This test looks for certain bacteria in a wound or an infection in a fluid sample. These bacteria are called anaerobic because they don't need oxygen to grow. Infections caused by anaerobic bacteria can occur almost anywhere in your body. These may be oral infections, lung infections,...
When is anaerobic culture used?
Anaerobic cultures are indicated particularly when suspected infections are related to gastrointestinal tract, pelvic organs, associated with malignancy, related to use of aminoglycosides, or occur in a setting in which the diagnosis of gas gangrene or actinomycosis is considered.
What can anaerobic bacteria cause?
Infections like tetanus and gangrene are caused by anaerobic bacteria. Anaerobic infections typically cause abscesses (buildups of pus), and death of tissue. Many anaerobic bacteria produce enzymes that destroy tissue or sometimes release potent toxins. Besides bacteria, some protozoans and worms are also anaerobic.
Why is anaerobic culture important?
Anaerobic blood culture may be most helpful when (1) bacteremia because of obligate anaerobes is clinically suspected, (2) patients are severely immunocompromised, and (3) source of bacteremia is not identified by clinical evaluation.
What are examples of anaerobic infections?
Anaerobic organ infections include, but are not restricted to, brain abscesses, dental infections, aspiration pneumonia, lung abscesses, bite infections (animal/human), abdominal abscesses, and necrotizing infections of soft tissue.
How do you catch anaerobic infection?
Anaerobic infections can happen when deep tissues become injured or exposed. This can occur due to trauma or surgery, such as animal bites or root canals. Your risk is higher if you have: low blood supply.
What antibiotic kills anaerobic bacteria?
The third-generation cephalosporins are usually less active than cefoxitin against the B fragilis group. Drugs active against essentially all Gram-negative (and other) anaerobes are metronidazole, imipenem, chloramphenicol, and combinations of β-lactam drugs plus a β-lactamase inhibitor.
Do anaerobic bacteria cause UTI?
The majority of bacterial urinary tract infections (UTI) are caused by groups of Gram-negative aerobic or facultative anaerobic bacilli, which include Escherichia, Klebsiella, Aerobacter, Proteus and Pseudomonas spp.
What if culture report is positive?
If the blood culture is positive, this means you have a bacterial or yeast infection in your blood. The results usually help your doctor identify the specific bacteria or fungi that's causing the infection.
Where do anaerobic bacteria live and what can they cause?
Anaerobic bacteria are bacteria that do not live or grow when oxygen is present. In humans, these bacteria are most commonly found in the gastrointestinal tract. They play a role in conditions such as appendicitis, diverticulitis, and perforation of the bowel.
Where are anaerobic bacteria found in the body?
gastrointestinal tractAnaerobic bacteria are bacteria that do not live or grow when oxygen is present. In humans, these bacteria are most commonly found in the gastrointestinal tract. They play a role in conditions such as appendicitis, diverticulitis, and perforation of the bowel.
What is an anaerobic bacterial infection?
Anaerobic infections are caused by anaerobic bacteria. Obligately anaerobic bacteria do not grow on solid media in room air (0.04% carbon dioxide and 21% oxygen); facultatively anaerobic bacteria can grow in the presence or absence of air.
How do you get rid of anaerobic bacteria?
The most effective antimicrobials against anaerobic organisms are metronidazole, the carbapenems (imipenem, meropenem and ertapenem), chloramphenicol, the combinations of a penicillin and a beta-lactamase inhibitor (ampicillin or ticarcillin plus clavulanate, amoxicillin plus sulbactam, and piperacillin plus tazobactam ...
Which disease is caused by aerobic bacteria?
Infections can occur in the root canals, gums (gingivitis), jaw, tonsils, throat, sinuses, and ears. Lung. Anaerobic bacteria can cause pneumonia, lung abscesses, infecton of the lining of the lung (empyema), and dilated lung bronchi (bronchiectasis). Intraabdominal.
Is UTI caused by anaerobic bacteria?
The majority of bacterial urinary tract infections (UTI) are caused by groups of Gram-negative aerobic or facultative anaerobic bacilli, which include Escherichia, Klebsiella, Aerobacter, Proteus and Pseudomonas spp.
