
What do chondrocytes do?
So what, exactly, do chondrocytes do? Since chondrocytes are the only cells located in cartilage, they produce and maintain the cartilage matrix. So what is a cartilage matrix?
What is the distribution of chondrocytes in cartilage?
In the middle zone, chondrocytes are larger and more rounded and display a random distribution, in which the collagen fibers also are more randomly arranged. In the deeper zones, chondrocytes form columns that are oriented perpendicular to the cartilage surface, along with the collagen fibers.
What factors affect the number of chondrocyte cells created?
The number of chondrocyte cells created and their maturation process can be influenced by multiple different genes and proteins. Two proteins, bone morphogenetic protein 4 (BMP-4) and fibroblast growth factor 2 (FGF2) have been seen to influence the amount of differentiation into chondrocytes.
What organelles are present in chondrocytes?
Chondrocytes’ size and shape vary depending on the anatomical layer, but all of them has organelles like endoplasmic retinaculum and Golgi membrane for matrix synthesis. Cytoskeleton of chondrocytes is composed of actin, tubulin and vimentin filaments.
What type of cells do chondrocytes produce?
Chondrocytes are metabolically active cells that synthesize and turnover a large volume of extra cellular matrix (ECM) components such as collagen, glycoproteins, proteoglycans, and hyaluronan [2].
Do chondrocytes make cartilage?
Chondrocytes are the cells responsible for cartilage formation, and they are crucial for the process of endochondral ossification, which is useful for bone development. Also, by mimicking skeletal development chondrocytes play a critical role in fracture repair.
What are chondrocytes responsible for?
Chondrocytes are responsible for the synthesis of the two major constituents of the matrix, collagen and proteoglycan, as well as enzymes that degrade matrix components (collagenase, neutral proteinases, and cathepsins).
Do chondrocytes produce fibers?
The cells, called chondrocytes, make the matrix and fibers of the tissue.
Do chondrocytes make bone?
For decades, it has been widely accepted that hypertrophic chondrocytes undergo apoptosis prior to endochondral bone formation. However, very recent studies in long bone suggest that chondrocytes can directly transform into bone cells.
What is inside a chondrocyte?
Chondrocytes (/ˈkɒndrəsaɪt, -droʊ-/, from Greek χόνδρος, chondros = cartilage + κύτος, kytos = cell) are the only cells found in healthy cartilage. They produce and maintain the cartilaginous matrix, which consists mainly of collagen and proteoglycans.
Do chondrocytes produce synovial fluid?
The fluid contains hyaluronan secreted by fibroblast-like cells in the synovial membrane, lubricin (proteoglycan 4; PRG4) secreted by the surface chondrocytes of the articular cartilage and interstitial fluid filtered from the blood plasma.
What produces cartilage?
Cartilage is formed from the mesoderm germ layer by the process known as chondrogenesis. [5] Mesenchyme differentiates into chondroblasts, which are the cells that secrete the major components of the extracellular matrix—the most important of these components for cartilage formation being aggrecan and type II collagen.
What is the main function of chondroblasts?
Chondroblasts, located in the perichondrium, are cells that play an important role in the development of cartilage. By producing extracellular matrix, chondroblasts create the main component that provides structure and strength to cartilage.
What is the role of chondroblasts?
Chondroblasts Function Chondroblast cells function to carry out the development, maintenance, growth, and homeostasis of the cartilage tissue. Their functions are as follows: Development of cartilage: The primary function of the chondroblast is the development of the cartilage.
How are chondrocytes formed?
Chondrocytes arise from cranial neural crest cells (CNCCs) of the neural ectoderm, cephalic mesoderm, sclerotome of the paraxial mesoderm, or somato-pleure of the lateral plate mesoderm. Terminal differentiation of chondrocytes results in different types of cartilage: hyaline; elastic; and fibrous.
Which cell produces collagen fibers and ground substance?
FibroblastsFibroblasts are the most common cell type of connective tissue. They produce both fibers and amorphous ground substance.
What is the difference between a chondrocyte and an Osteocyte?
Chondrocytes vs Osteocytes Osteocytes are a type of bone cells present in mature bone tissues. Osteocytes are involved in the maintenance of bone tissue. Chondrocytes are involved in the maintenance of cartilage.
Are fibers present in cartilage?
Fibers: Cartilage is composed of collagen and elastic fibers. In hyaline cartilage, type II collagen makes up 40% of its dry weight. Elastic cartilage also contains elastic fibers, and fibrocartilage contains more collagen than hyaline cartilage.
How do chondrocytes become osteoblasts?
We show that hypertrophic chondrocytes can survive the cartilage-to-bone transition and become osteoblasts and osteocytes during endochondral bone formation and in bone repair.
