Bone disease (Osteodystrophy)
- Features of renal osteodystrophy. ...
- The major players in renal osteodystrophy are: Increased phosphate levels in the blood – this causes the parathyroid glands to produce more Parathyroid Hormone, PTH.
- Hyperparathyroidism. ...
- Adynamic bone disease. ...
- Other issues. ...
- Further info
What is osteodystrophy?
Osteodystrophy is any dystrophic growth of the bone. It is defective bone development that is usually attributable to renal disease or to disturbances in calcium and phosphorus metabolism . One form is renal osteodystrophy .
What causes renal osteodystrophy?
Causes of Renal Osteodystrophy Calcitriol Deficiency- Calcitriol is secreted by normal kidney from Vitamin D. Kidney disease often results in calcitriol deficiency as kidney fails to secrete normal quantity of calcitriol. Absence of Calcitriol in blood prevents calcium absorption from digested food in intestine.
How serious is renal osteodystrophy?
Renal Osteodystrophy tends to be more serious in children as the bones in their body are still in the growth phase. Symptoms of Renal Osteodystrophy can be observed in children with kidney diseases even before beginning dialysis. Renal Osteodystrophy slows down growth of bone and may also lead to other deformities of the bone.
What are the causes of osteoporosis?
As a cause of osteoporosis, this one's in your hands. You can help "remodel" your bones with weight-bearing exercise, where you're putting gentle stress on bones. High levels of thyroid hormone have long been linked to an increase in bone loss.

What is the cause of osteodystrophy associated with chronic renal failure?
Neoplasms of the parathyroid glands secreting PTH autonomously, an example of tertiary hyperparathyroidism, can lead to a high bone turnover state. Secondary hyperparathyroidism is the predominant cause of osteodystrophy.
What are the causes of renal osteodystrophy?
Renal osteodystrophy has been classically described to be the result of hyperparathyroidism secondary to hyperphosphatemia combined with hypocalcemia, both of which are due to decreased excretion of phosphate by the damaged kidney.
How is osteodystrophy treated?
The major treatment modalities for renal osteodystrophy include phosphate binders, vitamin D compounds, and calcimimetics. Aluminum-containing phosphate binders have been shown to be toxic to bone secondary to their effects on bone turnover, mineralization, and bone volume.
How can osteodystrophy be prevented?
Strategies for prevention in early, moderate, and end-stage renal failure are reviewed and discussed with particular reference to dietary phosphorus restriction, use of gut phosphorus binders, control of acidosis, calcium supplementation, use of oral and intravenous calcitriol, and use of synthetic analogues of 1,25- ...
How is osteodystrophy diagnosis?
How is renal osteodystrophy diagnosed? To diagnose renal osteodystrophy, your doctor may take a sample of your blood to measure levels of calcium, phosphorus, PTH, and calcitriol. The doctor may perform a bone biopsy to see how dense your bones are.
Can renal osteodystrophy be reversed?
Once the diagnosis is clear, all forms of renal osteodystrophy have many reversible causes; some remain “idiopathic,” however. Newer therapies such as vitamin D analogues or cinacalcet can mitigate one form of renal osteodystrophy: secondary hyperparathyroidism.
Is renal osteodystrophy painful?
Symptoms of renal osteodystrophy Renal osteodystrophy is often called the “silent crippler” because symptoms do not occur until a patient has been on dialysis for a few years. Typical symptoms can be: Bone pain. Joint pain.
Does kidney disease cause bone disease?
To keep your bones strong, your kidneys must keep the right balance of several important substances. These include phosphorus, calcium, parathyroid hormone, and vitamin D. When you have chronic kidney disease, your body no longer keeps the right balance of these substances. This can lead to bone disease.
Can kidney problems cause bone pain?
Bone disease can happen in the early stages of CKD. However, most patients do not have symptoms or feelings of bone disease in the early stages. As phosphorus builds up in your body in late kidney disease, symptoms may include itching, bone pain, muscle weakness, fractures and joint pain.
Are calcium supplements hard on your kidneys?
Long-term calcium and vitamin D supplement use may be linked to increased risk of kidney stones. Summary: Calcium and vitamin D supplements are associated with high calcium levels in the blood and urine, which could increase the risk of kidney stones, a new study finds.
How is renal bone disease treated?
Treatment includes dietary advice and titrated doses of oral phosphate binders such as calcium salts, vitamin D analogues, sodium bicarbonate and cinacalcet. Dialysis is beneficial for patients with end-stage renal failure. Early referral to a nephrologist to guide monitoring and treatment is recommended.
