
Full Answer
What does mechanical ventilation stand for?
Mechanical ventilation, assisted ventilation or intermittent mandatory ventilation (IMV), is the medical term for using a machine called a ventilator to fully or partially provide artificial ventilation. Mechanical ventilation helps move air into and out of the lungs, with the main goal of helping the delivery of oxygen and removal of carbon ...
What are the different types of mechanical ventilation?
Volume Modes
- Assist-Control Ventilation (ACV) Also known as continuous mandatory ventilation (CMV). ...
- Synchronized Intermittent-Mandatory Ventilation (SIMV) Guarantees a certain number of breaths, but unlike ACV, patient breaths are partially their own, reducing the risk of hyperinflation or alkalosis.
- ACV vs. ...
What is the purpose of mechanical ventilation?
- Used as a primary means of mechanical ventilation
- Used in patients who have respiratory patterns that use asynchronous with the control mode
- Used in patients who hyperventilate on the assist/control mode
- Used in patients who require some respiratory support but are able to breathe spontaneously
What does mechanical ventilation mean?
Mechanical ventilation, or assisted ventilation, is the medical term for artificial ventilation where mechanical means are used to assist or replace spontaneous breathing. Face or nasal masks are used for non-invasive ventilation in appropriately selected conscious patients. Click to see full answer.
What is considered mechanical ventilation?
Mechanical Ventilation. Mechanical ventilation is a form of life support. A mechanical ventilator is a machine that takes over the work of breathing when a person is not able to breathe enough on their own. The mechanical ventilator is also called a ventilator, respirator, or breathing machine.
What is an example of mechanical ventilation?
The common method is by insertion of a tube into the trachea. Intubation, which provides a clear route for the air can be either an endotracheal tube, inserted through the natural openings of mouth or nose, or a tracheostomy inserted through an artificial opening in the neck.
What is the purpose of mechanical ventilation?
Mechanical ventilation is use of a machine to assist with the work of breathing. Mechanical ventilators are frequently used for conditions that cause either low oxygen levels (such as pneumonia) or high carbon dioxide levels (such as chronic obstructive pulmonary disease).
How long can you be on a mechanical ventilator?
How long does someone typically stay on a ventilator? Some people may need to be on a ventilator for a few hours, while others may require one, two, or three weeks. If a person needs to be on a ventilator for a longer period of time, a tracheostomy may be required.
What are the 4 types of mechanical ventilation?
Basic Modes of Mechanical VentilationA/C, VCV - Assisted/Controlled, Volume Cycled Ventilation.A/C, PCV - Assisted/Controlled, Pressure Controlled Ventilation (time cycled)SIMV - Synchronized Intermittent Mandatory Ventilation.PSV - Pressure Support Ventilation.
What are the three types of mechanical ventilation?
Understanding the 3 Types of Mechanical VentilationExhaust-only ventilation. This ventilation type uses a fan to move indoor air out of your home, while outdoor air is drawn in through leaks. ... Supply-only ventilation. ... Balanced ventilation.
What does it mean when someone is breathing over the ventilator?
During a severe illness. Sometimes, a person who is very ill becomes too weak to breathe well enough to provide enough oxygen to the brain and body. A ventilator can do the work of breathing for them, allowing their body to rest and recover.
What are the two types of mechanical ventilation?
There are two primary types of mechanical ventilation: negative pressure ventilation (NPV) and positive pressure ventilation (PPV). Negative pressure ventilation exposes the thorax to sub-atmospheric pressure, which causes breathing by sucking air into the lungs.
What is it called when they put you on a ventilator?
You may be put on a mechanical ventilator, also known as a breathing machine, if a condition makes it very difficult for you to breathe or get enough oxygen into your blood. This condition is called respiratory failure.
Is a ventilator considered life support?
Types of Life Support When most people talk about a person being on life support, they're usually talking about a ventilator, which is a machine that helps someone breathe. A ventilator keeps oxygen flowing throughout the body by pushing air into the lungs.
What is the life expectancy of someone on a ventilator?
In general, most patients did not survive longer than 1 to 3 years, although some patients did exhibit a longer survival time. All patients survived the initial 21 days of treatment by mechanical ventilation, and the survival times reported here exclusively refer to survival duration thereafter.
How serious is being put on a ventilator?
When using a ventilator, you may need to stay in bed or use a wheelchair. This raises your risk of blood clots, serious wounds on your skin called bedsores, and infections. Fluid can build up in the air sacs inside your lungs, which are usually filled with air. This is called pulmonary edema.
