
Explore
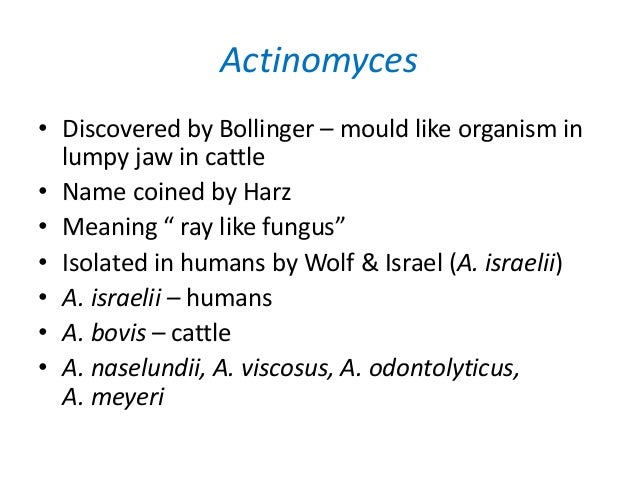
[ak′tinōmī′sēz] , pl. actinomycetes. Etymology: Gk, aktis, ray, mykes, fungus. a genus of anaerobic or facultative anaerobic, gram-positive bacteria. Species that may cause disease in humans, such as Actinomyces israelii (which causes actinomycosis), are normally present in the mouth and throat.
What is the etymology of Actinomyces?
Actinomyces is a genus of the Actinobacteria class of bacteria. They are all gram-positive. Actinomyces species are facultatively anaerobic (except A. meyeri and A. israelii both obligate anaerobe ), and they grow best under anaerobic conditions. Actinomyces species may form endospores, and,...
Is Actinomyces aerobic or anaerobic?
Actinomycosis is a long-term infection that causes sores, or abscesses, in the body’s soft tissues. Actinomycosis is usually found in the: Actinomycosis rarely appears elsewhere in the body. However, it can spread from the initial infected area to other parts of the body if illness or injury damages your tissue. Actinomycosis isn’t contagious.
What is actinomycosis and how is it treated?
a hard, painful swelling in the soft tissue of the mouth, known as a “woody” fibrosis This is the most common form of infection caused by Actinomyces. It accounts for 50 percent of all cases, according to an article published in Antimicrobe.
What are the symptoms of Actinomyces infection?

How serious is Actinomyces?
Actinomycosis is a rare type of bacterial infection. It can be very serious but can usually be cured with antibiotics.
How do you get Actinomyces infection?
The bacteria that cause this infection typically live in dental plaque. It can result from: dental problems, such as decay and poor oral hygiene. trauma to the mouth or face, if particles of dental plaque enter the mucous membrane.
What is the meaning of Actinomyces?
Actinomycosis is a long-term (chronic) bacterial infection that commonly affects the face and neck.
What kind of infection is Actinomyces?
Actinomycosis is a rare subacute to chronic infection caused by the gram-positive filamentous non-acid fast anaerobic to microaerophilic bacteria, Actinomyces. The infection is usually a granulomatous and suppurative infection.
Can actinomycosis be fatal?
Local actinomycosis in head and neck lesions can be an intractable and sometimes fatal disease. Initial treatment is extremely important. Insufficient dose or intermittent dosage of antibiotics may not be able to control an Actinomyces infection in a patient in an immunocompromised state.
What happens if leaving actinomycosis untreated?
Thoracic actinomycosis commonly presents as a pulmonary infiltrate or mass, which, if left untreated, can spread to involve the pleura, pericardium, and chest wall, ultimately leading to the formation of sinuses that discharge sulfur granules.
Do you need to treat Actinomyces?
All forms of actinomycosis are treated with high doses of intravenous penicillin G over two to six weeks, followed by oral penicillin V (10). Surgical treatment may be necessary if there is extensive necrotic tissue, sinus tracts, fistulas, or if patients do not respond to medical treatment (4).
How long does it take Actinomyces to grow?
Actinomyces are non-spore-forming Gram-positive rods. Except for A. meyeri, which is small and nonbranching, all the other species are branching filamentous rods. Growth of Actinomyces is slow; it appears within at least 5 days and may take up to 15–20 days.
Is Actinomyces a fungus?
The name actinomycosis means “ray fungus,” and the organisms may resemble fungi owing to their filamentous appearance. Aerobic actinomyces are a large, diverse group of gram-positive bacteria (2).
What is the best antibiotic for Actinomyces?
Preferred regimens — We generally suggest high-dose penicillin for actinomycosis [1-3]. Reasonable alternatives include ceftriaxone and amoxicillin.
What kills Actinomyces?