Can you take calcium if you have kidney disease?
According to the National Kidney Foundation (NKF) clinical practice guidelines, also known as Kidney Disease Outcomes Quality Initiative (KDOQI), total calcium intake for people with renal disease should not be greater than 2,000 mg daily.
What is osteoporosis and what causes it?
Osteoporosis is a bone disease that develops when bone mineral density and bone mass decreases, or when the quality or structure of bone changes. This can lead to a decrease in bone strength that can increase the risk of fractures (broken bones).
What causes osteopetrosis?
Cause of Osteopetrosis We have two copies of most of our genes, one from each parent. People with osteopetrosis have a gene that causes the body to make too few or abnormal cells called osteoclasts. When the osteoclasts are missing, old bone is not broken down as new bone is made, leading to dense, weak bones.
What is hyperparathyroidism caused by?
Hyperparathyroidism is caused by factors that increase the production of parathyroid hormone. The parathyroid glands keep proper levels of both calcium and phosphorus in your body by turning the release of parathyroid hormone off or on.
What can cause your bones to break easily?
Overview. Osteoporosis causes bones to become weak and brittle — so brittle that a fall or even mild stresses such as bending over or coughing can cause a fracture. Osteoporosis-related fractures most commonly occur in the hip, wrist or spine.
What causes renal osteodystrophy?
The major players in renal osteodystrophy are: Increased phosphate levels in the blood – this causes the parathyroid glands to produce more Parathyroid Hormone, PTH. Healthy kidneys respond to PTH by putting out more phosphate in urine.
Why is vitamin D important for bone?
Active Vitamin D causes the gut to take in more calcium from food. Vitamin D is also necessary for normal bone formulation – without it you get rickets. In rickets bones don’t calcify properly. They may break or bend in growing children, to cause bow legs and other abnormalities.
Why does low calcium cause PTH?
Low calcium levels in the blood – caused by failure of the kidneys to process Vitamin D normally. Low calcium levels make the parathyroid glands produce more PTH.
How to treat phosphate?
Treatment: Phosphate comes from what you eat, so cutting down on foods that are high in phosphate and taking “phosphate binders” with food help. If you are on dialysis, more dialysis is likely to help – especially long or frequent dialysis treatments (phosphate is removed slowly by conventional dialysis).
What happens when calcium is released from bones?
After a long period it gets out of control and becomes less responsive to calcium levels, even causing high blood calcium, (‘Tertiary hyperthyroidism).
Does PTH cause uraemic syndrome?
Prevention is through control of calcium and phosphate levels. PTH has been suspected of causing various other elements of ‘uraemic syndrome’, but its role in most of them is speculative.
Is adynamic bone disease a phosphate binder?
Thought to be at least partially due to over-suppression of PTH by excessive use of vitamin D therapy. In the past aluminium toxicity (from dialysis and use of aluminium hydroxide as a phosphate binder) may have contributed to this.
What causes renal osteostrophy?
Causes of Renal Osteodystrophy. Calcitriol Deficiency -. Calcitriol is secreted by normal kidney from Vitamin D. Kidney disease often results in calcitriol deficiency as kidney fails to secrete normal quantity of calcitriol. Absence of Calcitriol in blood prevents calcium absorption from digested food in intestine.
How Do We Define Renal Osteodystrophy?
Renal Osteodystrophy (RD)- Renal Osteodystrophy is a pathological condition of the bone, which tends to occur when the kidneys are unable to maintain adequate levels of calcium and phosphorus in the bloodstream.
What causes bone depletion?
Renal Osteodystrophy causes a depletion of bone minerals. Kidney fails to maintain normal level of calcium and phosphorous in blood. The abnormal blood level of calcium and phosphorous causes hormonal changes, which follows demineralization of bone. The disease is observed in patients undergoing regular dialysis.
Why is renal osteodystrophy called renal osteodystrophy?
The disease is known as Renal Osteodystrophy because renal disease induces the cascade to cause demineralization of bone.
What causes calcium to be removed from bones?
Increased Parathyroid hormone in circulating blood causes removal of calcium from bone in to blood so as to maintain normal blood level of calcium. Removal of calcium from bones causes Osteodystrophy. The disease is known as Renal Osteodystrophy because renal disease induces the cascade to cause demineralization of bone.
What is a bone deformity that slows down growth?