Where do chondrocytes divide?
In growing cartilage, the chondrocytes can divide, and the daughter cells remain close together in groups, forming a 'nest' of 2-4 cells. The matrix enclosed compartments that they sit in are called lacunae.
What happens to chondrocytes after they proliferate?
During this process, a cartilage template is formed in which chondrocytes proliferate and differentiate into hypertrophic chondrocytes and are gradually replaced by bone. Postnatally, remnants of embryonic chondrocytes remain in a restricted domain between the ossified regions of the bones forming the growth plate.
How do chondrocytes get nutrients?
Since there is no direct blood supply, chondrocytes receive nourishment via diffusion from the surrounding environment. The compressive forces that regularly act on cartilage also increase the diffusion of nutrients.
What is the definition of chondrocytes?
(KON-droh-site) Cartilage cell. Chondrocytes make the structural components of cartilage.
How are nutrients supplied to chondrocytes?
nutrient acquisition Cartilage cells, called chondrocytes, occur at scattered sites through the cartilage and receive nutrition by diffusion through the gel; cartilage contains no blood vessels or nerves, unlike bone.
What is the difference between a chondrocyte and an Osteocyte?
Chondrocytes vs Osteocytes Osteocytes are a type of bone cells present in mature bone tissues. Osteocytes are involved in the maintenance of bone tissue. Chondrocytes are involved in the maintenance of cartilage.
What do chondrocytes do in hyaline cartilage?
Chondrocytes are mainly responsible for the production of collagen and the extracellular matrix that will lead to the maintenance of cartilaginous tissues within joints.
What do chondrocytes do in articular cartilage?
Chondrocytes are responsible for the development, maintenance, and repair of the ECM via a group of degradative enzymes. Chondrocytes synthesize matrix components, including proteins and glycosaminoglycan side chains.
How are chondrocytes formed?
Chondrocytes arise from cranial neural crest cells (CNCCs) of the neural ectoderm, cephalic mesoderm, sclerotome of the paraxial mesoderm, or somato-pleure of the lateral plate mesoderm. Terminal differentiation of chondrocytes results in different types of cartilage: hyaline; elastic; and fibrous.
Which proteoglycans are present in the chondrocyte?
The two main proteoglycans that are used in this process are heparan sulfate proteoglycans (HSPGs) and chondroitin sulfate proteoglycans (CSPGs) which are present at high levels in the chondrocyte extracellular matrix and are crucial in regulating chondrocyte maturation.
Why is chondrocyte maturation so tightly regulated?
Few deviations, misregulations, and mutations are found in organisms because they are often detrimental or lethal to the organism. This is why chondrocyte maturation is so tightly regulated.
What is cartilage matrix structure?
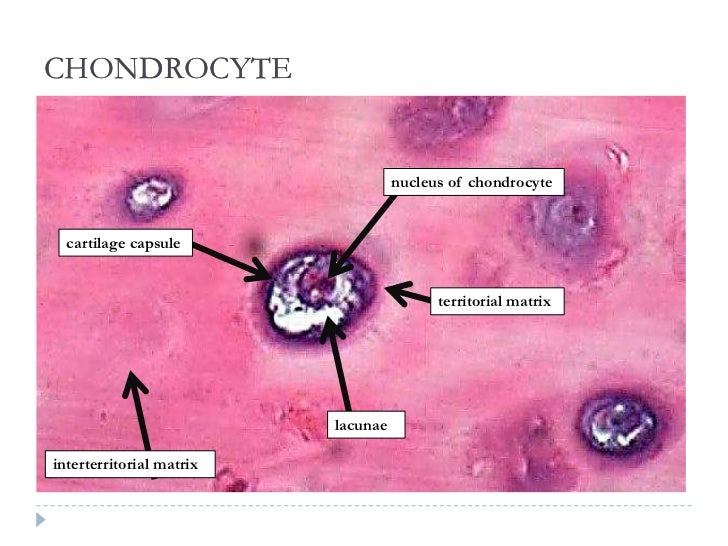
Structure. The chondrocyte in cartilage matrix has rounded or polygonal structure. The exception occurs at tissue boundaries, for example the articular surfaces of joints, in which chondrocytes may be flattened or discoid. Intra-cellular features are characteristic of a synthetically active cell.
How do vertebrate skeletal structures form?