Long-term, high-dose penicillin is the mainstay of actinomycosis treatment to completely eliminate the organism and prevent recurrence.
How do I know if I have actinomycosis?
Approaches to the detection of actinomycetes ranged from investigations of neglected habitats and extreme environments (e.g. alkaline soils and oil drills) to the analysis of DNA extracted from the environment and use of specific phages.
What is actinomyces in medical terms?
Medical Definition of actinomyces. 1 capitalized : a genus of filamentous or rod-shaped gram-positive bacteria of the family Actinomycetaceae that includes usually commensal and sometimes pathogenic forms inhabiting mucosal surfaces especially of the oral cavity — compare actinomycosis.
What is actinomyces in biology?
Definition of actinomyces. : any of a genus (Actinomyces) of filamentous or rod-shaped bacteria that includes usually commensal and sometimes pathogenic forms inhabiting mucosal surfaces especially of the oral cavity of warm-blooded vertebrates.
What is the most common cause of oral abscesses?
Actinobacteria are normally present in the gums, and are the most common cause of infection in dental procedures and oral abscesses. Many Actinomyces species are opportunistic pathogens of humans and other mammals, particularly in the oral cavity. In rare cases, these bacteria can cause actinomycosis, a disease characterized by the formation of abscesses in the mouth, lungs, or the gastrointestinal tract. Actinomycosis is most frequently caused by A. israelii, which may also cause endocarditis, though the resulting symptoms may be similar to those resulting from infections by other bacterial species. Aggregatibacter actinomycetemcomitans has been identified as being of note in periodontal disease .
What are the symptoms of a dog with actinomyces?
Symptoms include fever, abdominal pain, and weight loss. Actinomyces species have also been shown to infect the central nervous system in a dog "without history or evidence of previous trauma or other organ involvement.". Pelvic actinomycosis is a rare but proven complication of use of intrauterine devices.
What causes a lumpy jaw?
The genus is typically the cause of oral-cervicofacial disease. It is characterized by a painless "lumpy jaw". Lymphadenopathy is uncommon in this form of the disease. Another form of actinomycosis is thoracic disease, which is often misdiagnosed as a neoplasm, as it forms a mass that extends to the chest wall. It arises from aspiration of organisms from the oropharynx. Symptoms include chest pain, fever, and weight loss. Abdominal disease is another manifestation of actinomycosis. This can lead to a sinus tract that drains to the abdominal wall or the perianal area. Symptoms include fever, abdominal pain, and weight loss. Actinomyces species have also been shown to infect the central nervous system in a dog "without history or evidence of previous trauma or other organ involvement."
What is pelvic actinomycosis?
Pelvic actinomycosis is a rare but proven complication of use of intrauterine devices. In extreme cases, pelvic abscesses might develop. Treatment of pelvic actinomycosis associated with intrauterine devices involves removal of the device and antibiotic treatment.
How long does it take to cure actinomycosis?
Treatment for actinomycosis consists of antibiotics such as penicillin or amoxicillin for 5 to 12 months, as well as surgery if the disease is extensive.
What is the name of the organism that is found in soil?
The aspect of these colonies initially led to the incorrect assumption that the organism was a fungus and to the name Actinomyces, "ray fungus" (from Greek actis, ray or beam, and mykes, fungus). Actinomyces species are ubiquitous, occurring in soil and in the microbiota of animals, including the human microbiota.
What is commensal flora?
Certain species are commensal in the skin flora, oral flora, gut flora, and vaginal flora of humans and livestock. They are also known for causing diseases in humans and livestock, usually when they opportunistically gain access to the body's interior through wounds.
Actinomyces
a genus of gram-negative, non–acid fast, nonmotile bacteria that form branched filaments. It includes A. israe´lii and A. naeslun´dii, both of which cause human actinomycosis and periodontal disease.
Actinomyces
A genus of slow-growing, nonmotile, nonsporeforming, anaerobic to facultatively anaerobic bacteria (family Actinomycetaceae) containing gram-positive, irregularly staining filaments; diphtheroid cells may be predominant. They exhibit true branching while forming mycelial-type colonies. Most of the species produce a filamentous microcolony.
actinomyces
Any of various rod-shaped or filamentous, chiefly anaerobic bacteria of the genus Actinomyces, commonly found in the mammalian oral cavity and including pathogenic species, such as the causative agents of actinomycosis.
Actinomyces
A genus of slow-growing, facultatively anaerobic, nonmotile, nonspore-forming, gram-positive bacteria, which form branching, irregularly staining filaments, filamentous microcolonies, and metabolise by fermentation of certain sugars.
