
It can occur due to a number of issues and conditions, including:
- Poorly fit contact lenses
- Incomplete lid closure ( lagophthalmos)
- Blepharitis
- Allergic reaction to ingredients in eye drops, particularly preservatives
- Mechanical irritation to the eyes by an eyelash
- Dry eye syndrome
- Viral or bacterial infection
- Recurrent corneal erosions
What drugs can cause whorl keratopathy?
Amiodarone Verticillata – Whorl Keratopathy (Video) Drugs that can cause this pattern: CACTI Mneumonic: chloroquine, amiodarone, chlorpromazine, tamoxifen, indomethacin. In addition, you can presumably get a similar pattern with amodiaquine, meperidine, and with Fabry’s disease.
What is whorl keratopathy?
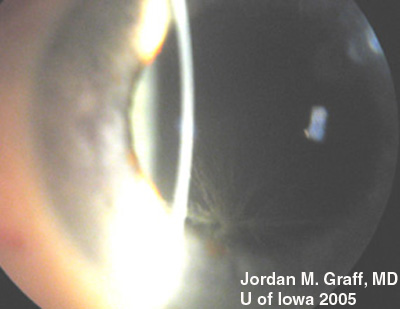
This cornea has a subtle finding of linear deposits on the surface epithelium. This is called whorl keratopathy (also known as hurricane keratopathy or verticillata) and occurs secondary to several medications. This finding is usually subtle, and doesn’t seem to cause any visual symptoms.
What is keratopathy and what causes it?
The literal meaning of keratopathy is a disease of the cornea. Each keratopathy is seen in association with different clinical scenarios. Some may represent some local causes whereas some may point at systemic causes.
What are the causes of bullous keratopathy?
Occasionally, bullous keratopathy may be caused by a corneal dystrophy. Corneal dystrophies are a group of genetic conditions that result in abnormal material accumulating within the cornea. Rarely, a few other eye conditions or blunt-force trauma to the eye can cause bullous keratopathy.
What is Cornea verticillata associated with?
How to identify drug-induced cornea verticillata?
What is the name of the disease that causes brown opacities in the cornea?
What are the differences between Fabry disease and slitlamp microscopy?
What are the properties of cornea verticillata?
Can cornea verticillata cause eye pain?
Is there a treatment for cornea verticillata?
See 4 more
About this website
What drugs causes whorl keratopathy?
Drugs associated with vortex keratopathy:Amiodarone. Effects 98% of patients on doses 200-300 mg a day or greater. ... Aminoquinolones (chloroquine, hydroxychloroquine, amodiaquine, quinacrine, tafenoquine) ... Atovaquone.Clofazimine.Gentamicin (Subconjunctival)Gold.Ibuprofen.Indomethacin.More items...
What causes corneal whorls?
The whorl-like pattern of cornea verticillata results from the centripetal migration of deposit-laden limbal stem cells as the corneal epithelium undergoes natural growth and repair.
What causes keratopathy?
Band Keratopathy is caused by an imbalance of calcium and phosphate that initiates deposition into the cornea.
What drugs cause vortex keratopathy?
Vortex keratopathy is commonly caused by certain cationic amphiphilic drugs such as amiodarone, antimalarials, suramin, tamoxifen, chlorpromazine and non-steroidal anti-inflammatory drugs. These deposits usually occur once a certain dose of the drug is reached.
How do you get rid of corneal arcus?
There's no treatment or cure for arcus senilis. But if you're experiencing arcus juvenilis, you may be at higher risk for coronary heart disease and high cholesterol....To reduce your cholesterol, there are some lifestyle changes that you can make:Eat healthier. ... Exercise more. ... Drink less alcohol. ... Stop smoking.
What does corneal arcus indicate?
In individuals under 40 years, corneal arcus is strongly associated with increased risk of coronary artery disease. If the corneal arcus is only present in one eye, then it may also be associated with carotid vascular disease.
What causes calcium build up around eyes?
Causes include autoimmune diseases like lupus, rheumatoid arthritis, and scleroderma as well as acne, skin infections, varicose veins, and burns.
Can too much calcium cause eye problems?
In a study published last month in the medical journal JAMA Ophthalmology, researchers found that people who take calcium supplements had a higher likelihood of developing age-related macular degeneration.
How do you treat calcium deposits in your eye?
The most common methods for removing the calcium deposits are mechanical debridement with a blade, chemical chelation with ethylenediaminetetraacetic acid (EDTA), and phototherapeutic keratectomy. Manual debridement of CBK by scraping with a blade is effective but can lead to an irregular corneal surface.
