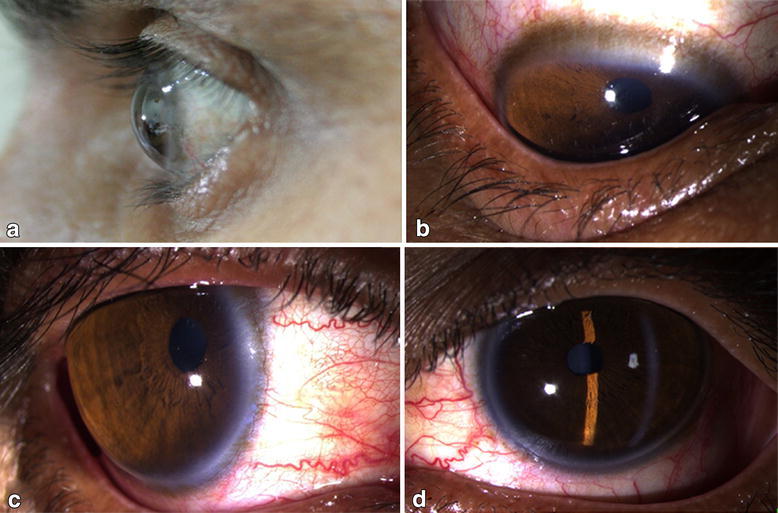
Inflammatory corneal disorders can cause thinning with stromal melting. These conditions are often associated with pain, epithelial defects, corneal neovascularization, and other inflammatory changes. Progression is fast and emergent treatment is warranted upon diagnosis.
What are the symptoms of a torn cornea?
Symptoms . If you have a corneal abrasion, you'll probably be in a great deal of pain. You may experience light sensitivity, blurry vision, foreign body sensation, sandy-gritty feeling or eye redness. You may also find it difficult to hold your eye open, and doing so may result in excessive tearing.
What is a thin cornea?
Keratoconus (ker-uh-toe-KOH-nus) occurs when your cornea — the clear, dome-shaped front surface of your eye — thins and gradually bulges outward into a cone shape. A cone-shaped cornea causes blurred vision and may cause sensitivity to light and glare. Click to see full answer. In this manner, what causes cornea to change shape?
Can spots on the cornea affect my vision?
The spots on the cornea are an allergic response to viral antigen. Spots can increase, cause blurring of vision etc., but tend to fade over 3-4 months. Low dose steroids and lubricating drops give a good clinical response. You can continue to do all activities, take steam/head bath etc.
What is peripheral corneal degeneration?
What is peripheral corneal degeneration? Terrien marginal degeneration is a painless, slowly progressive thinning of the peripheral corneal stroma. It is usually bilateral but may be asymmetric. As opposed to other causes of peripheral corneal thinning, there is typically no inflammation and the corneal epithelium remains intact.

How do I fix my thinning cornea?
Vision Correction Options for Patients With Thin CorneasThin Corneas and LASIK.PRK. Photorefractive keratectomy, or PRK, is a type of laser eye surgery that serves as an alternative for those not suited to LASIK due to thin corneas. ... Lens Replacement Surgery. ... Implantable Lenses. ... Contact Schwartz Laser Eye Center.
Is thin cornea serious?
Thinning corneas can lead to serious vision complications and even vision loss. Fortunately, you have plenty of treatments available to preserve your sight. While severe cases may require a corneal transplant, many can be treated with special contact lenses just for keratoconic eyes.
Can you go blind from thin cornea?
Without treatment, you are likely to experience a thinning cornea or a bulging cornea. Both are irreversible. You may not go blind, but your vision will get worse, and you likely will have increase eye pain over time.
How common are thin corneas?
Interestingly, 23% of participants (38 of 168 eyes) had clinically thin corneas, defined by a total central corneal thickness value of less than 500 μm; 28% of females (32 eyes) examined had thin corneas, whereas only 12% of males (6 eyes) were clinically thin (P<0.001, chi-square test).
Does your cornea thin as you age?
Thinning of the cornea at a rate of 3–7 μm per decade has been observed in older age in some ethnic groups. A study in 1998 with 1,242 participants aged 10–87 years showed that CCT decreased by 5–6 μm for each decade of life.
Can you have laser eye surgery if you have thin corneas?
Your corneas are too thin If your corneas are too thin, you cannot safely have the LASIK procedure. During LASIK, you must have enough corneal tissue, as it is reshaped during the procedure. If your corneas are too thin, getting LASIK could cause severe vision complications.