Renal Osteodystrophy slows down growth of bone and may also lead to other deformities of the bone. An example of such deformity is bowed leg where the legs are bent inwards or outwards. The skeletal abnormalities are known as Renal Rickets.
What causes hypocalcaemia in the body?
High parathyroid hormone causes hypocalcaemia, which follows demineralization of calcium from bones.
What is the primary cause of osteodystrophy?
Secondary hyperparathyroidism is the predominant cause of osteodystrophy. The different factors involved in the pathway building up to secondary hyperparathyroidism are also worth mentioning in the etiology of renal osteodystrophy:
Why is renal osteodystrophy accelerated?
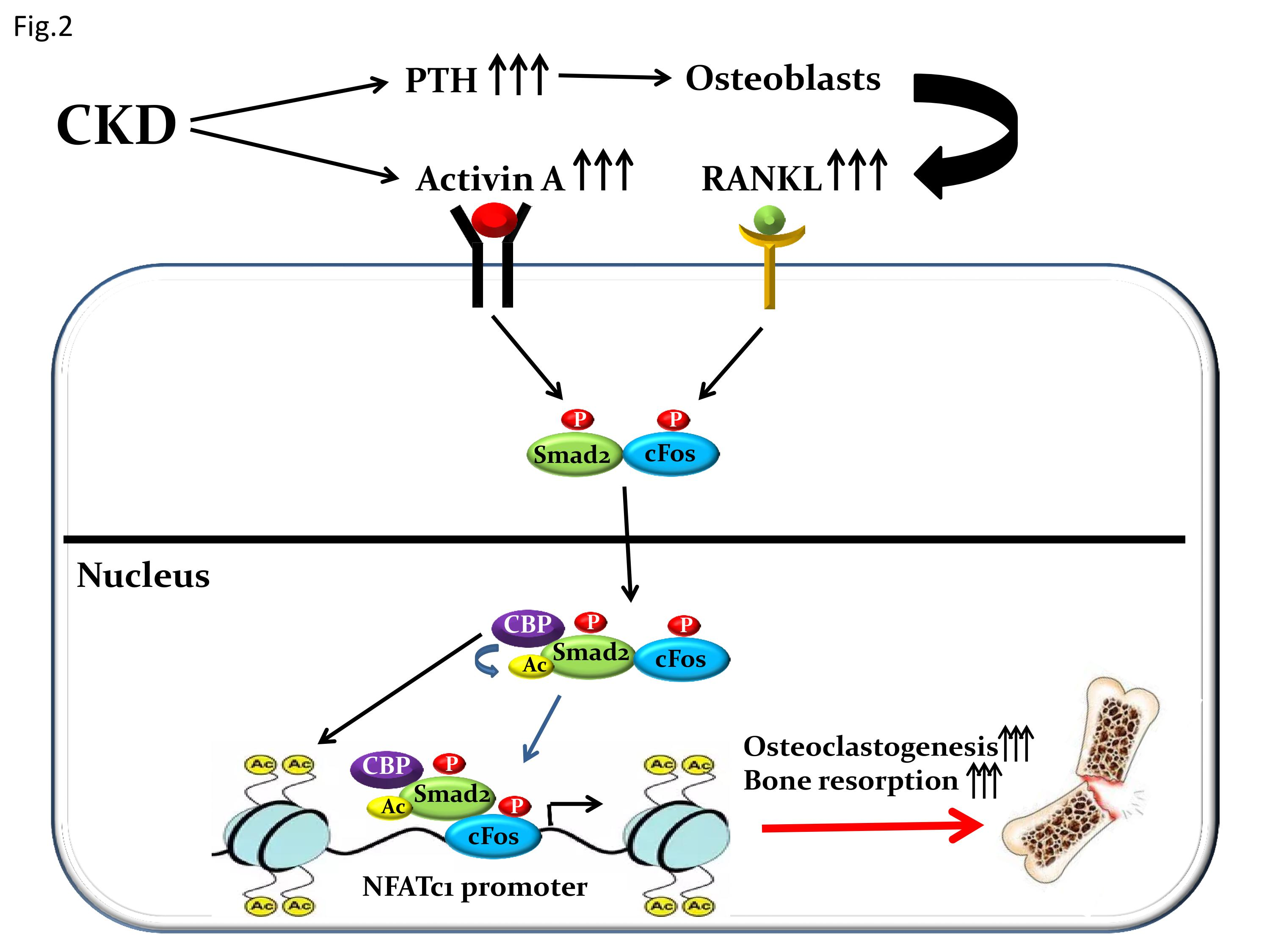
Patients suffering from chronic kidney disease (CKD) have an accelerated disease process due to the alteration in levels of other factors like phosphate, calcium, and vitamin D along with PTH. High bone turnover states involving an increased PTH act through the RANK complex to activate more osteoclasts. On the other hand, low bone turnover states have lower than normal PTH levels, which renders the bone incapable of integrating calcium into the new bone that is being formed.