What medicines cause eye problems?
If you take any of these types of medicines, you could get dry eye:Diuretics.Antihistamines.Antidepressants.Cholesterol-lowering drugs.Beta-blockers.Birth control pills.
What drugs increase ocular pressure?
Steroids. Corticosteroids, or steroids, can raise eye pressure, especially in those persons who have open-angle glaucoma, first-degree relatives of those with open-angle glaucoma, elderly and young (<6 years) persons, those with type 1 diabetes and those with high myopia (short-sightedness).
How is keratopathy treated?
Band keratopathy treatment consists of a chemical treatment called chelation. Chelation is a chemical process that uses EDTA (ethylenediamine-tetraacetic acid) that chemically removes the calcium from the cornea.
Is corneal arcus rare?
The condition affects about 60 percent of the population between 50 and 60 years old. For persons over the age of 80, corneal arcus afflicts nearly 100 percent of those tested. The incidence is even higher in the African American population, although researchers aren't sure why.
What causes hair to grow on eyeball?
A rare tumor in a 19-year old man caused hair to grow on his eyeball, researchers report. The tumor, called a limbal dermoid, was benign and had been present since birth.
Does corneal arcus grow?
They can grow with time, and can eventually form a ring around the entire cornea. The diagnosis of corneal arcus is made visually by examination with a biomicroscope (slit lamp).
What causes spinners in the eyes?
What are the causes? Oscillopsia is caused by nervous system disorders that damage parts of the brain or inner ear that control eye movements and balance. One possible cause is the loss of your vestibulo-ocular reflex (VOR). This reflex makes your eyes move in coordination with the rotation of your head.
General information
Keratopathy is a group of diseases of acquired or congenital genesis, which are accompanied by a violation of the integrity of the surface layers of the cornea. Aphakic, pseudoaphakic, cordaronic and neurotrophic keratopathies most often develop in old age, due to organic changes in the organ of vision.
Causes
There is a clear connection between the etiology of keratopathy and its clinical form. The most common cause of the threadlike form of the disease is dry eye syndrome, often combined with autoimmune pathology (Sjogren’s syndrome).
Symptoms
From a clinical point of view, there are threadlike, exposure, neurotrophic, ribbon-like, aphakic, pseudoaphakic, cordaronic, lipoid, thermal, ultraviolet forms and surface point keratopathy of Tigeson. Common symptoms for all variants are hyperemia of the eyes, foreign body sensation, photophobia and pain in the eyes of varying intensity.
Diagnosis
The main methods of diagnosis of keratopathy are external eye examination and biomicroscopy using a slit lamp. Additionally, visometry, ophthalmoscopy and tonometry are performed. External examination with filamentous keratopathy allows you to identify short formations consisting of epithelial cells and mucus.
Treatment
In all forms of keratopathy, therapeutic measures should begin with etiotropic therapy of the underlying disease. Pathogenetic treatment is reduced to moisturizing the cornea (in the absence of defects) with artificial tear preparations and moisturizing ointments.
Prognosis and prevention
Specific measures for the prevention of keratopathy have not been developed. Patients are advised to monitor eye hygiene. With prolonged visual load, special means should be used to moisturize the cornea, do gymnastics and short breaks.
What is Cornea verticillata associated with?
Cornea verticillata is most commonly associated with amiodarone and Fabry disease.
How to identify drug-induced cornea verticillata?
The etiology of drug-induced forms of cornea verticillata can typically be identified with a thorough review of the patient’s medical history and medications. If attempting to differentiate between drug-induced cornea verticillata and that caused by Fabry disease, the microstructure of the deposits can be viewed with confocal laser scanning microscopy. However, this is not a routine part of the diagnostic evaluation.
What is the name of the disease that causes brown opacities in the cornea?
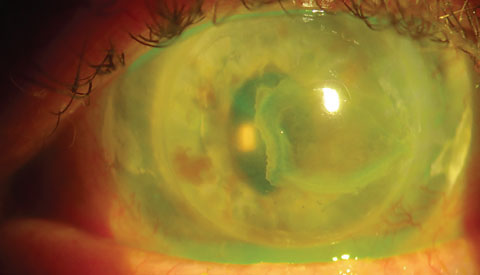
Disease Entity. Cornea verticillata (also called vortex keratopathy, whorl keratopathy, or Fleischer vortex) describes a whorl-like pattern of golden brown or gray opacities in the cornea. It is termed cornea verticillata from the Latin noun “verticillus,” meaning “whorl”.