What does it mean if a bacteria is anaerobic?
Anaerobic bacteria are bacteria that do not live or grow when oxygen is present. In humans, these bacteria are most commonly found in the gastrointestinal tract.
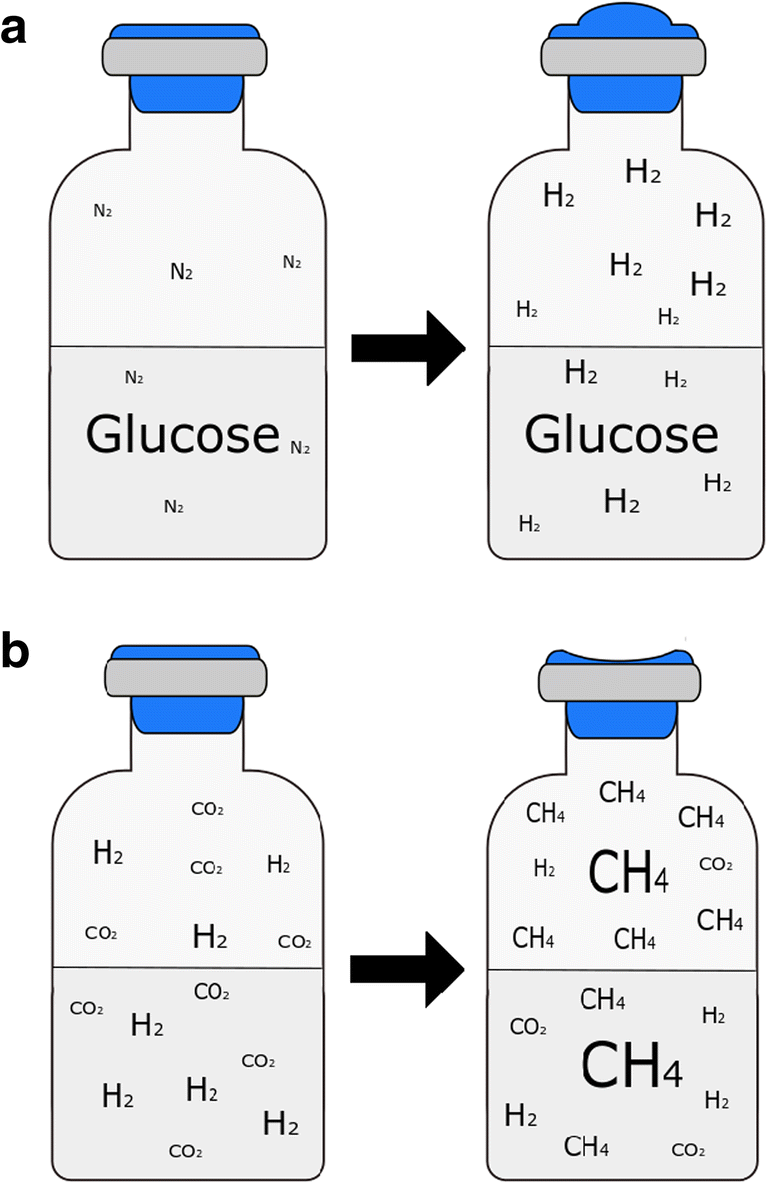
What gas does anaerobic bacteria produce?
BiogasBiogas is generated during anaerobic digestion when microorganisms break down (eat) organic materials in the absence of air (or oxygen). Biogas is mostly methane (CH4) and carbon dioxide (CO2), with very small amounts of water vapor and other gases.
How is this test done?
This test requires a sample of fluid or tissue from your wound or sore. Your healthcare provider may use a cotton swab to get the sample. Or he or she may use a needle to draw fluid from your wound.
What is this test?
This test looks for certain types of bacteria in a wound or a fluid sample from an infection site. These bacteria are called anaerobic because they don't need oxygen to grow. An anaerobic culture means the test is done without letting oxygen get to the sample.
Why do I need this test?