Actinomyces
Microbiology A genus of slow-growing, facultatively anaerobic, nonmotile, nonspore-forming, gram-positive bacteria, which form branching, irregularly staining filaments, filamentous microcolonies, and metabolize by fermentation of certain sugars. See Actinomycosis, Sulfur granules. Cf Bacteroides spp, Nocardiaspp.
What is the name of the bacteria that live deep inside the body?
In severe cases, the skin can break open, leaking large amounts of pus. Actinomyces bacteria are anaerobic. This means they live deep inside body tissues, where oxygen levels are very low. This type of bacterial infection can be harder to diagnose and often takes longer to treat than other types.
Why does Actinomycosis occur?
Actinomycosis happens when the Actinomyces species of bacteria spread through the body because of tissue damage. Most people have Actinomyces bacteria in the lining of the mouth, throat, digestive tract, and urinary tract, and it is present in the female genital tract.
How to diagnose actinomycosis?
To diagnose actinomycosis, a doctor may take a sample of sputum, pus, or tissue to send for microscopic investigation in a laboratory. Sometimes, the laboratory will make a culture of the bacteria. If the infection is present, the pus or tissue will usually contain yellow sulfur granules.
What happens if you pierce a fish bone?
If something sharp pierces the internal body tissues, such as a fish bone in the esophagus, the bacteria can spread . Actinomycosis can also happen if there is tooth decay or gum disease.
What is the name of the disease that resembles other infections?
Actinomycosis can take a variety of forms. It can also resemble other infections, and even neoplasms, or tumors.
How long does actinomycosis last?
Actinomycosis can persist for a long time. Long-term treatment with antibiotics, such as penicillin, is common. It may last from 8 weeks to over 12 months.
What is actinomycosis?
Actinomycosis is a rare, infectious disease in which bacteria spread from one part of the body to another through body tissues. Over time, it can result in linked abscesses, pain, and inflammation. It can affect the skin or deeper areas within the body and sometimes the blood.
Are we missing a good definition for actinomyces? Don't keep it to yourself..
The ASL fingerspelling provided here is most commonly used for proper names of people and places; it is also used in some languages for concepts for which no sign is available at that moment.
Definitions & Translations
Get instant definitions for any word that hits you anywhere on the web!
What is the most common disease in kangaroos?
Actinomycosis is the most common infectious disease of kangaroos ( 7 ). In 1958, Batty ( 8) isolated A. odontolyticus from persons with advanced dental caries. During the ensuing 40+ years, 23 patients with invasive infection caused by A. odontolyticus have been described in North America, Europe, and Asia ( 9 – 16 ).
What is the clinical disease of A. odontolyticus?
Clinical disease in patients with A. odontolyticusclosely resembles disease caused by A. israeliiand other actinomyces species. Similar to A. israeliiinfections, those caused by A. odontolyticusprimarily involve the cervicofacial regions, the chest, abdomen, and pelvis with rare involvement of the central nervous system, bones, and joints. Additional similarities include a more frequent occurrence in men than women and a peak incidence in the middle decades of life. Clinical features in 97% of 181 patients with actinomycosis including the following: mass or swelling, pulmonary disease, draining abscesses, abdominal disease, dental disease, and intracranial infection (17).
What is Actinomyces odontolyticus?
Actinomyces odontolyticusis an anaerobic, facultative capnophilic, gram-positive, nonsporulating, nonacid fast, non-motile, irregularly staining bacterium. Sometimes short or medium-sized rods resembling diphtheroids are seen. Shorter rods resembling propionibacteria are frequently seen with A. odontolyticusand may be arranged in palisades as well as other diphtheroidal arrangements. On blood agar, the bacteria develop as small, irregular, whitish colonies that are smooth to slightly granular and show a dark red pigment when mature (2–14 days). This pigmentation is most obvious when the cultures are left standing in air at room temperature after primary anaerobic isolation. The organism also grows well on CNA and Brucella agar.
What is the major pathogen for actinomycosis?
The major human pathogen for actinomycosis, A. israelii,was identified in two patients in 1878 and fully delineated by Israel (5). In 1891, Wolff and Israel (6) described the cultural characteristics and its anaerobic growth. Since then, studies have identified A. naeslundii, A. viscosus, A. pyogenes, A denticolens, A. howellii, A. hordeovulneris,and A. meyeriin humans as well as in dogs and cats. Actinomycosis is the most common infectious disease of kangaroos (7).
Where was Actinomycosis discovered?
Actinomycosis is a disease of antiquity, having most likely infected the jaw of a fossil rhinoceros ( 1) and the ribs of a man discovered in southeastern Ontario, Canada, who by radiocarbon dating lived 230 A.D. + 55 ( 2 ). In 1877, Bollinger and Harz ( 3) named the genus Actinomyces when they described the etiologic agent of bovine actinomycosis ...
