargement) in addition to generalized skeletal muscle weakness and a life expectancy of less than 2 years, if untreated (classic infantile Pompe disease).
What are the signs and symptoms of Pompe disease?
Symptoms begin in the first months of life, with feeding problems, poor weight gain, muscle weakness, floppiness, and head lag. Respiratory difficulties are often complicated by lung infections. The heart is grossly enlarged. Many infants with Pompe disease also have enlarged tongues.Aug 9, 2021
What is Wolman disease?
Wolman disease is a type of lysosomal acid lipase (LAL) deficiency; a rare genetic disorder characterized by complete absence of an enzyme known as lysosomal acid lipase (LIPA or LAL). This enzyme is required to breakdown (metabolize) certain fats (lipids) in the body.
What is glycogen storage disease?
Glycogen storage disease type 1 is an inherited disorder caused by the buildup of a complex sugar called glycogen in the body's cells. The accumulation of glycogen in certain organs and tissues, especially the liver, kidneys, and small intestines, impairs their ability to function normally. Researchers have described two types ...
What is related disease?
Related diseases are conditions that have similar signs and symptoms. A health care provider may consider these conditions in the table below when making a diagnosis. Please note that the table may not include all the possible conditions related to this disease.
What is the HPO database?
People with the same disease may not have all the symptoms listed. This information comes from a database called the Human Phenotype Ontology (HPO) . The HPO collects information on symptoms that have been described in medical resources.
What is a GTR?
The Genetic Testing Registry (GTR) provides information about the genetic tests for this condition. The intended audience for the GTR is health care providers and researchers. Patients and consumers with specific questions about a genetic test should contact a health care provider or a genetics professional.
What do doctors look for in a diagnosis?
Healthcare professionals typically look at a person’s medical history, symptoms, physical exam, and laboratory test results in order to make a diagnosis.
What is glycogen storage disease?
Glycogen storage diseases are a group of disorders in which stored glycogen cannot be metabolized into glucose to supply energy and to maintain steady blood glucose levels for the body. Type I glycogen storage disease is inherited as an autosomal recessive genetic disorder. Glycogen storage disease type I (GSDI) is characterized by accumulation ...
What is GSD type 1?
GSD type I is diagnosed by laboratory tests that indicate abnormal levels of glucose, lactate, uric acid, triglycerides and cholesterol. Molecular genetic testing for the G6PC and SLC37A4 genes is available to confirm a diagnosis. Molecular genetic testing can also be used for carrier testing and prenatal diagnosis.
What is GSDI gene?
GSDI is associated with abnormalities (mutations) in the G6PC gene (GSDIA) or SLC37A4 gene (GSDIB). These mutations result in enzyme deficiencies that block glycogen breakdown in affected organs causing excess amounts of glycogen and fat accumulation in the body tissues and low levels of circulating glucose in the blood.
What are the symptoms of GSDI in infants?
The primary symptom of GSDI in infancy is a low blood sugar level (hypoglycemia). Symptoms of GSDI usually begin at three to four months of age and include enlargement of the liver (hepatomegaly), kidney (nephromegaly), elevated levels of lactate, uric acid and lipids (both total lipids and triglycerides), and possible seizures caused due to repeated episodes of hypoglycemia. Continued low blood sugar can lead to delayed growth and development and muscle weakness. Affected children typically have doll-like faces with fat cheeks, relatively thin extremities, short stature, and protuberant abdomen.
What happens if you have low blood sugar?
Continued low blood sugar can lead to delayed growth and development and muscle weakness. Affected children typically have doll-like faces with fat cheeks, relatively thin extremities, short stature, and protuberant abdomen. High lipid levels can lead to the formation of fatty skin growths called xanthomas.
Is glycogen storage inherited?
Type I glycogen storage disease is inherited as an autosomal recessive genetic disorder. Recessive genetic disorders occur when an individual inherits a non-working gene from each parent. If an individual receives one working gene and one non-working gene for the disease, the person will be a carrier for the disease, ...
