Where are endothelial cells produced?
mesodermEndothelial cells originate from the mesoderm, a germinal layer that forms at gastrulation, an early embryonic development stage (Bautch and Caron, 2015).
Do endothelial cells produce cytokines?
Endothelial cells have been shown to produce various cytokines and chemokines during inflammatory processes and may be a source of cytokines and chemokines in the lung during influenza virus infection.
What cytokines do endothelial cells release?
We have shown that the release of soluble tie-1 from endothelial cells is regulated by proinflammatory cytokines, including TNFα, IL-1β, and LPS, and the angiogenic growth factor VEGF.
Do endothelial cells produce inflammatory mediators?
For vascular homeostasis, endothelial cells are of utmost importance and they produce a variety of mediators, surface proteins, and autocoids involved in vasomotion, coagulation, and inflammation [31].
How do cytokines cause vasodilation?
Cytokines could exert rapid vasoactive effects in blood vessels, likely by acting on the endothelial and smooth muscle receptors of the vessels.
Which cytokine increases stickiness of vascular endothelium?
Research in the last decade has shown that several cytokines, including tumour necrosis factor alpha (TNF alpha) and interleukin-1 beta (IL-1beta), potently increase the expression of many CAMs and thus increase the adhesiveness between leukocytes and the endothelium.
What are the endothelial cells?
The main type of cell found in the inside lining of blood vessels, lymph vessels, and the heart.
How does inflammation cause endothelial dysfunction?
Inflammation, as a feature of rheumatoid arthritis (RA), leads to the activation of endothelial cells (ECs). Activated ECs induce atherosclerosis through an increased expression of leukocyte adhesion molecules. Endothelial dysfunction (ED) is recognized as a failure of endothelial repair mechanisms.
What is the function of the endothelium?
The endothelium comprises the structure of the blood vessels and lymphatic vessels. It also allows for smooth vessel regulation, inflammation contr...
Why is endothelial function important?
The endothelium controls functions such as dilation and narrowing of blood vessels in order to help with blood pressure issues. It also secretes su...
What causes endothelial dysfunction?
Endothelial dysfunction is caused by many factors such as low oxygen, inflammation, infections, and cardiac conditions like high blood pressure.
What are four functions of endothelial cells?
The 4 main functions of endothelial cells are filtration of fluids, blood vessel size regulation, hemostasis, and transport of various substances t...
What causes damage to endothelial cells?
Many factors can damage endothelial cells such as cardiovascular diseases, infections, inflammation, plaque deposition from increased fat intake, a...
Where are your endothelial cells?
The endothelial cells are located in the lining of the cardiovascular system (arteries, veins, and capillaries) and in the vessels of the lymphatic...
What are the functions of endothelial cells?
The endothelial cells are involved in different tasks, which are performed either by all the endothelial cells in general or predominantly by endothelial cells in specific subsets of organs or vascular beds. For instance, endothelial cells in general regulate hemostasis.
What is the heterogeneity of endothelial cells?
The first hint of endothelial cell heterogeneity, a structural hetero geneity, was obtained following electron microscopy observations where differences in intercellular junctions led to the classification of continuous endothelium, fenestrated endothelium and discontinuous endothelium [92]. Continuous endothelium is found in most arteries, veins and capillaries of the brain, skin, lung, heart and muscle. Endothelial cells are coupled by tight junctions and anchored to a continuous basal membrane. Fenestrated endothelium is also associated with a continuous basal membrane and is characterized by the presence of transcellular 50–60 nm wide pores, which are sealed by a 5- to 6-nm-thick diaphragm. This is observed in tissues with an elevated trans-endothelial transport or an increased filtration role, such as endocrine and exocrine glands, gastrointestinal tract, choroid plexus, kidney glomeruli and subpopulations of renal tubules. The discontinuous endothelium is associated with a poorly structured basal membrane and is characterized by the presence of large 100- to 200-nm-wide fenestrations without diaphragm. This occurs in sinusoidal vascular beds in the liver, predominantly, but also in the spleen and bone marrow [20,1250].
What is the role of transcellular transport?
The transcellular transport involves membrane-attached and cytosolic caveolae that migrate across the capillary endothelial cells and shuttle macromolecules from the blood to the interstitium. Transcellular transport of macromolecules may involve receptor-dependent (for instance, albumin binding to GP60 protein) or -independent mechanisms (fluid phase transcytosis).
How is the endothelial barrier determined?