How often is doxycycline given?
Because of a penicillin allergy, 1 g of doxycycline was given intravenously to the patient every 12 hours for 2 weeks. Follow-up blood cultures were sterile. The patient’s dental health appeared normal and no source for the bacteremia was identified. The patient entered complete remission.
How long does it take for a blood agar to show red?
On blood agar, the bacteria develop as small, irregular, whitish colonies that are smooth to slightly granular and show a dark red pigment when mature (2–14 days). This pigmentation is most obvious when the cultures are left standing in air at room temperature after primary anaerobic isolation.
What is an actinomyce?
Actinomyces are fastidious, obligate anaerobic, gram-positive, slow-growing bacilli. These features make Actinomyces difficult to identify using routine specimen handling and culture techniques. If these organisms are to be cultured, an anaerobic swab is required as exposure to oxygen, even briefly, is often enough to kill anaerobic organisms. (For example; an IUD received in a sterile container is surrounded by oxygen, and consequently anaerobic culture cannot be performed.) Additionally, even if an appropriately anaerobic specimen (such as a blue top anaerobic gel swab) is used in attempt to culture Actinomyces vaginally, the other resident anaerobic flora will compete with the slow-growing Actinomyces, which therefore will not be detected.
Can actinomyces be found in the female genital tract?
Actinomyces may colonize the female genital tract and be present in polymicrobial pelvic abscesses—and while IUD-associated actinomycosis has been reported, case reporting is poor and therefore there are no clear statistics regarding the total number of cases. It is therefore impossible to give an accurate risk of occurrence; however, these abscesses are generally regarded as exceedingly rare.
Is a Pap test positive for Actinomyces?
Actinomyces-like organisms are seen on an average of 7% of Pap tests, which is clearly far greater than the prevalence of these (rare) abscesses. Therefore, the Pap test has a high false-positive rate and an extremely low positive predictive value for Actinomyces related disease. Sensitivity of the Pap test for Actinomyces is also poor; even among women with actinomycotic abscesses, only half of these had a Pap test that was positive for Actinomyces.
Is Actinomyces a pathogen?
Actinomyces are present as comme nsal organisms in healthy humans and are best thought of as opportunistic pathogens. Therefore, the mere presence of Actinomyces is not diagnostic of disease. (This is also why no molecular test exists for Actinomyces.)
Overview
Actinomyces is a genus of the Actinomycetia class of bacteria. They all are gram-positive. Actinomyces species are facultatively anaerobic (except A. meyeri and A. israelii are obligate anaerobes), and they grow best under anaerobic conditions. Actinomyces species may form endospores, and while individual bacteria are rod-shaped, Actinomyces colonies form fungus-like branched netw…
Genomics
Phylogenetic trees based on 16S ribosomal RNA (16SrRNA) sequences have shown that the genus Actinomyces is quite diverse, exhibiting polyphyletic branching into several clusters. The genera Actinomyces and Mobiluncus form a monophyletic clade in a phylogenetic tree constructed using RpoB, RpoC, and DNA gyrase B protein sequences. This clade is also strongly supported by a conserved signature indel consisting of a three-amino-acid insertion in isoleucine tRNA synthetase found …
Pathology
Actinomycota are normally present in the gums, and are the most common cause of infection in dental procedures and oral abscesses. Many Actinomyces species are opportunistic pathogens of humans and other mammals, particularly in the oral cavity. In rare cases, these bacteria can cause actinomycosis, a disease characterized by the formation of abscesses in the mouth, lungs, or the gastrointestinal tract. Actinomycosis is most frequently caused by A. israelii, which may al…
Diagnosis
Actinomycosis may be considered when a patient has chronic progression of disease across tissue planes that is mass-like at times, sinus tract development that may heal and recur, and refractory infection after a typical course of antibiotics.
Treatment
Treatment for actinomycosis consists of antibiotics such as penicillin or amoxicillin for 5 to 12 months, as well as surgery if the disease is extensive.
Species
The genus Actinomyces comprises the following species:
• "A. actinomycetemcomitans" Iinuma et al. 1994
• "A. bouchesdurhonensis" Fonkou et al. 2018
• A. bovis Harz 1877 (Approved Lists 1980)
Gallery
• Micrograph of actinomycosis, H&E stain
• Micrograph of actinomycosis, GMS stain
• Micrograph of actinomycosis, Gram stain
External links
• Actinomyces naeslundii MG1 Genome Page
• Actinomyces at BacDive - the Bacterial Diversity Metadatabase