What is glycogen storage disease?
Glycogen storage disease type I ( GSD I) is an inherited disease that results in the liver being unable to properly break down stored glycogen. This impairment disrupts the liver 's ability to break down stored glycogen that is necessary to maintain adequate blood sugar levels. GSD I is divided into two main types, GSD Ia and GSD Ib, ...
What causes splenomegaly in GSD I?
In GSD Ia, splenomegaly may be caused by a relation between the liver and the spl een which causes either to grow or shrink to match the relative size of the other , to a lessened degree. In GSD Ib, it is a side effect of the use of filgrastim to treat neutropenia.
How does glycogen work in the liver?
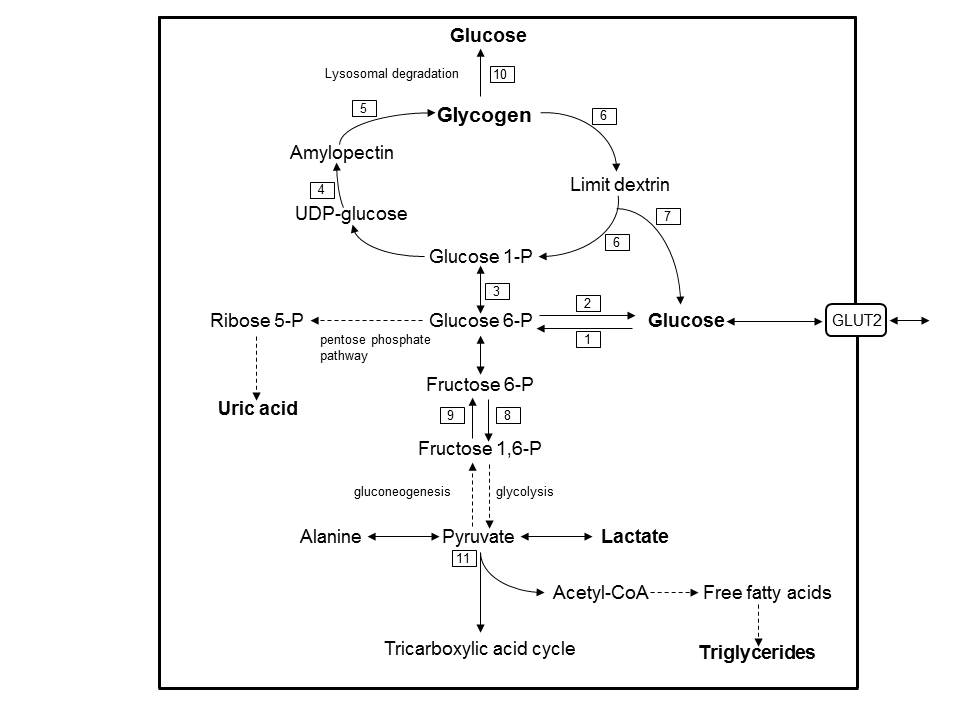
Glycogen in liver and (to a lesser degree) kidneys serves as a form of stored, rapidly accessible glucose, so that the blood glucose level can be maintained between meals. For about 3 hours after a carbohydrate-containing meal, high insulin levels direct liver cells to take glucose from the blood, to convert it to glucose-6-phosphate (G6P) with the enzyme glucokinase, and to add the G6P molecules to the ends of chains of glycogen (glycogen synthesis). Excess G6P is also shunted into production of triglycerides and exported for storage in adipose tissue as fat .
What is GSD 1?
GSD I patients typically present with an enlarged liver from non-alcoholic fatty liver disease as the result of this glycogen buildup. Other functions of the liver and kidneys are initially intact in GSD I, but are susceptible to a variety of other problems.
Can osteopenia be caused by GSD?
