
not present
| Enzyme | see Enzyme inhibition |
| Ion channel | See Ion channel modulators |
| Receptor & transporter | BA / M Adrenergic Adrenergic receptor ag ... |
| Miscellaneous | Cofactor (see Enzyme cofactors) Precurso ... |
Is muscarinic the same as cholinergic?
The adverse effects of cholinergic drugs (also known as Muscarinic effects or Cholinergic Syndrome) can be easily remembered with the acronym SLUDGE-M. If you noticed, it’s just its exact opposite – the SYMPATHETIC effect.
What do muscarinic antagonists mean?
Muscarinic antagonists (antimuscarinic agents) are a group of anticholinergic drugs that competitively inhibit postganglionic muscarinic receptors. As such, they have a variety of applications that involve the parasympathetic nervous system .
What is muscarinic antagonist?
The muscarinic antagonist is a class medication used to manage and treat numerous different conditions, including COPD and organophosphate toxicity.
What are examples of agonist and antagonist drugs?
Examples of full agonists are heroin, oxycodone, methadone, hydrocodone, morphine, opium and others. An antagonist is a drug that blocks opioids by attaching to the opioid receptors without activating them. Antagonists cause no opioid effect and block full agonist opioids. Examples are naltrexone and naloxone.
What do muscarinic antagonist do?
Muscarinic receptor antagonists (MRAs) function by competitively blocking the cholinergic response manifested by acetylcholine (ACh) binding muscarinic receptors on exocrine glandular cells, cardiac muscle cells, and smooth muscle cells.
What does the muscarinic receptor do?
Introduction. Muscarinic receptors recognize the neurotransmitter acetylcholine, translating this recognition into electrical transients and altered cell behavior by activating and suppressing an assortment of signaling pathways.
What happens when muscarinic receptors are activated?
The M2 muscarinic receptor is widely distributed in mammalian tissues and is the only subtype found in the human heart. Its activation results in a decrease in heart rate and a reduction in heart contraction force (3).
Do muscarinic receptors cause vasoconstriction?
Conclusions. These findings provide evidence that in murine ophthalmic arteries the muscarinic M3 receptor subtype mediates cholinergic endothelium-dependent vasodilation and endothelium-independent vasoconstriction.
Is muscarine an agonist or antagonist?
Muscarine is the prototypical agonist for all muscarinic receptors (muscarine is an alkaloid derived from mushrooms and is associated with toxicity when poisonous mushrooms are ingested).
What's the difference between cholinergic and muscarinic receptors?
Nicotinic and muscarinic receptors are the two main types of cholinergic receptors. Activated nicotinic receptors serve as ion channels while activated muscarinic receptors phosphorylate second messengers to mediate metabolic responses. The nicotinic receptors facilitate the transmission of nerve impulses.
Why does muscarine cause sweating?
Acetylcholine released from cholinergic nerves can activate both muscarinic and nicotinic receptors; each is known independently to induce cutaneous vasodilatation and eccrine sweating in humans.
What's the difference between muscarinic and nicotinic receptors?
The nicotinic receptor is a channel protein that, upon binding by acetylcholine, opens to allow diffusion of cations. The muscarinic receptor, on the other hand, is a membrane protein; upon stimulation by neurotransmitter, it causes the opening of ion channels indirectly, through a second messenger.
What is antimuscarinic medication?
Antimuscarinic medications are a group of anticholinergic agents, specifically known for blocking the activity of muscarinic receptors. These receptors play an important role in mediating the functions of the parasympathetic nervous system, which controls many involuntary functions to conserve energy, including the contraction of smooth muscle, ...
How does antimuscarinic work?
Antimuscarinic medications work by blocking muscarinic receptors from the action of acetylcholine, the chief chemical messenger controlling parasympathetic functions. Blocking the action of acetylcholine can ultimately influence neurologic function, increase heart rate, decrease smooth muscle motility, and decrease exocrine gland secretion.
What are the side effects of antimuscarinics?
Adverse effects resulting from the impaired secretion by exocrine glands are often a dry mouth and sore throat.
What is the name of the drug that blocks cholinergic receptors?
Anticholinergics refer to agents that block cholinergic receptors, or acetylcholine receptors. Anticholinergics are divided into 2 categories: antimuscarinics, which block muscarinic receptors, and antinicotinics, which block nicotinic receptors.
What is the effect of a parasympathetic nervous system on heart rate?
This leads to the inhibition of several functions of the parasympathetic nervous system, and can result in an increased heart rate, decreased smooth muscle motility, decreased exocrine secretions, or influence neurologic functions.
Can antimuscarinics help with asthma?
Finally, antimuscarinics can be helpful for individuals with certain respiratory conditions, such as asthma and chronic obstructive pulmonary disease. These medications serve as muscle relaxants in the lungs, which help individuals breathe more easily.