Endochondral ossification is the process by which most vertebrate axial skeletons form into hardened bones from cartilage. This process begins with a cartilage anlage where chondrocyte cells will congregate and start their maturation process. Once the chondrocytes have fully matured at the desired rate, the cartilage tissue will harden into bone. This process is similar across most vertebrates and is closely regulated due to the large importance of the skeleton in survival. Few deviations, misregulations, and mutations are found in organisms because they are often detrimental or lethal to the organism. This is why chondrocyte maturation is so tightly regulated. If they mature too quickly or slowly there is a large possibility the organism will not survive gestation or infancy. One gene that is closely involved in skeletal formation is Xylt1. Normally, this gene is responsible for catalyzing the addition of glycosaminoglycan (GAG) side chains to proteoglycans, which are used during cell signaling to control processes such as cell growth, proliferation, and adhesion. The two main proteoglycans that are used in this process are heparan sulfate proteoglycans (HSPGs) and chondroitin sulfate proteoglycans (CSPGs) which are present at high levels in the chondrocyte extracellular matrix and are crucial in regulating chondrocyte maturation. When the GAG chain functions properly, it controls the maturation speed of chondrocytes and ensures enough cells gather in the cartilage anlage. Xylt1 is an essential gene in regards to chondrocytes and proper skeletal formation, and is a key factor in the close regulation of maturation. However, the mutation pug of the Xylt1 gene was studied in mice in 2014 and was found to cause the pre-maturation of chondrocytes. Animals with homozygous pug alleles display dwarfism and have considerably shorter bones compared to wild-type animals. These organisms show a reduction of typical Xylt1 gene activity, as well as a reduction in GAG chain levels. This mutation causes fewer GAG chains to be added to HSPGs and CSPGs, meaning there are fewer complexes available to closely regulate the maturation of chondrocytes. Incorrect signals are sent to chondrocytes in the cartilage anlage because the GAG chain and proteoglycan complexes are unable to work properly and cause the chondrocytes to mature and ossify too quickly. The correct amount of chondrocytes are not able to gather in the cartilage anlage, leading to a shortage of cartilage for ossification and eventually shorter bones.
What is the effect of Vitamin A on chondrocytes?
Cell culture studies of excess Vitamin A inhibits the synthesis of chondroitin sulfate by chondrocytes and causes the inhibition of chondrogenesis in the developing embryo which may result in limb malformations.
What are mesenchymal stem cells?
Mesenchymal ( mesoderm origin) stem cells are undifferentiated, meaning they can differentiate into a variety of generative cells commonly known as osteochondrogenic (or osteogenic, chondrogenic, osteoprogenitor, etc.) cells. When referring to bone, or in this case cartilage, the originally undifferentiated mesenchymal stem cells lose their pluripotency, proliferate and crowd together in a dense aggregate of chondrogenic cells (cartilage) at the location of chondrification. These chondrogenic cells differentiate into so-called chondroblasts, which then synthesize the cartilage extracellular matrix (ECM), consisting of a ground substance (proteoglycans, glycosaminoglycans for low osmotic potential) and fibers. The chondroblast is now a mature chondrocyte that is usually inactive but can still secrete and degrade the matrix, depending on conditions.
What is the only cell in cartilage?
FMA. 66782. Anatomical terms of microanatomy. Chondrocytes ( / ˈkɒndrəsaɪt, - droʊ -/, from Greek χόνδρος, chondros = cartilage + κύτος, kytos = cell) are the only cells found in healthy cartilage. They produce and maintain the cartilaginous matrix, which consists mainly of collagen and proteoglycans.
What is a chondrocyte?
Here we will learn about chondrocytes meaning. Chondrocytes are the cells that are solely responsible for producing cartilaginous cells and matrix. Not just producing but they help in maintaining them too. An immature chondrocyte is known as a chondroblast. The cartilaginous matrix is comprised mainly of collagen and proteoglycan. Now here a question arises that where are chondrocytes found. The chondrocytes location is in the cartilage connective tissue. Apart from them, no other cells are located here. They are found in the cartilage matrix which is a kind of lake for them where they swim.
What are the features of chondrocytes?
Intracellular spacing is present in synthetically active cells. The adult chondrocytes exhibit various amazing features. When they get flattened, they get themselves aligned parallelly to the collagen fibers in the superficial zones. When present in the intermediate zone, they appear more round and larger in size which helps them in exhibiting a bottom type of distribution where the fibers are oriented in a random pattern. Due to their position, these chondrocytes behave differently in different layers. When they are present in the inner zone they form columns and are aligned 90 degrees to the surface of the cartilage. For the spatial organization of the cells, the primary cilia are important. These primary cilia are also sensory organelles in chondrocytes.
Which cells are responsible for maintaining cartilage and their matrix in our body?
From the above passage we can conclude that chondrocytes are the cells that are responsible for maintaining the cartilages and their matrix in our body. Cartilage is important for bones because it helps in providing cushioning to the bones and by sticking on their ends they protect the bones from wearing and tearing.