Can cornea repair itself?
The cornea can often repair itself after injury or disease, but more serious conditions -- infections, degenerative diseases, deterioration -- need treatment.
At what age keratoconus stops?
NEW YORK (Reuters Health) - Although keratoconus is often thought to stop progressing by the time patients are 30 to 40 years old, the corneal degeneration often continues beyond this point, according to researchers from New Zealand.
Can cornea repair itself?
The cornea can often repair itself after injury or disease, but more serious conditions -- infections, degenerative diseases, deterioration -- need treatment.
How thick should your cornea be?
between 520 microns and 540 micronsThe average corneal thickness is between 520 microns and 540 microns, however, the normal range for cornea thickness can range from as thin as 470 to as thick as 630 microns.
Can you have laser eye surgery if you have thin corneas?
Your corneas are too thin If your corneas are too thin, you cannot safely have the LASIK procedure. During LASIK, you must have enough corneal tissue, as it is reshaped during the procedure. If your corneas are too thin, getting LASIK could cause severe vision complications.
Does wearing contacts thin cornea?
Conclusions: Soft contact lenses and rigid gas-permeable contact lenses cause corneal thickening and corneal flattening in the first months, but they cause corneal thinning and corneal steepening with time. These alterations can be evaluated as evidence that contact lenses negatively influence corneal physiology.
What is the condition where the cornea bulges outward?
A notable condition of corneal ectasia is keratoconus, where the cornea bulges outward, which can lead to worsening one’s vision. People also consider alternative procedures such as LASEK, Epi-Lasik and PRK, but each of these involves removing tissue from the eye using a laser or blade.
What is the cornea?
The cornea is the transparent eye tissue that is located on the outermost layer of your eye. It functions to protect your eyes from dirt and germs along with filtering out small sounds of UV light. Thin corneas are when the thickness falls below 500 microns (half a millimeter) since the average normal thickness of a cornea is about 540 microns. 1.
What is the procedure called when you remove the cornea?
LASIK. With the similar-sounding LASEK procedure, eye drops loosen the cells on top of the cornea, the cells are scraped to the side, a laser is applied to reshape the cornea, cells are smoothed back on and a contact lens is placed on top to help the healing.
How long does it take for a corneal flap to heal?
Final results of the procedure are usually seen as soon as three days and up to 3 - 6 months for one’s vision to completely stabilize.
How does lasik affect the cornea?
The cornea is altered when LASIK is performed since it is responsible for how light enters your eye, influencing one’s scope of vision. During a LASIK procedure, the surgeon cuts a flap into the cornea, unhinges it and then uses a laser to cut away tissue to reshape it.
Can you remove a thin cornea?
Possibly one of the strongest choices for people with thin corneas is Visian Implantable Collamer Lenses, a procedure that uses a biocompatible, advanced lens rather than cutting away eye tissue. As a bonus, the lens provides UV protection and does not promote dry eye syndrome. If needed, the lens can be removed. Results can usually be seen within the next few days after the 20 - 30 minute procedure.
1. Glasses and Contact Lenses
Keratoconus can be treated with standard prescription glasses and soft contact lenses during its initial stages. As Dr.
2. Gas Permeable Contact Lenses
As it progresses, regular prescription eyeglasses and soft contacts don’t usually provide keratoconus sufferers with the same clear vision as specialized contact lenses. That’s why gas-permeable contact lenses are a preferred treatment option.
3. Scleral Contact Lenses
Scleral and semi-scleral contact lenses have larger diameters than other contacts to cover more of the sclera, or the white part, of your eye. Scleral lenses cover more of your eye while semi-scleral lenses cover a smaller portion.
4. Hybrid Contact Lenses
Specifically designed for keratoconic eyes, hybrid contact lenses provide a highly oxygen-permeable center with a soft peripheral “skirt.” Thanks to their gas-permeable center, hybrid lenses provide clear vision for wearers. Combined with soft lenses, they also give you a level of comfort that’s unmatched by some other options.
5. Intacs
Sometimes contacts won’t fit an eye due to irregularly shaped corneas. In this case, a procedure known as Intacs can be performed to improve your vision. During this procedure, a pair of tiny implants are placed into the cornea to help give it a more regular shape.