The specific etiology of low bone mineral density in GSD is not known, though it is strongly associated with poor metabolic control. Osteopenia may be directly caused by hypoglycemia , or the resulting endocrine and metabolic sequelae. Improvements in metabolic control have consistently been shown to prevent or reverse clinically relevant osteopenia in GSD I patients. In cases where osteopenia progresses with age, bone mineral density in the ribs is typically more severe than in the vertebrae. In some cases bone mineral density T-score will drop below -2.5, indicating osteoporosis. There is some evidence that osteopenia may be connected with associated kidney abnormalities in GSD I, particularly glomular hyperfiltration. The condition also seems responsive to calcium supplementation. In many cases bone mineral density can increase and return to the normal range given proper metabolic control and calcium supplementation alone, reversing osteopenia.
What is the treatment for GSD IB?
The principal treatment for this feature of GSD Ib is filgrastim; however, patients often still require treatment for frequent infections, and a chronically enlarged spleen is a common side effect. GSD Ib patients often present with inflammatory bowel disease. It is the most common of the glycogen storage diseases.
What causes lactic acidosis?
High levels of lactic acid in the blood, in extreme cases leading to lactic acidosis, caused by prolonged hypoglycemia. hepatic adenomas developing in adulthood and attendant risk of anemia, suspected to be caused by blood glucose dysregulation in the presence of non-alcoholic fatty liver disease.
What is glycogen storage disease?
Glycogen storage disease type I (GSD-I) is an autosomal recessive disorder caused by mutations in the glucose-6-phosphatase complex, leading to the accumulation of glycogen in the liver, kidneys, and intestine. Patients typically present within the first 6 months of life with hepatomegaly, hypoglycemia, and failure to thrive. Hepatic adenomas develop in 16% to 75% of patients with GSD-I, and their prevalence increases with age and with poor glycemic control. 48-50 Most patients with GSD-I develop adenomas by the second or third decade of life, and these adenomas are typically small, multiple, and nonencapsulated. The pathogenesis of adenoma formation has not been elucidated, although it is clear that these lesions have the potential to transform into carcinoma. In several reports, serial liver biopsies have documented the development of HCC within previously benign adenomas. 48,51-54 In a review by Coire et al, 48 the malignant transformation to HCC occurred in 11% of reported cases. Metabolic control has not been demonstrated to decrease the risk for malignancy in patients with GSD-I. In a recent study, Kishnani et al 55 suggested that genetic aberrations involving chromosome 6 may play a role in the malignant transformation of adenomas to HCC in GSD-I. Liver transplantation is appropriate when adenomas are progressively increasing in size despite dietary management and malignant change cannot be excluded or when patients have failed vigorous medical therapy. 48,56-58 In addition to eliminating the possibility of HCC development and progression, transplantation offers the advantage of correction of the metabolic abnormalities characteristic of GSD-I. Investigation continues regarding approaches to gene therapy for GSD-I, which may one day offer an alternative to liver transplantation. 59
What is GSD type 1?
GSD type 1 is caused by decreased activity of glucose-6-phosphatase, the enzyme that is perched at the terminus of both glycogenolysis and gluconeogenesis. Several different biochemical abnormalities can result in this phenotype, now classified as GSD types 1a, 1b, and 1c.
What is von Gierke disease?
Von Gierke disease is an autosomal recessive disorder caused by a deficiency of the enzyme glucose-6-phosphate translocase, which transports glucose-6-phosphate into the endoplasmic reticulum for further metabolism . In glycogen storage disease type 1b (GSD-1b), glucose-6-phosphate accumulates intracellularly. Affected neonates present with hypoglycemia, hepatomegaly, growth failure, and neutropenia. Patients with GSD-1b have recurrent bacterial infections, oral ulcers, and inflammatory bowel disease. The gene causing GSD-1b is located on chromosome 11q23. 25 rG-CSF can help patients avoid the recurrent bacterial infections that are otherwise a problematic part of this condition.