Where are articular cartilages located?
Answer: They are located in intervertebral discs in the form of articular cartilage. They produce and maintain cartilage matrix. They help in maintaining homeostasis in the articular cartilage joints. They also help in repairing cartilages.
Where do cells come from?
But, have you ever wondered where do these cells come from? Cells arise from pre-existing cells so there are different cells that are specialized in our body to form and maintain certain types of cells.
What is Perichondrium?
Perichondium is just a layer of dense irregular connective tissue. The cartilage of developing bone is surrounded by this perichondrium. It is made up of two separate layers which are the outer fibrous layer and the inner chondrogenic layer. Collagen fibers are produced by fibroblast cells which are present in the fibrous layer. The perichondrium is also found around the connective cartilage and hyaline cartilage. It contains type 1 and types 12 collagen which helps in the function and growth of cartilage.
What are the two subgroups of chondrocytes?
To divide chondrocytes into two subgroups, nonhypertrophic (resting and proliferating) and hypertrophic, is helpful to understand their differentiation processes. Several growth factors have been demonstrated to control nonhypertrophic chondrocyte differentiation in vivo.
How do chondrocytes respond to mechanical stimuli?
Chondrocytes can sense and respond to mechanical stimuli via several regulatory pathways (e.g., upstream signaling, transcription, translation, post-translational modification, vesicular transport).234 Chondrocytes can remodel extracellular matrix in response to alterations in functional demand, as physical forces influence the synthesis, assembly, and degradation of the extracellular cartilage matrix. High magnitude or duration loads can also cause chondrocyte death and collagen damage, and chondrocytes in the superficial zone appear to be more vulnerable to load-induced injury than those in the middle and deep zones.235,236 Normal stimuli help chondrocytes maintain the extracellular matrix; abnormal stimuli can disrupt this balance.
What are the two subpopulations of hypertrophic chondrocytes?
The hypertrophic chondrocytes comprise two subpopulations: the prehypertrophic chondrocytes and the fully differentiated hypertrophic chondrocytes. Parathyroid hormone (PTH)–related peptide (PTHrP) binds to the PTH/PTHrP receptor present in prehypertrophic chondrocytes, and it plays a critical role in regulating hypertrophic chondrocyte differentiation. PTHrP expression is under the control of Ihh; Ihh upregulates the synthesis of PTHrP by prehypertrophic chondrocytes, thereby indirectly slowing down the process of chondrocyte hypertrophy. 15 Wnt signaling also plays an important role in the regulation of hypertrophic chondrocyte biology. Studies have shown that misexpression of Wnt-4 accelerates the nonhypertrophic to hypertrophic transition and results in slightly advanced ossification, whereas misexpression of Wnt-5a causes a delay in the transition from prehypertrophic to hypertrophic chondrocyte and results in a mild delay in ossification. 22 Core-binding factor-α subunit 1 (CBFA1), a member of the runt family of transcription factors, is expressed in prehypertrophic chondrocytes, and its constitutive expression in nonhypertrophic chondrocytes induces hypertrophic chondrocyte differentiation, Ihh expression, and, eventually, endochondral bone formation. 23 These functions, along with its role during osteoblast differentiation and vascular invasion, identify CBFA1 as the most pleiotropic regulator of skeletogenesis.
What are the cellular components of cartilage?
Chondrocytes are the sole cellular constituents of cartilage. Their terminal differentiation determines the character of the cartilage (hyaline, fibrous, or elastic). This complex process has been recently reviewed. 22 Chondrocytes in articular cartilage persist and do not ordinarily divide after skeletal maturity is attained. 23 Those in the epiphyseal growth plate differentiate to facilitate endochondral ossification, after which they may undergo apoptosis or become osteoblasts. 23 Chondrocytes are responsible for the synthesis of the two major constituents of the matrix, collagen and proteoglycan, as well as enzymes that degrade matrix components (collagenase, neutral proteinases, and cathepsins). 23 This dual function places the chondrocyte in the role of regulating cartilage synthesis and degradation. Immediately surrounding the chondrocyte is the pericellular region, which contains type VI collagen and the proteoglycans decorin and aggrecan. 16 Chondrocytes in zone 1 produce superficial zone protein (lubricin) which is important in maintaining relatively frictionless joint motion. Synthesis of this protein is defective in the camptodactyl-arthropathy-coxa vara-pericarditis syndrome 24 (see Chapter 40 ).
How are chondrocyte integrins regulated?