What is the predominant histological bone pattern in renal osteodystrophy?
The predominant histological bone pattern in renal osteodystrophy is osteitis fibrosa, which is a product of high bone turnover due to secondary hyperparathyroidism. Along with the PTH level, secondary factors that play a role in the development of osteitis fibrosa include interleukins 1, 6, and TNF-alpha. [4]
What is renal osteodystrophy?
Renal osteodystrophy is a broad term that incorporates all the biochemical abnormalities and skeletal manifestations in patients suffering from chronic kidney disease or end-stage renal disease. The derangements in the serum levels of calcium, phosphorous, PTH, vitamin D, along with their effects on bone turnover, mineralization, and extraskeletal calcifications, are all important components of this condition. Reports suggest these abnormalities are most likely to be seen at a GFR below 60 mL/min/1.73 m2.[1][2]
What are the two main cells that are involved in the process of bone remodeling?
The two main cells in this process are osteoclasts that cut down or resorb the bone and osteoblasts that build-up or form new bone.[10] Osteoblasts produce the organic matrix of the bone consisting of type 1 collagen along with other non-collagenous proteins like alkaline phosphatase and osteocalcin. [11]
Is osteodystrophy a complication of end stage renal disease?
The development of renal osteodystrophy as a complication of end-stage renal disease has also influenced changes in the treatment protocols and dialysis regimens in patients.
Is renal osteodystrophy a complication?
Renal osteodystrophy is one of the main complications of end-stage renal disease that leads to skeletal and extraskeletal manifestations. Although it may be unavoidable in patients undergoing hemodialysis, appropriate and timely interventions can help alleviate the symptoms experienced by the patients and also reduce the osteodystrophy-related comorbidities. This activity reviews the evaluation and management of renal osteodystrophy and explains the role of the interprofessional team in improving the care of patients with this condition.
How to treat renal osteodystrophy?
The goal of treating renal osteodystrophy is to restore balance between calcium, PTH, phosphorus and vitamin D in the body. Renal osteodystrophy can be managed with phosphorus binders, activated vitamin D and a low-phosphorus diet. If you have a high level of PTH in your blood, it’s important to bring it back to a normal level to prevent calcium loss from your bones. Medicines to treat renal osteodystrophy can be given in pill form, but are usually given intravenously during dialysis treatments for people on in-center hemodialysis. These medicines are only used in people with kidney disease. Another drug that may be used acts directly on the parathyroid glands to block PTH release. In severe cases the parathyroid glands may be surgically removed.
Why are children with kidney disease especially affected by renal osteodystrophy?
Children with kidney disease can be especially affected by renal osteodystrophy because their bones are still growing.
What is the name of the bone cells that are not in balance?
In people with bone disease related to kidney failure, bone cells called osteoclasts and osteoblasts are often not in balance. This condition is called renal osteodystrophy. The way these bone cells get out of balance is when calcium, parathyroid hormone (PTH), phosphorus and activated vitamin D are out of balance.
Why does the body pull calcium from bones?
A high blood phosphorus level causes your body to pull calcium from your bones in an attempt to balance all the body’s minerals. When calcium is being pulled from your bones, your bones begin to break down and lose the ability to provide structural support.
Why is it important to have healthy bones?
Having healthy bones is essential to maintaining body structure and mobility. The human skeleton supports body weight and protects the brain and other organs. The skeleton also stores two important minerals— calcium and phosphorus. In people with bone disease related to kidney failure, bone cells called osteoclasts and osteoblasts are often not in ...
How to increase bone strength?
In addition to a low-phosphorus diet and taking prescribed medicines, exercise can also help increase your bone strength. Check with your doctor before beginning an exercise program.
Can osteodystrophy cause bone loss?
Over time, renal osteodystrophy can cause bones to break easily, harden the soft tissues of the body including the heart and may even lead to a higher death rate in people with end stage renal disease (ESRD).
What causes osteodystrophy?