6. Collagen Crosslinking
If keratoconus continues to progress then your eye doctor may recommend collagen crosslinking. In this procedure, the cornea is made more rigid to prevent further irregularities by applying vitamin riboflavin and UV light. When performed, this procedure causes the collagen fibrils to shorten and thicken, making your cornea stronger than before.
7. Corneal Transplant & Penetrating Keratoplasty
A corneal transplant is ideal if you don’t get positive results from contact lenses or other therapies. In these cases, a transplant is the best option in order to restore your vision. Also known as penetrating keratoplasty (PK or PKP for short), you may still require glasses or contacts to see clearly after your surgery.
What happens if you have thin corneas?
The space between the cornea and your iris contains fluid called aqueous humor that nourishes the surrounding tissues. If you have thin corneas, you may have an increased risk for corneal damage or misdiagnosis of eye conditions.
What is the test that a doctor will perform to determine the thickness of the cornea?
She will perform a quick measurement in her office, a test called corneal pachymetry, that will measure the exact thickness, and this will help you and your doctor determine any possible risks.
What does eye pressure mean?
An eye pressure reading measures the pressure created from the aqueous humor filling the area between your cornea and iris. A thin cornea may give a low reading for an eye pressure, even if you have a high intraocular pressure. Due to this, early signs of glaucoma could go undetected. Glaucoma, an eye condition resulting from high intraocular ...
Does eating antioxidants help with corneal breakdown?
However, consuming foods rich in antioxidants could help to prevent the breakdown of corneal tissues.
Can a thin cornea show up in an eye exam?
A thin cornea will often not show any signs of a problem, but your eye doctor may note your corneal thickness during an eye examination.
Does eating thicken your cornea?
Learn More. The foods you eat will not add thickness to your cornea. However, consuming foods rich in antioxidants could help to prevent the breakdown of corneal tissues. Oxidative stress occurs when abnormal oxygen molecules called free radicals damage cells, and this, in turn affects the health of the tissues.
Can you touch your cornea?
You will not feel the touch of the device. The eye doctor may touch your cornea a few times, taking multiple measurements to ensure accuracy. After she moves away from your eye, the test is complete, and your doctor will discuss her findings. If you do not know whether you have thin corneas, talk to your eye doctor.
What is the cornea?
Corneal Opacity . Cornea Transplant Surgery . Keratitis . The cornea is your eye’s clear, protective outer layer. Along with the sclera (the white of your eye), it serves as a barrier against dirt, germs, and other things that can cause damage.
How does the cornea help you focus?
It also plays a key role in vision. As light enters your eye, it gets refracted, or bent , by the cornea’s curved edge. This helps determine how well your eye can focus on objects close-up and far away.
What Conditions Can Cause Damage?
They can get in after an injury and cause infection, inflammation, and ulcers. If your contact lenses cause an eye injury, that, too, can lead to keratitis.
Why do I get cold sores on my eye?
The main cause is the herpes simplex virusI (HSV I), the same one that leads to cold sores. It can also result from the sexually transmitted herpes simplex virus II (HSV II) that causes genital herpes. This condition creates sores on the cornea. Over time, the inflammation can spread deeper into your cornea and eye.
Why is my vision blurry?
As your cornea changes, your vision may get blurry. You may also notice:
How many corneal diseases are there?
Corneal Dystrophies: There are more than 20 of these diseases. They cause structural problems within your cornea. Some of the most common are:
What causes maps, dots, and small fingerprints?
It grows irregularly (thick in some places, thin in others). That causes irregularities in your cornea that look like maps, dots, and small fingerprints.
What causes corneal scarring?
Injuries . Small abrasions (scratches) on the cornea usually heal on their own. Deeper scratches or other injuries can cause corneal scarring and vision problems. Allergies .
How to prevent corneal injury?
To prevent corneal injuries, wear protective eyewear when you: Play sports that use a ball or puck, like baseball or hockey. Do yardwork, like mowing the lawn or using a weedwhacker. Make repairs, like painting or hammering. Use machines, like sanders or drills. Use chemicals, like bleach or pesticides.
What is the treatment for corneal dystrophies?
Laser treatment. To treat some corneal dystrophies and other conditions, doctors can use a type of laser treatment called phototherapeutic keratectomy (PTK) to reshape the cornea, remove scar tissue, and make vision clearer. Corneal transplant surgery.
What causes cloudy vision?