The expression of chondrocyte β1 integrins is regulated by mechanical forces. Tension forces stimulate their expression with a mechanism that appears to be mediated by FAK, and this effect leads to inhibition of chondrogenesis, especially through α2β1 and α5β1 receptors (Takahashi et al., 2003; Onodera et al., 2005 ).
How does chondrocyte function change with age?
Chondrocyte function, including mitotic and synthetic activity, deteriorates with age. Degradative changes are generally due to the actions of proteinases and are, at least in part, the cumulative consequences of adverse conditions, such as mechanical insults or inflammation, to which the chondrocyte is exposed throughout life. Deficiencies in cartilage matrix proteins also may disrupt chondrocyte-matrix interactions that are important to cell survival. The decline in chondrocyte number may be attributed to increased cell death with age. Although programmed cell death, or apoptosis, increases with age in adult rats and mice, this may be due to skeletal growth that occurs throughout life in these animals. In human adult cartilage, apoptotic cell removal does not seem to be common, however.39 Replicative senescence, detected as β-galactosidase activity and decreased telomere length, has been proposed to contribute to age-related changes in the proliferative potential of adult articular chondrocytes.431,432
Why do chondrocytes decrease with age?
Although programmed cell death, or apoptosis, increases with age in adult rats and mice, this may be due to skeletal growth that occurs throughout life in these animals.
What Are Chondrocytes?
Chondrocytes are the cells making up the cartilage. They are pivotal to synthesize cartilage matrix and sustain the extracellular matrix. It primarily comprises the proteoglycans and collagen. Chondrocytes are surrounded by the collagenous fibres and secrete substances causing the cartilage to acquire strength and flexibility.
Where are chondrocytes found in cartilage?
They are found sitting in lacunae which are matrices enclosing the compartments.
What is the surface of cartilage encircling the layer of dense irregular connective tissue?
Its perichondrium is the surface of the cartilage encircling the layer of dense irregular connective tissue.
What is the 5th week of cartilage development?
In the fifth week of development, the initial cartilage comprises the mesenchyme which is crucial in activating the regions of chondral development. Additionally, it also condenses to make chondrification centres. Prechondrocytes are developed from mesenchymal cells that are the future chondroblasts.
What are the cells that maintain cartilage?
Chondrocytes are cells producing and maintaining the cartilage matrix. They are vital in sustaining homeostasis in the AC joints rendering cushioning in the joint movements. Chondrocytes drift apart from each other by the cartilage matrix. These cells take charge of chondral repair.
What are prechondrocytes made of?
Prechondrocytes are developed from mesenchymal cells that are the future chondroblasts. These structures in turn release extracellular matrix and collagenous fibrils. As a result, the elastic and collagenous fibres are accumulated in the intercellular matrix. The matrix hence formed conduces cartilaginous typecast.
Why do chondrocytes behave differently in different layers?
Chondrocytes behave differently in different layers due to their position. The zonal differences in synthetic attributes can remain in the primary chondrocyte cultures. The primary cilia are important for spatial organization of cells in the developing growth plate which are sensory organelles in chondrocytes.
How are chondrocytes isolated?
Chondrocyte isolation requires the services of a laboratory equipped for cell culture. Allograft chondrocytes are harvested from foals destroyed for noninfectious disease, most frequently irreparable fractures or severe congenital deformities. Cartilage slices are harvested aseptically from the stifle, shoulder, or elbow, and the cells isolated from their matrix by overnight collagenase digestion ( Nixon et al, 1992 ). The cells are then counted, and dimethyl sulfoxide (DMSO) is added to the culture medium prior to freezing and storage in liquid nitrogen. When the cells are required, 48 hours’ lead time is necessary to thaw the cells and then briefly culture to allow removal of any dead cells, before collection for use in surgery.
What is the role of chondrocytes in bone development?
Chondrocyte apoptosis plays a major role in the shaping of long bones during development. In the growth plate, chondrocytes undergo a series of highly regulated transformations leading to the replacement of the cartilage template by bone. During this process, known as endochondral ossification, chondrocytes proliferate, produce type II collagen, and form a columnar cell layer. Subsequently they undergo cell cycle arrest, differentiation, and hypertrophy, which is followed by mineralization of the surrounding matrix. At this point, the chondrocytes die by apoptosis and, after blood vessel invasion, the cartilage is replaced with bone (Gibson et al., 1995 ).
What causes uneven chondrocyte proliferation?