The integrity of the endothelial barrier is determined not only by the adhesive forces that couple endothelial cells with each other and to the extracellular matrix but also by the shape of endothelial cell. Endothelial adherens junctions link neighboring cells and consist in transmembrane VE-cadherins molecules, which are associated in the intercellular space, while the cytoplasmic tail is linked to catenins, which in turn are linked to the actin cytoskeleton [300]. Actin–myosin activation regulates the contractile function of endothelial cells. This calcium-dependent process is activated by inflammatory mediators. The traction exerted can thus disrupt the adherens junctions, precipitating the retraction of the endothelial cells [1051,1340]. This is a dynamic and reversible process. In experimental models, proper endothelial permeability and barrier integrity are generally restored within minutes (bradykinin or histamine) or hours (VEGF) following the administration of the inducing agent [412,424].
How do leukocytes interact with endothelium?
These interactions contribute to the immune response, wound repair and thrombosis as well as to acute and chronic inflammation. The passage of leukocytes from the circulation to the surrounding tissue requires the adhesion of the leukocyte to the endothelial cell surface, a multi-step cascade, already described in detail in the late 19th century [266], involving the capture (or tethering), rolling and arrest of the leukocytes, followed by their transmigration (or diapedesis). Again, these steps, often associated with inflammation, take place predominantly but not exclusively in post-capillary venules, since they can be observed in large veins, capillaries and arterioles [20,905].
Which type of cell is coupled by tight junctions and anchored to a continuous basal membrane?
Endothelial cells are coupled by tight junctions and anchored to a continuous basal membrane. Fenestrated endothelium is also associated with a continuous basal membrane and is characterized by the presence of transcellular 50–60 nm wide pores, which are sealed by a 5- to 6-nm-thick diaphragm.
Which cells regulate hemostasis?
For instance, endothelial cells in general regulate hemostasis. However, endothelium-derived products that, on the one hand, maintain blood fluidity and, on the other hand, are involved in the coagulation cascade and the formation of blood clot, are unevenly distributed over the vascular tree.
What is the function of endothelial cells?
Endothelial cells form the barrier between vessels and tissues ( Aman et al., 2016 ). They control the flow of substances and fluid into and out of a tissue. An impaired function can lead to serious health issues throughout the body. Endothelial cells line blood vessels and lymphatic vessels, they are found exclusively in vascularized tissue ...
Where are endothelial cells found?
Endothelial cells can be found in all large vessels , namely arteries and veins, as well as in capillaries ( Alberts B, Johnson A, Lewis J, et al., 2002 ). An artery consists of three layers (see illustration above): On the outside, it is sheathed with the Tunica externa, a type of connective tissue. The Tunica media is made up of smooth muscle cells, and the Tunica intima, which contains endothelial cells, lines the lumen of the blood vessel. All endothelial cells share certain molecular characteristics: they test positive for von Willebrand factor (vWF), as well as for CD31 glycoprotein, and they test negative for smooth muscle alpha-actin.
How big are endothelial cells?
Endothelial cells from various organs add another dimension of complexity. If you want to describe the size of endothelial cells, you need to specify which type. Garipcan and his team found iliac artery endothelial cells to be 13.2 ± 4.1 μ m in width and 25.8 ± 8.5 μm in length ( Garipcan et al., 2010 ). However, they described the width of hepatic artery endothelial cells as 4.9 ± 1.5 μm and 21.9 ± 6.6 μm in length.
What is the role of endothelial cells in glomerular filtration?
In the kidneys, endothelial cells play a key role in glomerular filtration ( Satchell and Braet, 2009 ). Fenestrations in the endothelium allow for passage of molecules with a defined size. This prevents an excessive loss of proteins . This mechanism complements the filtration occurring through podocyte filtration slits.
What are the characteristics of endothelial cells?
All endothelial cells share certain molecular characteristics: they test positive for von Willebrand factor (vWF), as well as for CD31 glycoprotein, and they test negative for smooth muscle alpha-actin. This also applies to endothelial cells in capillaries.
Why are endothelial cells important?
Angiogenesis and healthy endothelial cells are important for virtually all bodily functions. Researchers have been working on methods for studying endothelial cells in vitro for decades, to decipher the various factors that affect formation of new blood vessels in the human body.
What are the three cell types in the heart?
In the heart, three cell types enable the lifelong function of this continuously working organ: endothelial cells, fibroblasts, and cardiomyocytes ( Lim et al., 2014 ). The communication between these cell types allows for organ development, autoregulation, and adaptation. The most rigid separation between vessels and tissue can be found in ...
