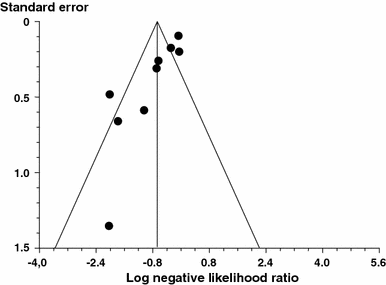
The authors concluded that a positive cuff-leak test (i.e., absence of an air-leak) indicates an elevated risk of upper airway obstruction and re-intubation. A negative cuff-leak test (i.e., presence of an air-leak), however, does not reliably exclude the presence of upper airway edema or the need for subsequent re-intubation.
Can cuff leak test be used to predict edema?
However the discrimination power of the cuff-leak test is highly variable and can be use, at best, to detect patients at risk to develop edema but should not be used to postpone extubation as tracheal extubation can still be successful in many patients with a positive test.
What do we know about cuff leaks and airway examination?
Of the 1,460 patient encounters in the database identified as an “evaluation for a cuff leak,” airway examination revealed that 699 patients proved to have a properly positioned ETT accompanied with a cuff perforation, an incompetent valve/pilot balloon, line assembly dysfunction or leak, or ETT damage (e.g., damage to the ETT wall from biting).
How do you determine cuff leak volume?
The threshold cuff-leak volume was determined by visual inspection of the receiver-operating characteristic plot. A leak of < 110 mL was considered a positive result of the CLT and indicated that patients were at risk for post-extubation stridor secondary to laryngeal edema. 3
What causes a low value for the cuff leak test?
a low value for cuff leak can also be caused by encrusted secretions around the tube rather than by a narrowed upper airway De Backer D. The cuff-leak test: what are we measuring? Crit Care. 2005 Feb;9 (1):31-3. Epub 2004 Dec 17. PubMed PMID: 15693980; PubMed Central PMCID: PMC1065116. Miller RL, Cole RP.
Why is it important to investigate a cuff leak?
How many patients were ventilated with a cuff leak?
How long was the man intubated for a cuff leak?
Why is air leak in the ICU so challenging?
Where is the cuff in grade 1?
Is VL more common in grade I cases than FFB?
See 1 more
What is positive cuff leak test?
The cuff-leak test has been proposed as a simple method to predict the occurrence of post-extubation stridor. The test is performed by cuff deflation and measuring the expired tidal volume a few breaths later (VT). The leak is calculated as the difference between VT with and without a deflated cuff.
What does a negative cuff leak test indicate?
Consistent with these findings, the nomogram suggested that while a negative cuff leak test represents low possibility of post-extubation airway obstruction, a positive test still provides a relatively low posttest probability.
What does a positive cuff leak test indicate quizlet?
What does a positive cuff leak test indicate? The patient is at minimal risk for upper airway obstruction. What is the most common complication of suctioning? Hypoxemia. After an intubation attempt, an expired capnogram indicates a CO2 level near zero.
What does it mean to have a cuff leak?
The 'cuff-leak' test, which involves demonstrating a leak around a tracheal tube with the cuff deflated, has been advocated to determine the safety of extubation in patients with upper airway obstruction. In 62 such patients we were able safely to extubate all patients with a cuff leak.
What does leak mean on ventilator?
Introduction. During mechanical ventilation, system leak is a major cause of patient-ventilator asynchrony. Leaks may be due to the endotracheal tube cuff, ventilator circuit, or chest drain during invasive ventilation. The incidence of endotracheal tube cuff leaks has been reported at ranges from 11% to 24%.
How do you check for leak in ICU?
PROCEDURESuction endotracheal and oral secretions and set the ventilator in the assist control mode with the patient receiving volume-cycled ventilation.With the cuff inflated, record displayed inspiratory and expiratory tidal volumes to see whether these are similar.Deflate the cuff.More items...
What is the purpose of a cuff on an artificial tracheal airway?
A cuff prevents the escape of air between the tube and the walls of the trachea and reduces aspiration when a patient is receiving mechanical ventilation.
What is the primary indication for tracheal suctioning?
Suctioning is performed when the patient is unable to effectively move secretions from the respiratory tract. This may occur with excessive production of secretions or ineffective clearance, which leads to the accumulation of secretions in the upper and lower respiratory tract.
What is the primary indication for tracheostomy?
A tracheostomy is usually done for one of three reasons: to bypass an obstructed upper airway; to clean and remove secretions from the airway; to more easily, and usually more safely, deliver oxygen to the lungs.
What are the criteria for extubation?