Uneven chondrocyte proliferation with subsequent increased joint space occurs early in response to increased GH and IGF-I levels. Ulcerations and fissures on the weight-bearing areas of new cartilage are often accompanied by new bone formation. This process eventually results in debilitating osteoarthritis associated with bone remodeling, osteophyte formation, subchondral cysts, narrowed joint spaces and lax periarticular ligaments. Osteophytes are seen at the tufts of the phalanges and over the anterior aspects of spinal vertebrae. Ossification of ligaments and periarticular calcium pyrophosphate deposition are also found [134]. The duration of hypersomatotrophism appears to directly correlate with the severity of the joint changes [143], and responses to therapy (see below) will usually depend upon the degree of irreversible cartilage degeneration already in place.
What is the role of chondrocytes in endochondral ossification?
In the growth plate, chondrocytes undergo a series of highly regulated transformations leading to the replacement of the cartilage template by bone.
What is chondrocyte alginate gel?
Chondrocyte–alginate gel suspensions have been investigated as a possible injectable material for endoscopic therapies to treat urinary incontinence and vesicoureteral reflux. The gelling properties of alginate combined with the low nutrient requirements of chondrocytes may facilitate the formation of a stable bulking material. Chondrocytes mixed with alginate gel were injected subcutaneously into athymic mice. The injected suspensions formed cartilaginous tissues in vivo and showed no evidence of cartilage or alginate migration, granuloma formation, or volume loss. Additional studies demonstrated that vesicoureteral reflux could be treated with an autologous chondrocyte–alginate suspension without any evidence of obstruction in a mini-pig model. Phase II clinical trials using this substance in humans are currently underway for both vesicoureteral reflux and urinary incontinence.
What are chondrocyte sheets?
Chondrocyte sheets applicable to cartilage regeneration were prepared with cell-sheet technique using temperature-responsive culture dishes. The layered chondrocyte sheets were able to maintain the phenotype of cartilage, and could be attached to the sites of cartilage damage. The cell sheets acted as a barrier to prevent a loss of proteoglycan from these sites and to protect them from catabolic factors in the joint [54]. Chondrocyte sheets with a consistent cartilaginous phenotype and adhesive properties were confirmed and it may lead to a new strategy for cartilage regeneration [55,56] ( Figure 5.6 ).
Why is chondrocyte culture important?
Chondrocyte culture is an efficient target system for evaluation of the pharmacological and toxicological effects of drugs acting on cartilaginous tissue. Many types of culture exist and have their own advantages and drawbacks. For example, in monolayer culture chondrocytes do not retain all of their specific functions. Cartilage slices and three-dimensional culture maintain chondrocytes in a differentiated state but without noticeable cell division. Therefore, it is necessary to choose the type of culture relevant to the pharmacological and toxicological end-point being considered.
What are the functions of chondrocytes?
The main function of chondrocytes in the superficial and mid zone is to synthesize ECM composed of collagen type II, IX, and XI and proteoglycans. This ECM facilitates compressional and tensile forces across the diarthrodial joint [9,10]. Collagens are the most abundant macromolecules of the ECM, make up 60% of the dry weight of the cartilage, and provide tensile and shear strength to the tissue. Collagen also stabilizes the matrix. Collagen type II makes up 90%–95% of the collagen in ECM and forms fibrils and fibers interwoven with proteoglycan like aggrecans [10]. Collagens type IX and XI represent 5%–10% of the AC collagenous network and offer support for the collagen fibrilar crosslinking. Chondrocytes of the deep zone are terminally differentiated and actively synthesize collagen type X. Proteoglycans represent the second largest group of macromolecules and are heavily glycosylated protein monomers that resist compressional forces by swelling pressure due to their affinity to water across the articular joint [9]. These proteoglycans include aggrecan, decorin, biglycan, and fibromodulin. Aggrecans are the largest among the group [9,11]. Growth factors play a crucial role in controlling chondrogenesis by affecting MSCs differentiation to chondrocytes. They also influence chondrocytes to synthesize specific ECM proteins (Figure 1). The shift in expression of collagen type X by the chondrocytes also marks the regulation of proteolytic enzymes production. These enzymes aid in the clearing of the cartilage ECM and allow vascularization and calcification of tissue [10,12].
What is the role of chondrocytes in the maintenance of cartilage?
The majority of its structure and function is controlled by chondrocytes that regulate Extracellular Matrix (ECM) turnover and maintain tissue homeostasis. Imbalance in their function leads to degenerative diseases like Osteoarthritis (OA). OA is characterized by cartilage degradation, osteophyte formation and stiffening of joints. Cartilage degeneration is a consequence of chondrocyte hypertrophy along with the expression of proteolytic enzymes. Matrix Metalloproteinases (MMPs) and A Disintegrin and Metalloproteinase with Thrombospondin Motifs (ADAMTS) are an example of these enzymes that degrade the ECM. Signaling cascades involved in limb patterning and cartilage repair play a role in OA progression. However, the regulation of these remains to be elucidated. Further the role of stem cells and mature chondrocytes in OA progression is unclear. The progress in cell based therapies that utilize Mesenchymal Stem Cell (MSC) infusion for cartilage repair may lead to new therapeutics in the long term. However, many questions are unanswered such as the efficacy of MSCs usage in therapy. This review focuses on the role of chondrocytes in cartilage formation and the progression of OA. Moreover, it summarizes possible alternative therapeutic approaches using MSC infusion for cartilage restoration.