How do endothelial cells proliferate?
The proliferation of endothelial cells can be demonstrated by using 3H-thymidine to labelcells synthesizing DNA. In most adult tissues, endothelial cells turn over very slowly, with a cell lifetime ranging, for a mouse, from a couple of months (in liver and lung) to years (in brain and muscle). But endothelial cells not only repair and renew the lining of established blood vessels, they also create new blood vessels. They must do this in embryonic tissues to keep pace with growth, in normal adult tissues to support recurrent cycles of remodeling and reconstruction (as, for example, in the lining of the uterus during the menstrual cycle), and in damaged adult tissues to support repair. In such circumstances, they can be roused to proliferate with a doubling time of just a few days. There is some evidence that, where there is a call for rapid blood-vessel growth, the local population of endothelial cells may also increase by recruitment from the blood stream, which has been reported to contain small numbers of endothelial precursor cells derived from the bone marrow.
How do endothelial cells form a capillary?
Observations such as these reveal that endothelial cells that are to form a new capillary grow out from the side of an existing capillary or small venule by extending long pseudopodia, pioneering the formation of a capillary sprout that hollows out to form a tube (Figure 22-25). This process continues until the sprout encounters another capillary, with which it connects, allowing blood to circulate. Endothelial cells on the arterial and venous sides of the developing network of vessels differ in their surface properties, in the embryo at least: the plasma membranes of the arterial cells contain the transmembrane proteinephrin-B2 (see Chapter 15), while the membranes of the venous cells contain the corresponding receptorprotein, Eph-B4, which is a receptor tyrosine kinase (discussed in Chapter 15). These molecules mediate a signal delivered at sites of cell-cell contact, and they are essential for the developmentof a properly organized network of vessels. One suggestion is that they somehow define the rules for joining one piece of growing capillary tube to another.
How do endothelial cells respond to the invaders?
In all these cases, the invading endothelial cells respond to signals produced by the tissue that they invade. The signals are complex, but a key part is played by a proteinknown as vascular endothelial growth factor(VEGF), a distant relative of platelet-derived growth factor (PDGF). The regulation of blood vessel growth to match the needs of the tissue depends on the control of VEGF production, through changes in the stability of its mRNAand in its rate of transcription. The latter control is relatively well understood. A shortage of oxygen, in practically any type of cell, causes an increase in the intracellular concentration of the active form of a gene regulatory proteincalled hypoxia-inducible factor 1(HIF-1). HIF stimulates transcription of the VEGF gene (and of other genes whose products are needed when oxygen is in short supply). The VEGF protein is secreted, diffuses through the tissue, and acts on nearby endothelial cells.
What are the cells that control the passage of materials?
Thus, endothelial cells line the entire vascular system, from the heart to the smallest capillary, and control the passage of materials—and the transit of white blood cells—into and out of the bloodstream. A study of the embryo reveals, moreover, that arteries and veins develop from small vessels constructed solely of endothelial cells and a basallamina: pericytes, connective tissueand smooth muscle are added later where required, under the influence of signals from the endothelial cells . The recruitment of pericytes in particular depends on PDGF-B secreted by the endothelial cells , and in mutants lacking this signal proteinor its receptor, pericytes in many regions are missing. As a result, the embryonic blood vessels develop microaneurysms—microscopic pathological dilatations—that eventually rupture, as well as other abnormalities, reflecting the importance of signals exchanged in both directions between the pericytes and the endothelial cells.
What is the process of creating a blood capillary?
Angiogenesis. A new blood capillary forms by the sprouting of an endothelial cell from the wall of an existing small vessel. This diagram is based on observations of cells in the transparent tail of a living tadpole. (After C.C. Speidel, Am. J. Anat.(more...)
Which cell layer regulates the flow of blood between the bloodstream and the surrounding tissues?
Summary. Endothelial cells form a single cell layer that lines all blood vessels and regulates exchanges between the bloodstream and the surrounding tissues. Signals from endothelial cells organize the growth and developmentof connective tissuecells that form the surrounding layers of the blood-vessel wall.
Which cells retain a capacity for cell divisionand movement?
Throughout the vascular system of the adult body, endothelial cells retain a capacity for cell divisionand movement. If, for example, a part of the wall of the aorta is damaged and denuded of endothelial cells, neighboring endothelial cells proliferate and migrate in to cover the exposed surface.
What is the vascular endothelium?