Extubation should not be performed until it has been determined that the patient's medical condition is stable, a weaning trial has been successful, the airway is patent, and any potential difficulties in reintubation have been identified.
Which of the following is a potential complication of a low pressure in the endotracheal cuff?
Which of the following is a potential complication of a low pressure in the ET cuff? Low pressure in the cuff can increase the risk for aspiration pneumonia. High cuff pressure can cause tracheal bleeding, ischemia, and pressure necrosis.
What is laryngeal edema?
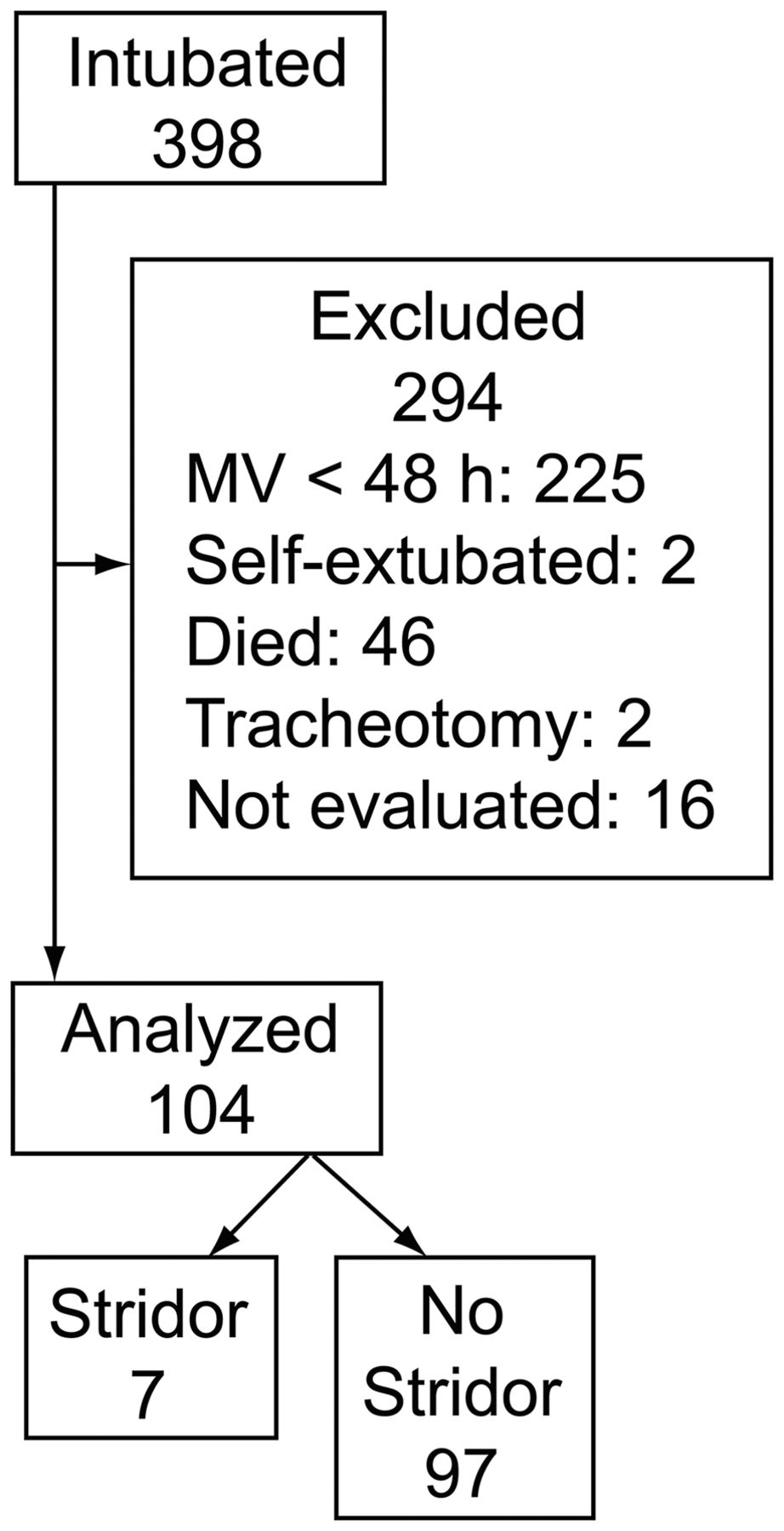
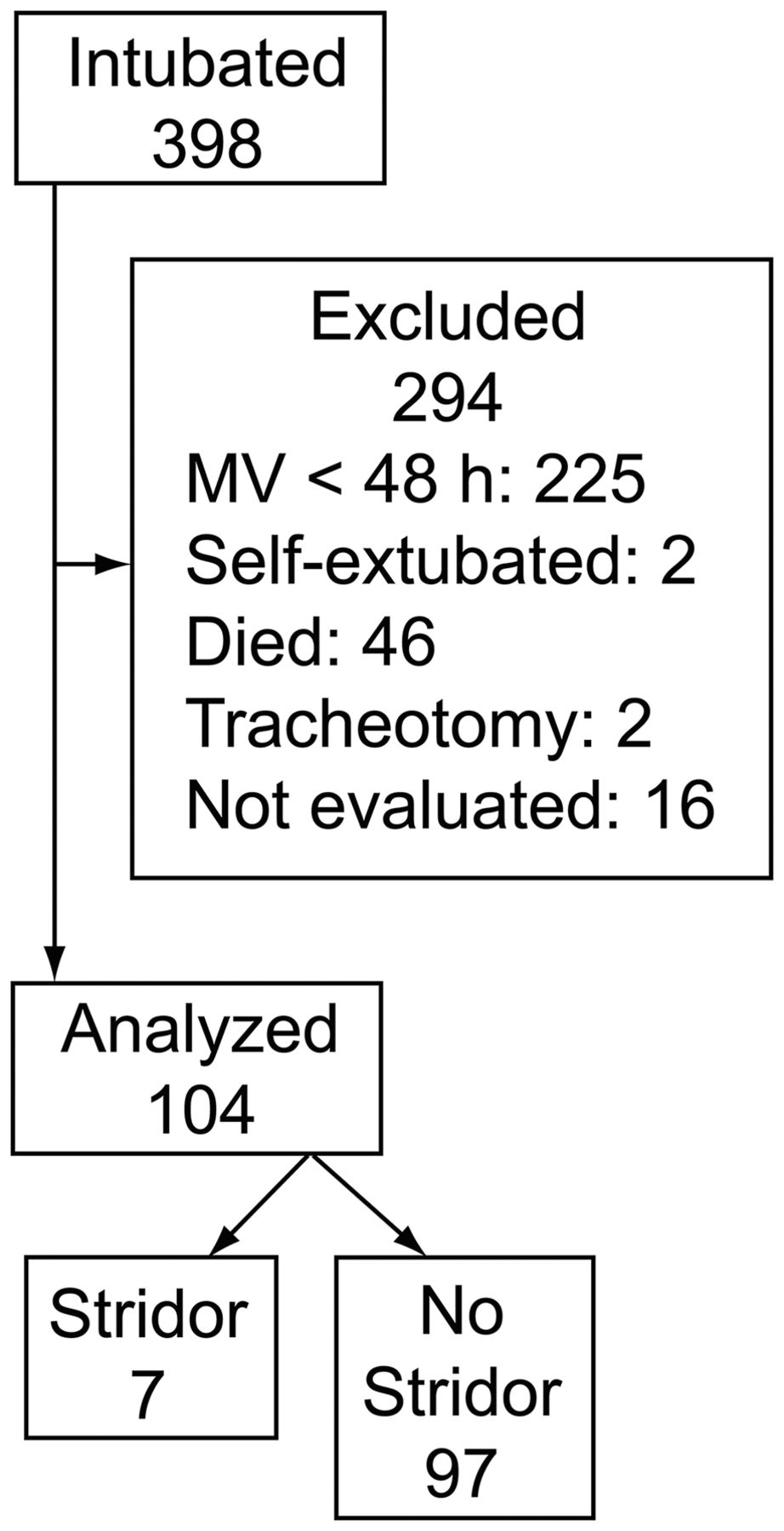
Laryngeal edema (LE) is a frequent complication of intubation and is caused by trauma to the larynx [1, 2]. The edema results in a decreased size of the laryngeal lumen, which may present as stridor or respiratory distress (or both) following extubation.
Can you Extubate without a cuff leak?
Absence of cuff leak can also occur due to having a large tube relative to the patient's trachea, or caked secretions around the tube. Thus, many patients without a cuff leak may still be safely extubated.
What is the normal cuff pressure?
A cuff pressure between 20 and 30 cm H2O is recommended to provide an adequate seal and reduce the risk of complications. Survey results5–7 indicate that cuff pressure is usually monitored and adjusted every 8 to 12 hours.
What are the criteria for extubation?
Extubation should not be performed until it has been determined that the patient's medical condition is stable, a weaning trial has been successful, the airway is patent, and any potential difficulties in reintubation have been identified.
What is laryngeal edema?
Laryngeal edema (LE) is a frequent complication of intubation and is caused by trauma to the larynx [1, 2]. The edema results in a decreased size of the laryngeal lumen, which may present as stridor or respiratory distress (or both) following extubation.