Can you take antimuscarinics with dry mouth?
For that reason, individuals should consult with their healthcare provider before taking antimuscarinics medications. Overdosing on antimuscarinics may lead to anticholinergic syndrome, which can present with dry mouth, flushed skin, tachycardia, confusion, and agitation.
Who needs a long acting muscarinic antagonist?
Who needs a long-acting muscarinic antagonist? In general, people who need more than an inhaled steroid to treat their asthma are those classified as having persistent, poorly-controlled asthma . These are people who have ongoing symptoms, even after consistently taking their inhaled steroids.
What is a long acting bronchodilator?
Another class of medications called long-acting beta agonists (LABAs for short) are more commonly used in treating severe asthma. LABAs are also long-acting bronchodilators. Frequently, they are combined with an inhaled steroid, when the steroid alone does not sufficiently provide asthma control. 4 Examples include formoterol and salmeterol.
What are muscarinic antagonists used for?
Drugs with muscarinic antagonist activity are widely used in medicine, in the treatment of low heart rate, overactive bladder, respiratory problems such as asthma and COPD, and neurological problems such as Parkinson's disease and Alzheimer's disease.
What is the function of muscarinic antagonists?
Notably, muscarinic antagonists reduce the activation of the parasympathetic nervous system. The normal function of the parasympathetic system is often summarised as "rest-and-digest", and includes slowing of the heart, an increased rate of digestion, narrowing of the airways, promotion of urination, and sexual arousal.
What is the MRA?
Metabotropic acetylcholinergic receptors. A muscarinic receptor antagonist ( MRA) is a type of anticholinergic agent that blocks the activity of the muscarinic acetylcholine receptor. The muscarinic receptor is a protein involved in the transmission of signals through certain parts of the nervous system, and muscarinic receptor antagonists work ...
What are the two most commonly used anticholinergics?
Most muscarinic receptor antagonists are synthetic chemicals; however, the two most commonly used anticholinergics, scopolamine and atropine, are belladonna alkaloids, and are naturally extracted from plants such as Atropa belladonna, the deadly nightshade.
What is the effect of atropine on the heart?
Atropine acts on the M2 receptors of the heart and antagonizes the activity of acetylcholine. It causes tachycardia by blocking vagal effects on the sinoatrial node. Acetylcholine hyperpolarizes the sinoatrial node, which is overcome by MRA and thus increases the heart rate.
What are the antagonists of vasodilation?
Important muscarinic antagonists include atropine, Hyoscyamine, hyoscine butylbromide and hydrobromide, ipratropium, tropicamide, cyclopentolate, and pirenzepine .
Does parkinsonism decrease dopaminergic activity?
Thus, in parkinsonism there is decreased level of dopaminergic activity. One method of balancing the neurotransmitters is through blocking central cholinergic activity using muscarinic receptor antagonists. Atropine acts on the M2 receptors of the heart and antagonizes the activity of acetylcholine.

Overview
Clinical significance
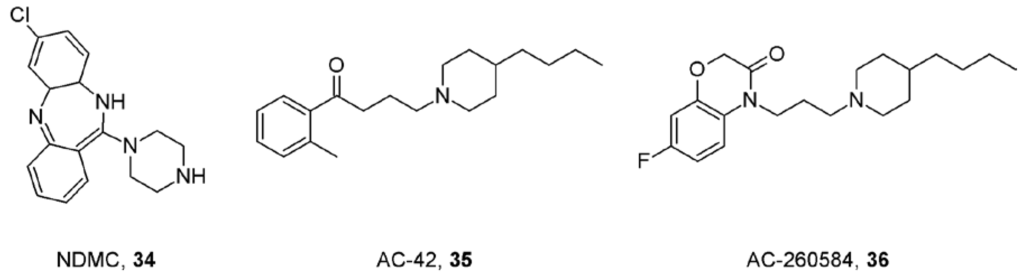
M1-type muscarinic acetylcholine receptors play a role in cognitive processing. In Alzheimer disease (AD), amyloid formation may decrease the ability of these receptors to transmit signals, leading to decreased cholinergic activity. As these receptors themselves appear relatively unchanged in the disease process, they have become a potential therapeutic target when trying to improve cognitive function in patients with AD.
Muscarinic acetylcholine receptor subtypes
The targets for muscarinic agonists are the muscarinic receptors: M1, M2, M3, M4 and M5. These receptors are GPCRs coupled to either Gi or Gq subunits.
See also
• Muscarine
• Muscarinic acetylcholine receptor
• Muscarinic antagonist
• Nicotinic acetylcholine receptor
External links
• Muscarinic+Agonists at the US National Library of Medicine Medical Subject Headings (MeSH)