What is the most common type of cartilage degenerative disease?
OA is the most prevalent type of cartilage degenerative disease, the other being rheumatoid arthritis. OA results in progressive cartilage degradation characterized by the softening, fibrillation and erosions of the articular surface [20]. Breakdown of proteoglycans leads to a reduction in the compressive stiffness of the tissue that accelerates the rate of collagen loss [21]. In OA , besides cartilage erosion in subchondral bone, synovial fluid, and the synovial membrane also play a role in the progression of OA. Osteophyte formations, subchondral bone remodeling, and synovial membrane inflammation may further aid in cartilage tissue degradation. In early stages of OA , hypertrophic chondrocytes express collagen type X. This production marks the terminal differentiation of chondrocytes that regulates the expression of proteolytic enzymes like MMPs, and ADAMTS that degrade the proteoglycan and collagen network. Simultaneously, activation of transcriptional regulators such as Runt-Related Transcription Factor 2 (RUNX2) are known to induce terminal differentiation and enhance the expression of collagen type X and proteolytic enzymes that digest the AC ECM [22–24]. MMP-1 (Collagenase-1) and MMP-13 (Collagenase-3) are the primary factors that lead to overall degradation of collagenous framework. MMP-3 (Stromelysin-1) and ADAMTS-4 (aggrecanase-1) degrade proteoglycans [25,26]. It is shown that MMP activities are controlled by physiologic activators such as cathepsin B and tissue inhibitors of MMPs (TIMPs) [27]. An imbalance between these factors is commonly seen in OA tissue. Repeated mechanical insult to AC enhances MMP production and enhances cartilage matrix breakdown, [28,29]. These deleterious effects are pronounced in the superficial region of AC [30]. However, the process that regulates the production of proteolytic enzymes still remains unclear [30].
How does BMP affect chondrogenesis?
The effect of BMPs on chondrogenesis was demonstrated. BMPs function promote differentiation, proliferation, and maturation throughout the chondrocytes lineage [60]. While BMP7 enhanced chondrogenic activity, BMP2 also induces chondrocyte hypertrophy. This is remarkable since both factors signal through the same receptors. The BMP canonical Smad 1/5/8 pathway is a potent inducer of chondrocyte hypertrophy and endochondral ossification [61]. Therefore, other pathways within BMP signaling may be responsible for the diversity of effects. During OA, BMP2 mRNA levels are upregulated and followed by terminal differentiation of chondrocytes [62]. The terminal differentiation of chondrocytes enhances the secretion of collagen type X and MMP-13. During progression of OA, several chondrocytes within the cartilage tissue express BMPs. Enhanced BMP production may influence the MSCs present in the OA cartilage. BMPs may potentiate chondrogenic differentiation but may also initiate aberrant osteophyte formation as well as enhance proteolytic enzyme production for the acceleration of cartilage degradation [63]. Crosstalk between BMP, TGF-β and Wnt signaling pathways is known to regulate terminal differentiation of chondrocytes and the differential modulation between these signaling pathways could accelerate OA [64,65]. Wnt-16, Wnt-2B, and Wnt-induced signaling protein 1 (WISP-1) are expressed at high levels in OA, similar to the level of BMPs [66]. BMP2-induced Wnt/β-catenin signaling enhances the low-density-lipoprotein receptor-related protein 5 catabolic activity, followed by promoting hypertrophy in osteoarthritic chondrocytes.[57]. Wnt/β-catenin negatively regulate NF-κβ and drive TGF-β/BMP signaling. This leads to enhanced expression of RUNX2 that enhances the expression of MMP-13, MMP3, and collagen type X [53]. This process drives chondrocyte hypertrophy and accelerates OA induced cartilage damage. Figure 2summarizes the pathways involved in OA progression. How or what causes these imbalances in these signaling cascades is not known. Moreover, the regulation of the crosstalk between the factors is not completely understood.
What is the process of chondrogenesis?