You may have this test if your healthcare provider needs to find out the type of bacteria that's causing an infection in your body. Your provider may order this test based on wound location , tissue damage, an unpleasant smelling wound, or a sore related to the infection.
What other tests might I have along with this test?
Your healthcare provider may also order other tests, depending on your symptoms. These tests may include:
What do my test results mean?
Many things may affect your lab test results. These include the method each lab uses to do the test. Even if your test results are different from the normal value, you may not have a problem. To learn what the results mean for you, talk with your healthcare provider.
What might affect my test results?
This means you may have a false-negative result. Anaerobic bacteria picked up in the sample that are present in the area of the infection but are not causing the infection can also affect your results.
What is anaerobic culture?
Anaerobic cultures are indicated particularly when suspected infections are related to gastrointestinal tract, pelvic organs, associated with malignancy, related to use of aminoglycosides, or occur in a setting in which the diagnosis of gas gangrene or actinomycosis is considered. Anaerobic culture is especially indicated when an exudate has a foul odor or if the exudate has a grayish discoloration and is hemorrhagic. Frequently, more than one organism is recovered from an anaerobic infection.
What is the ratio of anaerobes to facultative species?
The ratio of anaerobes to facultative species is normally about 10:1 in the mouth, vagina, and sebaceous glands and at least 1000:1 in the colon. Biopsy culture is particularly useful in establishing the diagnosis of anaerobic osteomyelitis, 2 clostridial myonecrosis, intracranial actinomycosis, and pleuropulmonary infections.
How long do anaerobes live?
Under these conditions, aerobes and anaerobes will survive 24 to 72 hours when properly collected in the anaerobic transport tube.
What is anaerobic infection?
Anaerobic infection is most commonly associated with operations involving opening or manipulating the bowel or a hollow viscus (eg, appendectomy, cholecystectomy, colectomy, gastrectomy, bile duct exploration, etc.).
Can you use aspirates for Gram staining?
Aspirates are preferable to swabs. A thin smear for Gram stain obtained from the same site is strongly recommended and must be ordered separately. Culture samples must be collected to avoid contamination with indigenous anaerobic flora from skin and mucous membranes.
Is it ok to culture a bronchoscopic specimen?
Bronchoscopically obtained specimens are not ideal as the instrument becomes contaminated by organisms normally contaminating the oropharynx during insertion. Culture of specimens from sites harboring endogenous anaerobic organisms or contaminated by endogenous organisms may be misleading with regard to etiology and selection of appropriate therapy.
Can a blood culture be positive?
Blood culture s yield positive results in less than five percent of cases of anaerobic pulmonary infection. Specimens received in anaerobic transport containers are not optimal for aerobic fungus cultures. Mycobacterium sp or Nocardia sp, which may cause abscesses, will not be recovered even if present, since extended incubation periods, ...
When to use anaerobic cultures?
Anaerobic cultures are indicated particularly when suspected infections are related to gastrointestinal tract, pelvic organs, associated with malignancy, related to use of aminoglycosides; or occur in a setting in which the diagnosis of gas gangrene or actinomycosis is considered.
What sites are inappropriate for anaerobic cultures?
Because of resident anaerobic flora, the following sites are inappropriate for anaerobic cultures and will be rejected: throat and nasopharynx, sputum, bronchoscopy specimens, gastrointestinal contents, voided or catheterized urine, urogenital swabs (eg, vaginal and/or cervical), and specimens from superficial wounds.
What are anaerobic and aerobes?