Causes. hyperphosphatemia. Osteodystrophy is any dystrophic growth of the bone. It is defective bone development that is usually attributable to renal disease or to disturbances in calcium and phosphorus metabolism . One form is renal osteodystrophy .
What is the term for a defective bone that is attributable to renal disease?
Unsourced or poorly sourced material may be challenged and removed. Osteodystrophy is any dystrophic growth of the bone. It is defective bone development that is usually attributable to renal disease or to disturbances in calcium and phosphorus metabolism . One form is renal osteodystrophy .
What are the factors that increase the risk of osteoporosis?
A number of factors can increase the likelihood that you'll develop osteoporosis — including your age, race, lifestyle choices, and medical conditions and treatments.
How likely is it to develop osteoporosis?
How likely you are to develop osteoporosis depends partly on how much bone mass you attained in your youth. Peak bone mass is somewhat inherited and varies also by ethnic group. The higher your peak bone mass, the more bone you have "in the bank" and the less likely you are to develop osteoporosis as you age.
What causes a fracture in the hip?
Osteoporosis causes bones to become weak and brittle — so brittle that a fall or even mild stresses such as bending over or coughing can cause a fracture. Osteoporosis-related fractures most commonly occur in the hip, wrist or spine.
How do you know if you have bone loss?
There typically are no symptoms in the early stages of bone loss. But once your bones have been weakened by osteoporosis, you might have signs and symptoms that include: Back pain, caused by a fractured or collapsed vertebra. Loss of height over time. A stooped posture.
How to reduce risk of falling?
Balance exercises such as tai chi can reduce your risk of falling especially as you get older. Swimming, cycling and exercising on machines such as elliptical trainers can provide a good cardiovascular workout, but they don't improve bone health. By Mayo Clinic Staff. Request an Appointment at Mayo Clinic.
What are some examples of osteoporosis?
Examples include: Sex hormones. Lowered sex hormone levels tend to weaken bone. The reduction of estrogen levels in women at menopause is one of the strongest risk factors for developing osteoporosis. Men have a gradual reduction in testosterone levels as they age.
How many alcoholic drinks a day can cause osteoporosis?
Excessive alcohol consumption. Regular consumption of more than two alcoholic drinks a day increases the risk of osteoporosis.
What is the most common cause of osteoporosis?
What’s the most common cause of osteoporosis? "In general, it's estrogen deficiency in women," says Paul Mystkowski, MD, an endocrinologist at Virginia Mason Medical Center in Seattle and clinical faculty member of the University of Washington in Seattle. Bone loss accelerates after menopause, when older women have a quick drop in estrogen. Over time, the risk of osteoporosis and fracture increases as older women lose more bone than they replace.
Why do men have osteoporosis?
Men need both testosterone and estrogen for bone health. That's because men convert testosterone into bone-preserving estrogen. "There's a clear consensus that when you're evaluating men with osteoporosis," says Mystkowski, "you always evaluate for testosterone deficiency.".
How often do bones change?
Bones continually change throughout your life, with some bone cells dissolving and new bone cells growing back in a process called remodeling. With this lifelong turnover of bone cells, you replace most of your skeleton every 10 years. But for people with osteoporosis -- a thinning of the bones -- bone loss outpaces the growth of new bone.
What happens to bone mass as you age?
Bone density is greatest in your early 20s. But as you age, you can lose bone mass from a variety of factors. Osteoporosis or its early warning sign, osteopenia, signals an imbalance in the remodeling process: Too much bone is broken down, and too little new bone is built back up. Brittle bones result, prone to fracture.
Why do people lose their bones?
For people who are sedentary or have a condition like paralysis or muscular dystrophy, bone loss happens quickly. As a cause of osteoporosis, this one's in your hands. You can help "remodel" your bones with weight-bearing exercise, where you're putting gentle stress on bones. Causes of Osteoporosis: Thyroid Conditions.
Why do bones get brittle?
Brittle bones result, prone to fracture. You probably know that you need calcium to build strong bones, but a low- calcium diet isn't the only culprit. There are lesser-known causes of osteoporosis. The experts now believe that a combination of causes is often to blame for bone loss.
How many people have osteoporosis?
But look at a hip with osteoporosis, and you see mostly air. The bony matrix has all but dissolved, with only a few thin strands left. As many as 10 million Americans have osteoporosis and 34 million more have low bone mass, called osteopenia, says the National Osteoporosis Foundation.