During skeletal development chondrogenesis begins with mesenchymal cell recruitment, migration, and proliferation [58,67]. Condensation or aggregation of chondroprogenitor mesenchymal cells by cell–cell and cell–matrix interactions are associated with an increase in cell adhesion. This process can be measured by determining the levels of neural cadherin (N-cadherin), and neural cell adhesion molecule (N-CAM) [68]. Multiple growth factors, such as TGF-β, BMPs, FGFs, and Wnts, control the limb patterning for the development of AC of the epiphyseal plates and endochondral ossification of the metaphyseal plates [69].
What is the organization of normal articular cartilage?
Organization of normal articular cartilage. Superficial, middle, and deep zones and their extracellular matrix is divided using different sections. Growth factors that control the chondrocyte function are divided based on the stage of chondrocyte lineage.
What cytokines are involved in OA?
Inflammatory cytokines, such as IL-1β, TNF-α, and IL-6 , are known to be upregulated during OA progression [4]. These inflammatory cytokines are secreted by chondrocytes and synoviocytes. They play a role in the disruption of cartilage homeostasis, and MMP mediated cartilage degradation [4,31] modulating the chondrocyte metabolism by increasing MMP expression and inhibiting the production of MMP inhibitors [27]. IL-1β mediated TNF-α expression has been shown to regulate IL-6 production and nuclear factor-κβ (NF-κβ) dependent transcriptional expression of Hypoxia-inducible factor 2α (HIF-2α) drive the processes that may further enhance AC destruction [32–37]. OA induced cartilage damage follows a myriad of cascades that once activated result in an irreversible damage to the tissue. Chondrocytes recognize the loss of ECM and actively produce collagen type II and proteoglycans. However, the ratio between the ECM protein production to proteolytic enzyme production is imbalanced and results in complete loss of cartilaginous tissue overtime. Moreover, cellular attempts to repair the tissue results in aberrant osteoblast like differentiation forming osteophytes or fibroblastic differentiation inducing fibrosis or stiffening of the joints [38–40].
Which cells produce and maintain the extracellular matrix of cartilage?
Chondrocytes are specialised cells which produce and maintain the extracellular matrix of cartilage, a tissue that is resilient and pliant. In vivo, it has to withstand very high compressive loads, and that is explicable in terms of the physico-chemical properties of cartilage-specific macromolecules and with the movement ...
What is the architect of cartilage?
The chondrocyte, architect of cartilage. Biomechanics, structure, function and molecular biology of cartilage matrix macromolecules

Overview
Chondrocytes are the only cells found in healthy cartilage. They produce and maintain the cartilaginous matrix, which consists mainly of collagen and proteoglycans. Although the word chondroblast is commonly used to describe an immature chondrocyte, the term is imprecise, since the progenitor of chondrocytes (which are mesenchymal stem cells) can differentiate into vario…
Development
From least- to terminally-differentiated, the chondrocytic lineage is:
1. Colony-forming unit-fibroblast
2. Mesenchymal stem cell / marrow stromal cell
3. Chondrocyte
4. Hypertrophic chondrocyte
Structure
The chondrocyte in cartilage matrix has rounded or polygonal structure. The exception occurs at tissue boundaries, for example the articular surfaces of joints, in which chondrocytes may be flattened or discoid. Intra-cellular features are characteristic of a synthetically active cell. The cell density of full-thickness, human, adult, femoral condyle cartilage is maintained at 14.5 (±3.0) × 10 cells/ mm from age 20 to 30 years. Although chondrocyte senescence occurs with aging, mitoti…
Genetics
The number of chondrocyte cells created and their maturation process can be influenced by multiple different genes and proteins. Two proteins, bone morphogenetic protein 4(BMP-4) and fibroblast growth factor 2(FGF2) have been seen to influence the amount of differentiation into chondrocytes. Both proteins are known to play a role in embryonic stem cell differentiation into mesodermal cells, through signaling with BMP-4 and as FGF2 acting as a stimulator. From the m…
Gallery
• Chondrocytes in hyaline cartilage
• Transmission electron micrograph of a chondrocyte, stained for calcium, showing its nucleus (N) and mitochondria (M).
See also
• Chondronectin
• Endochondral ossification
• Intramembranous ossification
• List of human cell types derived from the germ layers
Further reading
• Dominici M, Hofmann TJ, Horwitz EM (2001). "Bone marrow mesenchymal cells: biological properties and clinical applications". Journal of Biological Regulators and Homeostatic Agents. 15 (1): 28–37. PMID 11388742.
• Bianco P, Riminucci M, Gronthos S, Robey PG (2001). "Bone marrow stromal stem cells: nature, biology, and potential applications". Stem Cells. 19 (3): 180–92. doi:10.1634/stemcells.19-3-180. PMID 11359943. S2CID 12197415.
External links
• Histology image: 03317loa – Histology Learning System at Boston University
• Stem cell information