The vascular endothelium is a monolayer of cells between the vessel lumen and the vascular smooth muscle cells. Nitric oxide (NO) is a soluble gas continuously synthesized from the amino acid L-arginine in endothelial cells by the constitutive calcium-calmodulin-dependent enzyme nitric oxide synthas ….
What is the role of nitric oxide in endothelial cells?
The role of nitric oxide on endothelial function. The vascular endothelium is a monolayer of cells between the vessel lumen and the vascular smooth muscle cells. Nitric oxide (NO) is a soluble gas continuously synthesized from the amino acid L-arginine in endothelial cells by the constitutive calcium-calmodulin-dependent enzyme nitric oxide synthas ...
What is the nitric oxide in the endothelium?
The vascular endothelium is a monolayer of cells between the vessel lumen and the vascular smooth muscle cells. Nitric oxide (NO) is a soluble gas continuously synthesized from the amino acid L-arginine in endothelial cells by the constitutive calcium-calmodulin-dependent enzyme nitric oxide synthase (NOS). This substance has a wide range of ...
What are the functions of endothelial cells?
Endothelial cells act as selective filters to regulate the passage of gases, fluid and various molecules across their membranes. For example, your white blood cells or leucocytes are produced in the bone marrow. They travel through the blood stream where the endothelial cells facilitate their passage into your body’s tissue to allow them to destroy foreign agents or antigens. Endothelial cells also synthesize the vitally important molecule called Factor VIII or von Willibrand’s Factor which is essential for blood clotting. Without this molecule a person could bleed to death from a simple scratch.
What is the name of the molecule that is used to create nitric oxide?
L-arginine is called the “MIRACLE MOLECULE” and the 1998 Nobel Prize in Medicine was awarded to the researchers of Nitric Oxide. The best and most effective L-arginine product for the creation of Nitric Oxide to provide far-reaching health benefits and powerful support for the cardiovascular system is ProArgi9 Plus!
What causes the smooth and flexible lining of your blood vessels to become rough and hard?
This causes the smooth and flexible lining of your blood vessels to become rough and hard leading to the disease commonly called arteriosclerosis or atherosclerosis. As this process continues over time, the deposits or plaques become larger which narrows the interior of the blood vessel making it harder for blood to pass through. This increases resistance to blood flow which can cause your blood pressure to increase.
Does smoking damage endothelial cells?
High blood pressure, high sugar levels, cholesterol and other lipid deposits, and smoking will damage your endothelial cells. Properly bringing in a good source of L-arginine, combined with good eating and lifestyle habits like those found in the Mediterranean diet, can help reverse this damage to the endothelial cells so that they can stay healthy to produce a good supply of nitric oxide. Your heart and other key organs will thank you.