What is GSD I?
Glycogen storage disease type I (GSD I; Von Gierke disease) is an autosomal recessive inborn error of carbohydrate metabolism caused by defects of the glucose-6-phosphatase (G6Pase) complex. G6Pase catalyzes the hydrolysis of glucose-6-phosphate (G6P) to glucose and phosphate in the terminal steps of gluconeogenesis and glycogenolysis. The genes responsible for GSD I including G6Pase and G6P transporter genes have been identified and various mutations in the genes of GSD I patients have been reported ( Lei et al 1993, Lin et al 1998 ). G6Pase deficiency results in excessive accumulation of glycogen in the liver and kidney, leading to progressive hepatomegaly and renal enlargement. Clinical manifestations of GSD I including coma, seizures, irritability and increased respiratory rate caused by hypoglycemia, lactic acidosis and ketonemia, and hepatomegaly, present in early infancy. The recurrent hypoglycemia leads to the elevation of plasma glucagon levels, activating glycogen phosphorylase. The activation promotes the further elevation of G6P levels, resulting in a decrease of intrahepatic phosphate that inhibits AMP deaminase. This decrease stimulates AMP deaminase, resulting in the degradation of adenine nucleotides and consequent overproduction of uric acid ( Greene et al 1978, Cohen et al 1985 ). Lactic acidosis and ketonemia also decreases renal uric acid excretion by stimulation of uric acid reabsorption via URAT1. Conclusively, both overproduction and underexcretion of uric acid cause hyperuricemia in GSD I.
What is Type 1B?
Type 1b disease also causes impaired neutrophil function and recurrent infections. Infants presenting with hypoglycemia and progressive hepatomegaly are likely to have the disease. Routine laboratory studies, such as elevated blood lactate, triglycerides, and uric acid, support the diagnosis.
What is the G6Pase complex?
The enzyme G6Pase is associated with a complex of translocases, or transport proteins (108). The active site of the enzyme faces the lumen of the endoplasmic reticulum in hepatocytes. The enzyme complex appears to consist of the enzyme protein situated in close proximity to three translocases (T1, T2, and T3), which transport glucose-6-phosphate, phosphate and glucose, respectively, across the membrane of the endoplasmic reticulum. The clinical and biochemical features of GSD Ia result from deficiency of the catalytic subunit of the G6Pase enzyme. The absence or defective function of T1 (also called glucose-6-phosphate translocase or G6PT) results in GSD Ib, which is described later. Defects involving the other proteins of the complex are not well characterized, but may appear clinically similar to deficiency of the enzyme itself.
What are the two subtypes of GSD?
GSD type I has two biochemical subtypes – GSD Ia and Ib – each derived from deficiencies in particular components of the glucose-6-phosphatase (G6Pase) complex. The G6Pase complex comprises the catalytic subunit G6Pase (G6Pase and glucose-6-phosphatase alpha; responsible for GSD Ia ) and glucose-6-phosphate translocase (G6PT) (responsible for GSD Ib). The former is more common. The defects in both types Ia and Ib lead to inadequate hepatic conversion of glucose-6-phosphate to glucose through normal glycogenolysis and gluconeogenesis and make affected individuals susceptible to fasting hypoglycemia.
What is glycogen storage disease?
Glycogen storage disease type 1B (GSD1B) is an inherited condition in which the body is unable to break down a complex sugar called glycogen. As a result, glycogen accumulates in cells throughout the body. In GSD1B, specifically, glycogen and fats build up within the liver and kidneys which can cause these organs to be enlarged ...
What is a GTR?
The Genetic Testing Registry (GTR) provides information about the genetic tests for this condition. The intended audience for the GTR is health care providers and researchers. Patients and consumers with specific questions about a genetic test should contact a health care provider or a genetics professional.
What is the HPO database?