Corneal dystrophies cause cloudy vision when material builds up on the cornea. These diseases usually run in families. There are also a number of less common diseases that can affect the cornea — including ocular herpes, Stevens-Johnson Syndrome, iridocorneal endothelial syndrome, and pterygium.
What to do if cornea can't be repaired?
If the damage to your cornea can’t be repaired, doctors can remove the damaged part and replace it with healthy corneal tissue from a donor.
What causes dry eye?
Learn more about contact lens-related infections. Dry eye . Dry eye happens when your eyes don’t make enough tears to stay wet. This can be uncomfortable and may cause vision problems. Learn more about dry eye. Corneal dystrophies . Corneal dystrophies cause cloudy vision when material builds up on the cornea.
What is the name of the artificial cornea?
Artificial cornea. As an alternative to corneal transplant, doctors can replace a damaged cornea with an artificial cornea, called a keratoprosthesis (KPro).
What causes corneal scarring?from nei.nih.gov
Injuries . Small abrasions (scratches) on the cornea usually heal on their own. Deeper scratches or other injuries can cause corneal scarring and vision problems. Allergies .
What happens when your cornea changes?from webmd.com
It can also change your cornea's normal curve and cause astigmatism, nearsightedness, or farsightedness. As your cornea changes, your vision may get blurry. You may also notice: Moderate to severe pain. Increased sensitivity to light. Excessive tearing. A feeling that something is in your eye.
What Conditions Can Cause Damage?from webmd.com
They can get in after an injury and cause infection, inflammation, and ulcers. If your contact lenses cause an eye injury, that, too, can lead to keratitis.
How far can keratocytes project?from sciencedirect.com
2001 ), which may allow different stromal levels to communicate with each other. These can project 30–50 µm from the cell body. Thus an individual cell can bridge a corneal distance of about 100 µm, which is unusual for a non-neural cell but useful to maintain a transcorneal communicating network.
How thick is the cornea after PK?from sciencedirect.com
Bourne (1983) showed that in a group of 231 PK eyes, average central corneal thickness (CCT) was 540 ± 60 µm with a range of 420–740 µm measured 2 months postoperatively. Kus et al. (1999) showed corneal thickness following PK after a follow-up of 22 years was 608 ± 75 µm. Sarnicola et al. (2010) showed in a retrospective evaluation of 236 DALK procedures between 2000 and 2006 that the average central corneal thickness after surgery was 584 ± 49 µm. The observed changes relate to corneal swelling at the time of surgery, followed by reduction in thickness due to topical steroid use. Essentially, the corneal thickness is likely to be thicker than a typical cornea following PKs and DALK; therefore pachymetry should be measured and noted in view of possible endothelial changes.
Why is corneal thickness important?from sciencedirect.com
In keratoconus, knowing the corneal thickness assists in determining which patients may be candidates for corneal collagen cross-linking. If the cornea is too thin, cross-linking may be contraindicated. Monitoring corneal thickness also assists in knowledge of the corneal thinning and progression of the disease over time. For corneal transplant patients, increased corneal thickness over time is an indication of either rejection ( Larkin, 1994) or graft failure ( Sugar, 2015 ). Global corneal thickness is easily provided from the Sheimpflug or slit-scanning-based elevation topography or anterior-segment optical coherence tomography ( Fig. 39.12 ). However, clinicians should be aware that corneal thickness measurements are influenced by the method of measurement and that, although highly correlated, instruments such as ultrasound pachymetry, anterior-segment optical coherence tomography and topography should not be used interchangeably for the assessment of corneal thickness ( Li et al., 2007 ).
Why do I get cold sores on my eye?from webmd.com
The main cause is the herpes simplex virusI (HSV I), the same one that leads to cold sores. It can also result from the sexually transmitted herpes simplex virus II (HSV II) that causes genital herpes. This condition creates sores on the cornea. Over time, the inflammation can spread deeper into your cornea and eye.
What causes corneal stromal melting?
Inflammatory corneal disorders can cause thinning with stromal melting. These conditions are often associated with pain, epithelial defects, corneal neovascularization, and other inflammatory changes. Progression is fast and emergent treatment is warranted upon diagnosis.
How to treat perforation in the eye?
A protective shield should be kept in place at all times. Preservative-free artificial tears applied frequently will aid in lubrication with a bandage lens in place. Patients also benefit from oral doxycycline because of its ability to inhibit collagenase. Depending on the cause, infected perforations are treated with frequent fortified antibacterial, antiviral, or antifungal therapy. Initially, patients should be examined daily, and any complaints of decreased vision, pain, tearing, or photophobia should be attended to immediately. If the bandage lens falls out, it must be replaced. If the glue becomes dislodged, reapplication is often necessary.