The cuff-leak test: what are we measuring? - Critical Care
Stridor is one of the most frequent causes of early extubation failure. The cuff-leak test may help to identify patients at risk to develop post-extubation laryngeal edema. However the discrimination power of the cuff-leak test is highly variable and can be use, at best, to detect patients at risk to develop edema but should not be used to postpone extubation as tracheal extubation can still ...
The cuff-leak test: what are we measuring? - PMC - PubMed Central (PMC)
In this issue, Prinianakis and colleagues [] shed some new light on the factors that might affect the leak, and hence the evaluation of the cuff-leak test.First, they separate the inspiratory and expiratory components of the leak. Usually, the leak is calculated by measuring five or more tidal volumes after deflation of the cuff.
Endotracheal tube cuff leaks: causes, consequences, and management
The consequences of endotracheal tube (ETT) cuff leak may range from a bubbling noise to a life-threatening ventilatory failure. Although the definitive solution is ETT replacement, this is often neither needed nor safe to perform. Frequently, the leak is not caused by a structural defect in the ETT …
Why is it important to investigate a cuff leak?
Due to the variety of cuff leak etiologies, it is imperative to investigate the leak rather than assume that the ETT cuff is leaking or dysfunctional. Determining the cause of the cuff leak will assist in planning corrective measures, if indicated. Thus, an airway assessment and review of the patient’s history and recent bedside activities—for example, recent placement of a feeding tube—may offer valuable information to assist the airway team in the delivery of optimal patient care.
How many patients were ventilated with a cuff leak?
Overall, a total of 1,460 mechanically ventilated patients with a cuff leak were documented in the database (years 2005-2018) and underwent assessment by the anesthesia airway team.
How long was the man intubated for a cuff leak?
Intubated for 12 days, he remained dependent on mechanical support due to malnutrition and his respiratory limitations.
Why is air leak in the ICU so challenging?
An “air leak” in the ICU is often more challenging because of its remote location. Being summoned to a remote location presents unique issues. The acutely ill ICU patient is likely unknown to the airway team. Moreover, a plethora of conditions mark the mechanically ventilated ICU patient in an elevated risk category compared with most elective surgical patients. Suboptimal or limited airway visualization due to an indwelling endotracheal tube (ETT), secretions, edema, limited oral access, cervical spine appliances, the presence of orogastric feeding tubes, anatomic constraints and restricted positioning abilities are just a few of the challenging conditions that make the ICU patient unique. 1-6
Where is the cuff in grade 1?
In grade I, the cuff is between the vocal cords (Figur e 2).
Is VL more common in grade I cases than FFB?
Although management was random and noncontrolled, VL use was more common in grade I and II cases, whereas FFB use was considered the primary method mainly for grade II and III cases (Table 4). Of note, many events categorized as FFB actually had a VL assessment performed initially.
Why is it important to investigate a cuff leak?
Due to the variety of cuff leak etiologies, it is imperative to investigate the leak rather than assume that the ETT cuff is leaking or dysfunctional. Determining the cause of the cuff leak will assist in planning corrective measures, if indicated. Thus, an airway assessment and review of the patient’s history and recent bedside activities—for example, recent placement of a feeding tube—may offer valuable information to assist the airway team in the delivery of optimal patient care.
How many patients were ventilated with a cuff leak?
Overall, a total of 1,460 mechanically ventilated patients with a cuff leak were documented in the database (years 2005-2018) and underwent assessment by the anesthesia airway team.
How long was the man intubated for a cuff leak?
Intubated for 12 days, he remained dependent on mechanical support due to malnutrition and his respiratory limitations.
Why is air leak in the ICU so challenging?
An “air leak” in the ICU is often more challenging because of its remote location. Being summoned to a remote location presents unique issues. The acutely ill ICU patient is likely unknown to the airway team. Moreover, a plethora of conditions mark the mechanically ventilated ICU patient in an elevated risk category compared with most elective surgical patients. Suboptimal or limited airway visualization due to an indwelling endotracheal tube (ETT), secretions, edema, limited oral access, cervical spine appliances, the presence of orogastric feeding tubes, anatomic constraints and restricted positioning abilities are just a few of the challenging conditions that make the ICU patient unique. 1-6
Where is the cuff in grade 1?
In grade I, the cuff is between the vocal cords (Figur e 2).
Is VL more common in grade I cases than FFB?
Although management was random and noncontrolled, VL use was more common in grade I and II cases, whereas FFB use was considered the primary method mainly for grade II and III cases (Table 4). Of note, many events categorized as FFB actually had a VL assessment performed initially.