What are the differences between Fabry disease and slitlamp microscopy?
Occasionally, slight differences on slit-lamp microscopy can be seen in the opacities due to medications compared to those seen in Fabry disease. Drug-related opacities may appear as horizontal lines with fine branching at the extrem ities, while Fabry disease-related opacities may appear as curving lines that form whorls before becoming almost straight at the periphery.
What are the properties of cornea verticillata?
The medications that produce cornea verticillata share cationic, amphiphilic properties that allow them to penetrate lysosomes in the basal epithelial layer of the cornea, where they bind to cellular lipids. These medication-lipid complexes are resistant to enzymatic degradation and accumulate as deposits in the cornea.
Can cornea verticillata cause eye pain?
Patients with cornea verticillata typically have no visual complaints or eye discomfort. Rarely, patients may see blue-green rings in their vision or halos around lights.
Is there a treatment for cornea verticillata?
Management and Follow-up. There is no recommended treatment for cornea verticillata. The deposits are typically not visually significant, and typically resolve with cessation of the responsible agent. No alteration in medication regimen or further work-up is required for an isolated finding of cornea verticillata.
What is the term for a corneal keratopathy?
This cornea has a subtle finding of linear deposits on the surface epithelium. This is called whorl keratopathy (also known as hurricane keratopathy or verticillata) and occurs secondary to several medications. This finding is usually subtle, and doesn’t seem to cause any visual symptoms.
Does hurricane keratophathy cause visual symptoms?
This finding is usually subtle, and doesn’t seem to cause any visual symptoms. This photograph shows an eye suffering from hurricane keratophathy. This occurs as a result of several medications (such as amiodarone) that deposit in the corneal surface.
Does corneal verticillata cause vision loss?
So, while corneal verticillata appears to be a common side effect of this drug, it also appears to cause no degradation in vision and resolves with discontinuation. About 17% of subjects in Rocket 1 and 2 also showed mild subconjunctival hemorrhages, which can be striking in appearance and can cause concern in uninformed patients.
Can Rhopressa cause verticillata?
When prescribing Rhopressa for your open-angle glaucoma and ocular hypertension patients, keep in mind that a significant amount of them may experience mild, transient conjunctival hyperemia, and almost one quarter of patients may manifest corneal verticillata.
Introduction
Drug-induced corneal complications can be categorized by histological layer:
Pathogenesis
Systemically-administered drugs reach the cornea via the tear film, aqueous humor, and limbal vasculature. Pathology is caused by deposition or direct cytotoxicity. Manifestation of corneal disease may foreshadow that of retinal disease. [1]
Stromal
Corneal stromal deposition can occur via the aqueous humor, limbal vasculature, and tear film. Deposits may be pigmented, refractile, or crystalline. [1]
How to Monitor These Side Effects
If you are prescribed and taking a medication that has severe eye side effects, you should have an annual eye exam with your eye doctor to monitor your eye health.
Medications with Major Eye Side Effects
Some medications that have major eye side effects are amlodipine, hydroxychloroquine, topiramate, tamoxifen, and ethambutol.
Eye Problems Caused by Amlodipine
Amlodipine is a heart medication that is prescribed frequently for arrythmia treatment.
Eye Problems Caused by Hydroxychloroquine
Hydroxychloroquine is an anti-inflammatory drug often prescribed for autoimmune conditions like rheumatoid arthritis or lupus.
Eye Problems Caused by Topiramate
Topiramate is an anti-seizure medication that is also used in treatment of migraines.
Eye Problems Caused by Tamoxifen
Tamoxifen is a medication that inhibits estrogen and is used to treat some forms of breast cancer.
Importance of Disclosing Medications
These medications are just a few of thousands of medications which have been shown to have eye side effects.
What is Cornea verticillata associated with?
Cornea verticillata is most commonly associated with amiodarone and Fabry disease.
How to identify drug-induced cornea verticillata?
The etiology of drug-induced forms of cornea verticillata can typically be identified with a thorough review of the patient’s medical history and medications. If attempting to differentiate between drug-induced cornea verticillata and that caused by Fabry disease, the microstructure of the deposits can be viewed with confocal laser scanning microscopy. However, this is not a routine part of the diagnostic evaluation.
What is the name of the disease that causes brown opacities in the cornea?