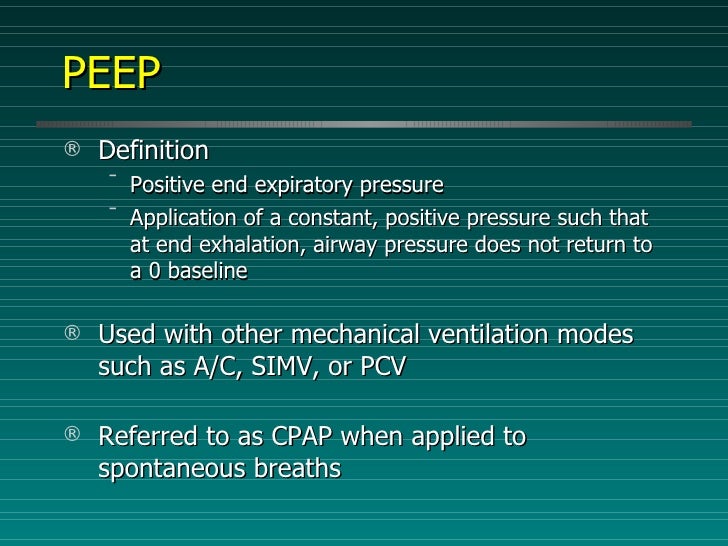
Is CPAP mechanical ventilation?
One type of non-invasive mechanical ventilation is called CPAP (continuous positive airway pressure) and another is called BiPAP (bi-level positive airway pressure). Invasive mechanical ventilation uses a machine to push air and oxygen into your lungs through a tube in your windpipe.
What is a mechanical ventilation in nursing?
A mechanical ventilator is a machine that helps a patient breathe (ventilate) when he or she cannot breathe on his or her own for any reason. There are many benefits, but a major risk is infection.
What are the 2 types of ventilators?
There are different types of ventilator, including noninvasive and invasive, that provide varying degrees of support. Demand for ventilators has increased due to COVID-19.
Is mechanical ventilation the same as intubation?
Definition. Intubation is placing a tube in your throat to help move air in and out of your lungs. Mechanical ventilation is the use of a machine to move air in and out of your lungs.
What Is A Mechanical Ventilator?
A mechanical ventilator is a machine that helps a patient breathe (ventilate) when he or she is recovering from surgery or critical illness, or can...
Why Do We Use Mechanical Ventilators?
A mechanical ventilator is mainly used to make it easier for very sick people to breathe. Another reason is to help raise the oxygen level for thes...
What Are The Benefits of Mechanical Ventilation?
The main benefits of mechanical ventilation are the following: 1. The patient doesn’t have to work as hard to breathe; 2. The patient's breathing h...
What Are The Risks of Mechanical Ventilation?
The main risk of mechanical ventilation is infection, as the artificial airway may allow germs to enter the lung. Another risk factor is lung damag...
What Procedures Can Help A Patient With An Artificial Airway Connected to A Mechanical Ventilator?
1. Suctioning: This is a procedure in which a catheter (a thin, hollow tube) is inserted into the breathing tube to help remove secretions and wast...
How Long Does The Patient Stay Connected to The Mechanical Ventilator?
The main purpose for using a mechanical ventilator is to allow the patient time to heal. Usually, as soon as a patient can breathe effectively on h...
Who Are The Caregivers Who Take Care of The Patient on A Mechanical Ventilator?
1. Physician: The physician is usually an anesthesiologist, pulmonologist, intensivist, or critical care physician. These doctors have special trai...
When should mechanical ventilation be considered?
There are numerous indications for endotracheal intubation and mechanical ventilation (see table Situations Requiring Airway Control ), but, in general, mechanical ventilation should be considered when there are clinical or laboratory signs that the patient cannot maintain an airway or adequate oxygenation or ventilation.
What is the pressure gradient in mechanical ventilation?
In mechanical ventilation, the pressure gradient results from increased (positive) pressure of the air source.
How much inspiratory flow should I use for a patient?
The inspiratory flow should generally be set at about 60 L/minute but can be increased up to 120 L/minute for patients with airflow limitation to facilitate having more time in exhalation, thereby limiting autoPEEP.
Where does resistance to airflow occur?