What is the goal of local ocular treatment?
The goals of local (ocular) treatment are to (1) provide local supportive therapy to decrease corneal melting; and (2) promote re-epithelization of the corneal surface.
Can you use tissue adhesive on a Frank corneal perforation?
Unless contraindicated, an air bubble can be placed into the anterior chamber to temporarily occlude the perforation by surface tension. Larger air bubbles risk pupillary block and increased intraocular pressure (IOP), so caution must be exercised. In eyes with flat anterior chambers, to avoid incarceration of uveal tissue or the lens, viscoelastic material may be injected into the anterior chamber.
Does fibrin glue cause neovascularization?
Studies have shown that fibrin glue causes less neovascularization ; however, a longer time is required for the adhesive plug to form. Application of fibrin glue has been shown to be successful with the additional placement of amniotic membrane grafts for structural support of a perforated cornea.
Can a corneal patch graft be used for a perforation?
4.31.3 ). These procedures can temporarily stabilize a perforation or descemetocele or may be a permanent treatment. It is ideal for peripheral pathology. Care should be taken when used for central pathology because it can interfere with visual outcome.
Why is Corneal Thickness Important?
Corneal thickness is important because it can mask an accurate reading of eye pressure, causing doctors to treat you for a condition that may not really exist or to treat you unnecessarily when are normal. Actual IOP may be underestimated in patients with thinner CCT, and overestimated in patients with thicker CCT.
A Thin Cornea – The Danger of Misreading Eye Pressure
Many times, patients with thin corneas (less than 555 µm) show artificially low IOP readings. This is dangerous because if your actual IOP is higher than your reading shows, you may be at risk for developing glaucoma and your doctor may not know it. Left untreated, high IOP can lead to glaucoma and vision loss.
A Thicker Cornea – May Mean Less Reason to Worry About Glaucoma
Those patients with thicker CCT may show a higher reading of IOP than actually exists. This means their eye pressure is lower than thought, a lower IOP means that risk for developing glaucoma is lowered. However, it is still important to have regular eye exams to monitor eye pressure and stay aware of changes.
Pachymetry – A Simple Test to Determine Corneal Thickness
A pachymetry test is a simple, quick, painless test to measure the thickness of your cornea. With this measurement, your doctor can better understand your IOP reading, and develop a treatment plan that is right for your condition. The procedure takes only about a minute to measure both eyes.
Who is at Risk for Glaucoma?
People at high risk for glaucoma includes people with increased eye pressure; everyone over the age of 60; people of African descent over the age of 40; and people who have a family history of glaucoma.
Why is my cornea scarred?
Advanced keratoconus also may cause your cornea to become scarred, particularly where the cone is most prominent. A scarred cornea causes worsening vision problems and may require cornea transplant surgery.
Why does my cornea swell?
This is caused by a condition in which the inside lining of your cornea breaks down, allowing fluid to enter the cornea (hydrops). The swelling usually subsides by itself, but a scar may form that affects your vision.
Why is my eye distorted?
In keratoconus, your cornea thins and gradually bulges outward into a cone shape. This can cause blurry, distorted vision.
What is the treatment for keratoconus?
If your condition progresses to an advanced stage, you may need a cornea transplant . A new treatment called corneal collagen cross-linking may help to slow or stop keratoconus from progressing, possibly preventing the need for a future cornea transplant.
Why is my eyeight worse?
See your eye doctor (ophthalmologist or optometrist) if your eyesight is worsening rapidly, which might be caused by an irregular curvature of the eye (astigmatism). He or she may also look for signs of keratoconus during routine eye exams.
What are the risk factors for keratoconus?
These factors can increase your chances of developing keratoconus: Having a family history of keratoconus. Rubbing your eyes vigorously. Having certain conditions, such as retinitis pigmentosa, Down syndrome, Ehlers-Danlos syndrome, hay fever and asthma.
How long does keratoconus last?
The condition may progress slowly for 10 years or longer . In the early stages of keratoconus, you might be able to correct vision problems with glasses or soft contact lenses. Later, you may have to be fitted with rigid, gas permeable contact lenses or other types of lenses, such as scleral lenses.