Disease Entity. Cornea verticillata (also called vortex keratopathy, whorl keratopathy, or Fleischer vortex) describes a whorl-like pattern of golden brown or gray opacities in the cornea. It is termed cornea verticillata from the Latin noun “verticillus,” meaning “whorl”.
What are the differences between Fabry disease and slitlamp microscopy?
Occasionally, slight differences on slit-lamp microscopy can be seen in the opacities due to medications compared to those seen in Fabry disease. Drug-related opacities may appear as horizontal lines with fine branching at the extrem ities, while Fabry disease-related opacities may appear as curving lines that form whorls before becoming almost straight at the periphery.
What are the properties of cornea verticillata?
The medications that produce cornea verticillata share cationic, amphiphilic properties that allow them to penetrate lysosomes in the basal epithelial layer of the cornea, where they bind to cellular lipids. These medication-lipid complexes are resistant to enzymatic degradation and accumulate as deposits in the cornea.
Can cornea verticillata cause eye pain?
Patients with cornea verticillata typically have no visual complaints or eye discomfort. Rarely, patients may see blue-green rings in their vision or halos around lights.
Is there a treatment for cornea verticillata?
Management and Follow-up. There is no recommended treatment for cornea verticillata. The deposits are typically not visually significant, and typically resolve with cessation of the responsible agent. No alteration in medication regimen or further work-up is required for an isolated finding of cornea verticillata.
General Information
Causes
- There is a clear connection between the etiology of keratopathy and its clinical form. The most common cause of the threadlike form of the disease is dry eye syndrome, often combined with autoimmune pathology (Sjogren’s syndrome). Keratoconjunctivitis, recurrent corneal erosion, the imposition of mono- or binocular dressing in the postoperative per...
Symptoms
- From a clinical point of view, there are threadlike, exposure, neurotrophic, ribbon-like, aphakic, pseudoaphakic, cordaronic, lipoid, thermal, ultraviolet forms and surface point keratopathy of Tigeson. Common symptoms for all variants are hyperemia of the eyes, foreign body sensation, photophobia and pain in the eyes of varying intensity. A specific sign is corneal opacity, which p…
Diagnosis
- The main methods of diagnosis of keratopathy are external eye examination and biomicroscopy using a slit lamp. Additionally, visometry, ophthalmoscopy and tonometry are performed. External examination with filamentous keratopathy allows you to identify short formations consisting of epithelial cells and mucus. These structures resemble threads that are attached to the anterior s…
Treatment
- In all forms of keratopathy, therapeutic measures should begin with etiotropic therapy of the underlying disease. Pathogenetic treatment is reduced to moisturizing the cornea (in the absence of defects) with artificial tear preparations and moisturizing ointments. With filamentous keratopathy, removal of pathological formations under regional anesthesia is indicated. With a ri…
Prognosis and Prevention
- Specific measures for the prevention of keratopathy have not been developed. Patients are advised to monitor eye hygiene. With prolonged visual load, special means should be used to moisturize the cornea, do gymnastics and short breaks. Patients with a genetic predisposition or when taking Cordarone for 6 months need to be examined by an ophthalmologist 2 times a year…
Etiology
- Cornea verticillata is most associated with amiodarone and Fabry disease. It can also be caused by a variety of other medications, the most common of which include: 1. Chloroquine and Hydroxychloroquine 2. Indomethacin 3. Phenothiazines Other agents implicated in cornea verticillata include gentamicin, tamoxifen, meperidine, chlorpromazine, atovaquone, suramin, tilo…
Pathophysiology
- The whorl-like pattern of cornea verticillata results from the centripetal migration of deposit-laden limbal stem cells as the corneal epithelium undergoes natural growth and repair. The medications that produce cornea verticillata share cationic, amphiphilic properties that allow them to penetrate lysosomes in the basal epithelial layer of the cor...
Symptoms
- Patients with cornea verticillata typically have no visual complaints or eye discomfort. Rarely, patients may see blue-green rings in their vision or halos around lights.
Signs
- Corneal verticillata is recognizable as fine golden-brown or gray opacities in the basal epithelium that branch out from a central whorl, usually across the inferior cornea. The deposits do not stain and are almost always bilateral. Occasionally, slight differences on slit-lamp microscopy can be seen in the opacities due to medications compared to those seen in Fabry disease. Drug-related …
Management and Follow-Up
- There is no recommended treatment for cornea verticillata. The deposits are typically not visually significant, and typically resolve with cessation of the responsible agent. No alteration in medication regimen or further work-up is required for an isolated finding of cornea verticillata.Several case reports have described the resolution of cornea verticillata with the use …