In open wounds, anaerobic organisms may play an etiologic role, whereas aerobes may represent superficial contamination. Serious anaerobic infections are often due to mixed flora, which are pathologic synergists. Anaerobes frequently recovered from closed postoperative wound infections include Bacteroides fragilis, approximately 50%; Prevotella melaninogenica, approximately 25%; Peptostreptococcus prevotii, approximately 15%; and Fusobacterium sp, approximately 25%. Anaerobes are seldom recovered in pure culture (10% to 15% of cultures). Aerobes and facultative bacteria when present are frequently found in lesser numbers than the anaerobes. Anaerobic infection is most commonly associated with operations involving opening or manipulating the bowel or a hollow viscus (eg, appendectomy, cholecystectomy, colectomy, gastrectomy, bile duct exploration, etc). The ratio of anaerobes to facultative species is normally about 10:1 in the mouth, vagina, and sebaceous glands and at least 1000:1 in the colon. Biopsy culture is particularly useful in establishing the diagnosis of anaerobic osteomyelitis, 2 clostridial myonecrosis, intracranial actinomycosis, and pleuropulmonary infections. Anaerobic infections of soft tissue include anaerobic cellulitis, necrotizing fasciitis, clostridial myonecrosis (gas gangrene), anaerobic streptococcal myositis or myonecrosis, synergistic nonclostridial anaerobic myonecrosis, and infected vascular gangrene. These infections, particularly clostridial myonecrosis, necrotizing fasciitis, and nonclostridial anaerobic myonecrosis, may be fulminant and are frequently characterized by the presence of gas and foul-smelling necrotic tissue. 3 Empiric therapy based on likely pathogens should be instituted as soon as appropriate cultures are collected.
What is the ratio of anaerobes to facultative species?
The ratio of anaerobes to facultative species is normally about 10:1 in the mouth, vagina, and sebaceous glands and at least 1000:1 in the colon. Biopsy culture is particularly useful in establishing the diagnosis of anaerobic osteomyelitis, 2 clostridial myonecrosis, intracranial actinomycosis, and pleuropulmonary infections.
What is anaerobic transport?
Anaerobic transports must be used for swabs and for aspirates. Specimens are to be collected from a prepared site using sterile technique. Contamination with normal flora from skin, rectum, vaginal tract, or other body surfaces must be avoided.
How long can anaerobes survive in an ESWAB?
Under these conditions, anaerobes will survive 24 to 72 hours when properly collected in the anaerobic transport tube. Storage of specimens in the ESwab™ transport at room temperature for greater than 48 hours may result in diminished recovery of certain anaerobic species.
What is anaerobic infection?
Anaerobic infection is most commonly associated with operations involving opening or manipulating the bowel or a hollow viscus (eg, appendectomy, cholecystectomy, colectomy, gastrectomy, bile duct exploration, etc).
What are some specimens that are not suitable for anaerobic culture?
Specimens that are NOT suitable for anaerobic culture: Saliva. Vaginal or cervical specimens. Feces (unless looking for a particular Clostridial pathogen) Tracheal swabs. Naso- tracheal aspirates . Colostomy or ileostomy effluents. Skin or superficial wound swabs. Urine.
What are the clinical conditions suggestive of anaerobic infections?
Clinical Conditions suggestive of anaerobic infections: Deep infections from penetration of cutaneous or mucosal surfaces. Necrotic tissue, gangrene, pseudo membrane formation. Infection associated with malignancy or other disease causing tissue destruction and impaired circulation.
How big should a tissue specimen be for a sterile tube?
Tissue specimens: Tissue specimens should be >2-3 cm in diameter.
How to avoid shocking anaerobes?
It is important to avoid shocking the anaerobes by exposing them to oxygen or allowing the sample to become dry. The following guidelines can be used to determine when it is appropriate to choose an ANAEROBIC culture.
What is the preferred swab for pyometra?
Septic processes such as pyometra. The Clinical Microbiology Laboratory accepts swabs, tissue and fluid samples. If swabs are submitted, the preferred swab is the eSwab™. These eSwabs™ are acceptable swabs for aerobic, anaerobic, Mycoplasma and fungal culture and can be used for other laboratory testing as well.
Clinical Significance
Deep wound/abscess infections are often caused by a mixture of aerobic and anaerobic bacteria.
Test Details
Culture, Aerobic Bacteria and Culture, Anaerobic Bacteria with Gram Stain
What is anaerobic culture?
Anaerobic culture is especially indicated when an exudate has a foul odor or if the exudate has a grayish discoloration and is hemorrhagic. Frequently, more than one organism is recovered from an anaerobic infection.
How long can anaerobic culture be stored?