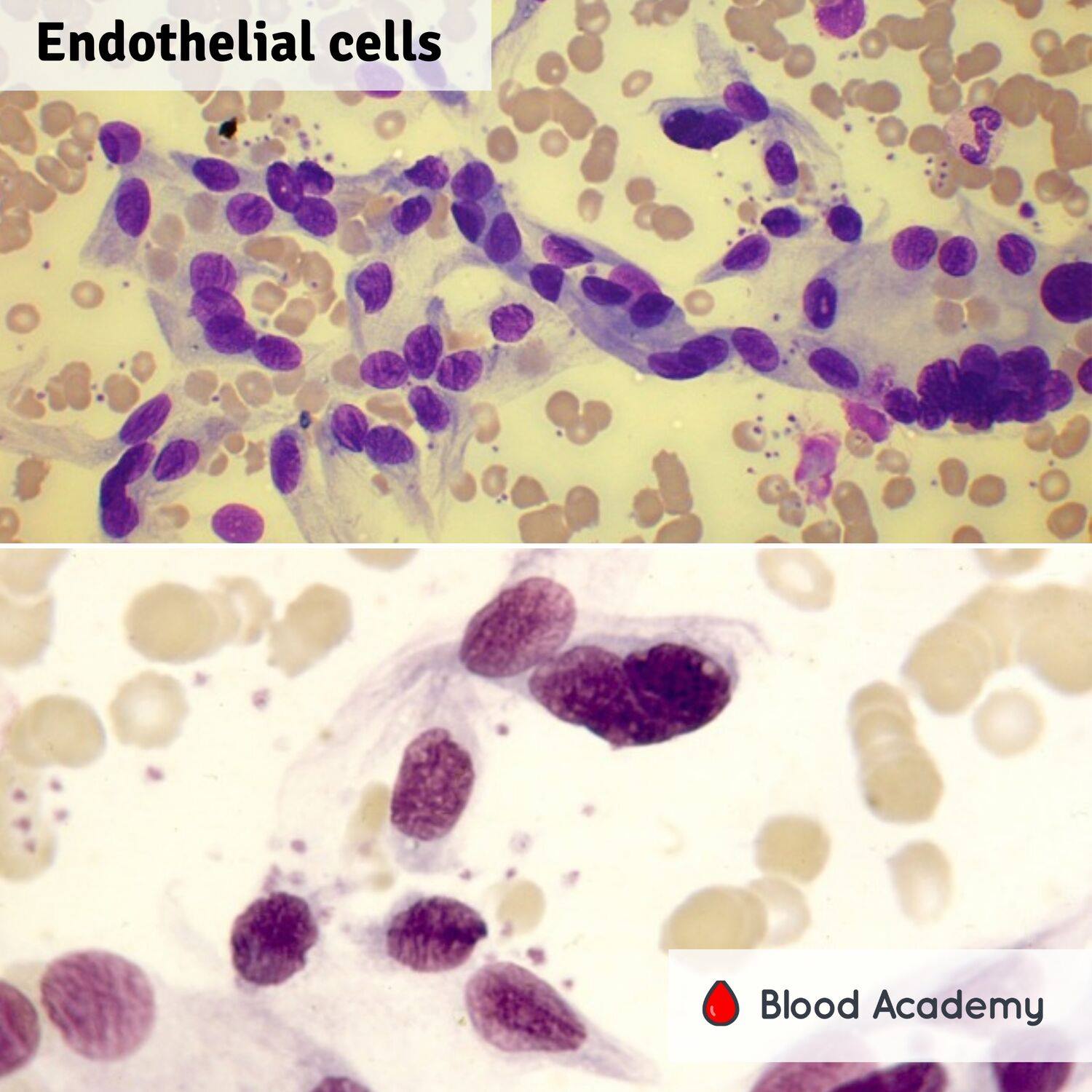
Definition
Morphology
- However, different subtypes of endothelial cells exist. Particular molecular markers distinguish endothelial cells that are found in lymphatic vessels from those that originate from blood vessels (Bautch and Caron, 2015). Endothelial cells from various organs add another dimension of complexity. If you want to describe the size of endothelial cells, you need to specify which type. …
Function
- In medical research, endothelial cells are no longer seen as a passive barrier, but as a tissue that fulfills various functions (Michiels, 2003). These include numerous processes, such as blood vessel formation, coagulation and fibrinolysis, regulation of vascular tone, to a role in inflammation. Endothelial cells originate from the mesoderm, a germinal layer that forms at gast…
Where Are Endothelial Cells Found?
- Endothelial cells can be found in all large vessels , namely arteries and veins, as well as in capillaries (Alberts B, Johnson A, Lewis J, et al., 2002). An artery consists of three layers (see illustration above): On the outside, it is sheathed with the Tunica externa, a type of connective tissue. The Tunica media is made up of smooth muscle cells, and the Tunica intima, which cont…
Heart, Brain, Liver, Lungs and Kidney
- In the heart, three cell types enable the lifelong function of this continuously working organ: endothelial cells, fibroblasts, and cardiomyocytes (Lim et al., 2014). The communication between these cell types allows for organ development, autoregulation, and adaptation. The most rigid separation between vessels and tissue can be found in the brain (Stamatovic et al., 2008). This s…
Pathology and Cancer
- Endothelial cells are nearly ubiquitous throughout the body. However, there are two major instances where dysfunction of endothelial cells is involved in pathogenesis of a medical condition. First, in coronary artery disease, endothelial cells are damaged. So the generation of new vascular cells to restore organ function following a myocardial infarction is of high researc…
Bioassays with Endothelial Cells
- Angiogenesis and healthy endothelial cells are important for virtually all bodily functions. Researchers have been working on methods for studying endothelial cells in vitro for decades, to decipher the various factors that affect formation of new blood vessels in the human body. Many cell types can be used in cell culture research (Read our blog poston primary endothelial cells). …
Promocell Endothelial Cell Culture
- The in vitroculture of primary human endothelial cells is a widely established model system used to investigate several cardiovascular diseases and cancer research applications. Our comprehensive endothelial cell culture portfolio consists of 12 different types of large vessel and microvascular human endothelial cells with optimized growth media for each cell type. 1. Tissu…