People with the same disease may not have all the symptoms listed. This information comes from a database called the Human Phenotype Ontology (HPO) . The HPO collects information on symptoms that have been described in medical resources.
What do doctors look for in a diagnosis?
Healthcare professionals typically look at a person’s medical history, symptoms, physical exam, and laboratory test results in order to make a diagnosis.
Why is research important?
Research helps us better understand diseases and can lead to advances in diagnosis and treatment. This section provides resources to help you learn about medical research and ways to get involved.
When does a symtom develop?
Signs and symptoms of the condition generally develop at age 3 to 4 months and may include hypoglycemia, seizures, lactic acidosis, hyperuricemia (high levels of a waste product called uric acid in the body), and hyperlipidemia.
What is the NORD website?
NORD is a patient advocacy organization for individuals with rare diseases and the organizations that serve them.

Overview
Glycogen storage disease type I (GSD I) is an inherited disease that results in the liver being unable to properly break down stored glycogen. This impairment disrupts the liver's ability to break down stored glycogen that is necessary to maintain adequate blood sugar levels. GSD I is divided into two main types, GSD Ia and GSD Ib, which differ in cause, presentation, and treatment. GSD Ia is cau…
Signs and symptoms
Early research into GSD I identified numerous clinical manifestations falsely thought to be primary features of the genetic disorder. However, continuing research has revealed that these clinical features are the consequences of only one (in GSD Ia) or two (in GSD Ib) fundamental abnormalities:
• impairment in the liver's ability to convert stored glycogen into glucose through glycogenolysis
Early research into GSD I identified numerous clinical manifestations falsely thought to be primary features of the genetic disorder. However, continuing research has revealed that these clinical features are the consequences of only one (in GSD Ia) or two (in GSD Ib) fundamental abnormalities:
• impairment in the liver's ability to convert stored glycogen into glucose through glycogenolysis
Genetics
GSD I is inherited in an autosomal recessive manner. People with one copy of the faulty gene are carriersof the disease and have no symptoms. As with other autosomal recessive diseases, each child born to two carriers of the disease has a 25% chance of inheriting both copies of the faulty gene and manifesting the disease. Unaffected parents of a child with GSD I can be assumed to be ca…
Pathophysiology
Glycogen in liver and (to a lesser degree) kidneys serves as a form of stored, rapidly accessible glucose, so that the blood glucose level can be maintained between meals. For about 3 hours after a carbohydrate-containing meal, high insulin levels direct liver cells to take glucose from the blood, to convert it to glucose-6-phosphate (G6P) with the enzyme glucokinase, and to add the G6P …
Diagnosis
Several different problems may lead to the diagnosis, usually by two years of age:
• seizures or other manifestations of severe fasting hypoglycemia
• hepatomegaly with abdominal protuberance
• hyperventilation and apparent respiratory distress due to metabolic acidosis
Treatment
The primary treatment goal is prevention of hypoglycemia and the secondary metabolic derangements by frequent feedings of foods high in glucose or starch (which is readily digested to glucose). To compensate for the inability of the liver to provide sugar, the total amount of dietary carbohydrate should approximate the 24-hour glucose production rate. The diet should contain approximately 65–70% carbohydrate, 10–15% protein, and 20–25% fat. At least a third o…
Prognosis
Without adequate metabolic treatment, patients with GSD I have died in infancy or childhood of overwhelming hypoglycemia and acidosis. Those who survived were stunted in physical growth and delayed in puberty because of chronically low insulin levels. Intellectual disability resulting from recurrent, severe hypoglycemia is considered preventable with appropriate treatment.
Liver complications have been serious in some patients. Adenomasof the liver can develop in th…
Epidemiology
In the United States, GSD I has an incidence of approximately 1 in 50,000 to 100,000 births. None of the glycogenoses are currently detected by standard or extended newborn screening.
The disease is more common in people of Ashkenazi Jewish, Mexican, Chinese, and Japanese descent.