Under these conditions, aerobes and anaerobes will survive 24 to 72 hours when properly collected in the anaerobic transport tube. Storage of specimens in the ESwab™ transport at room temperature for greater than 48 hours may result in diminished recovery of certain anaerobic species.
What are anaerobic and aerobes?
In open wounds, anaerobic organisms may play an etiologic role, whereas aerobes may represent superficial contamination. Serious anaerobic infections are often due to mixed flora that are pathologic synergists. Anaerobes frequently recovered from closed postoperative wound infections include Bacteroides fragilis, approximately 50%; Prevotella melaninogenica, approximately 25%; Peptostreptococcus prevotii, approximately 15%; and Fusobacterium sp, approximately 25%. Anaerobes are seldom recovered in pure culture (10% to 15% of cultures). Aerobes and facultative bacteria when present are frequently found in lesser numbers than the anaerobes. Anaerobic infection is most commonly associated with operations involving opening or manipulating the bowel or a hollow viscus (eg, appendectomy, cholecystectomy, colectomy, gastrectomy, bile duct exploration, etc). The ratio of anaerobes to facultative species is normally about 10:1 in the mouth, vagina, and sebaceous glands and at least 1000:1 in the colon. Biopsy culture is particularly useful in establishing the diagnosis of anaerobic osteomyelitis, 2 clostridial myonecrosis, intracranial actinomycosis, and pleuropulmonary infections. Anaerobic infections of soft tissue include anaerobic cellulitis, necrotizing fasciitis, clostridial myonecrosis (gas gangrene), anaerobic streptococcal myositis or myonecrosis, synergistic nonclostridial anaerobic myonecrosis, and infected vascular gangrene. These infections, particularly clostridial myonecrosis, necrotizing fasciitis, and nonclostridial anaerobic myonecrosis, may be fulminant and are frequently characterized by the presence of gas and foul-smelling necrotic tissue. 3 Empiric therapy based on likely pathogens should be instituted as soon as appropriate cultures are collected.
How to obtain a lower respiratory sample?
Lower respiratory samples must be obtained by transtracheal percutaneous needle aspiration, transbronchial biopsy, transthoracic needle biopsy, or open lung biopsy by physicians trained in these procedures. If swabs must be used, collect two, use one for Gram stain and one for culture. Anaerobic transports must be used for swabs and for aspirates.
What sites are inappropriate for anaerobic cultures?
Because of resident anaerobic flora, the following sites are inappropriate for anaerobic cultures and will be rejected: throat and nasopharynx, sputum, bronchoscopy specimens, gastrointestinal contents, voided or catheterized urine, urogenital swabs (eg, vaginal and/or cervical), and specimens from superficial wounds.
What is the ratio of anaerobes to facultative species?
The ratio of anaerobes to facultative species is normally about 10:1 in the mouth, vagina, and sebaceous glands and at least 1000:1 in the colon. Biopsy culture is particularly useful in establishing the diagnosis of anaerobic osteomyelitis, 2 clostridial myonecrosis, intracranial actinomycosis, and pleuropulmonary infections.
How to kill anaerobes?
Some anaerobes will be killed by contact with molecular oxygen for only a few seconds. Overlying and adjacent areas must be carefully disinfected to eliminate contamination with indigenous flora. Ideally, pus or other fluid obtained by needle aspiration through intact skin or mucosal surface that has been cleaned with antiseptic should be collected. Sampling of open lesions is enhanced by deep aspiration using a sterile plastic catheter. Curettings of the base of an open lesion are optimal. If irrigation is necessary, nonbacteriostatic sterile normal saline may be used. Lower respiratory samples must be obtained by transtracheal percutaneous needle aspiration, transbronchial biopsy, transthoracic needle biopsy, or open lung biopsy by physicians trained in these procedures. If swabs must be used, collect two, use one for Gram stain and one for culture. Anaerobic transports must be used for swabs and for aspirates. Specimens are to be collected from a prepared site using sterile technique. Contamination with normal flora from skin, rectum, vaginal tract, or other body surfaces must be avoided.