In the mechanically ventilated patient, resistance to airflow occurs in the ventilator circuit, the endotracheal tube, and, most importantly, the patient’s airways. (NOTE: Even when these factors are constant, an increase in airflow increases resistive pressure.)
What is pressure cycled?
Pressure cycled: Delivering constant pressure during each breath (volume delivered may vary) A combination of volume and pressure cycled. Assist-control (A/C) modes of ventilation are modes that maintain a minimum respiratory rate regardless of whether or not the patient initiates a spontaneous breath.
Should mechanical ventilation be delayed?
However, mechanical ventilation should not be delayed until the patient is in extremis.
Is airway pressure fixed?
The resultant airway pressure is not fixed but varies with the resistance and elastance of the respiratory system and with the flow rate selected.
Why do we need ventilators?
Why is a Ventilator Needed? Brain and Spinal Cord Injury or Disease: An injury or disease to the brain can interfere with the signals that control breathing. Damage to the spinal cord can block the brain’s signals from reaching the breathing muscles. Disorders of the Muscles: Can weaken the breathing muscles or change the way in which they receive ...
Why is it important to heat and humidify the air delivered from a ventilator?
It is important to heat and humidify the air delivered from a ventilator. Dry, cold air can damage the delicate tissues of the airways and cause mucus plugs. Heat and humidity can be delivered in 2 different ways:
Why does my ventilator alarm sound?
High pressure alarm: This will sound when the pressure in the circuit has increased. It helps protect the lungs from high pressures delivered from the ventilator. Secretions, water in the tubing, or kinks in the tubing can cause high pressure. Suction the patient and look for other sources. If this does not fix the problem, disconnect the patient from the circuit and manually ventilate with an AMbu bag. Then call for help.
How does a ventilator deliver air?
The ventilator will deliver the breath in 2 different ways: Volume: The ventilator delivers a pre-set volume of air with every breath. Pressure: The ventilator will deliver a breath until a pre-set pressure is reached.
What happens when a ventilator is full?
Once the lungs are full, the vent stops pushing the air into the lungs. The air then passively leaves the lungs. This is similar to letting air out of a full balloon. Settings are selected when a patient is placed on a ventilator. These settings are different for every patient depending on their needs.
How often should a ventilator be checked?
Patient monitoring and ventilator checks are generally performed every 4 hours in the hospital. This is important to guarantee proper ventilator function and to know if there is a patient issue. Such as:
What outlet do you plug a ventilator into?
In the hospital, the ventilator will always be plugged into a red electrical outlet. If the hospital loses power, the red outlets are connected to a backup generator.
Are we missing a good definition for mechanical ventilation? Don't keep it to yourself..
The ASL fingerspelling provided here is most commonly used for proper names of people and places; it is also used in some languages for concepts for which no sign is available at that moment.
Definitions & Translations
Get instant definitions for any word that hits you anywhere on the web!
What are the characteristics of ventilatory modes?
While modes have classically been divided up into pressure or volume controlled modes, a more modern approach describes ventilatory modes based on three characteristics – the trigger (flow versus pressure), the limit (what determines the size of the breath), and the cycle (what actually ends the breath). In both VCV and PCV, time is the cycle, the difference being in how the time to cessation is determined. PSV, by contrast, has a flow cycle.
What is inverse ratio ventilation?
Inverse Ratio Ventilation (IRV) is a subset of PCV in which inflation time is prolonged ( In IRV, 1:1 , 2:1, or 3:1 may be use . Normal I:E is 1:3). This lowers peak airway pressures but increases mean airway pressures. The result may be improved oxygenation but at the expense of compromised venous return and cardiac output, thus it is not clear that this mode of ventilation leads to improved survival. IRV’s major indication is in patients with ARDS with refractory hypoxemia or hypercapnia in other modes of ventilation [Am J Surg 183: 151, 2002]
What is APRV in CPAP?
Airway pressure release ventilation is similar to PCIRV – instead of being a variation of PCV in which the I:E ratio is reversed, APRV is a variation of CPAP that releases pressure temporarily on exhalation. This unique mode of ventilation results in higher average airway pressures. Patients are able to spontaneously ventilate at both low and high pressures, although typically most (or all) ventilation occurs at the high pressure. In the absence of attempted breaths, APRV and PCIRV are identical. As in PCIRV, hemodynamic compromise is a concern in APRV. Additionally, APRV typically requires increased sedation
What is pressure controlled ventilatory mode?
Pressure controlled ventilatory mode in which the majority of time is spent at the higher (inspiratory) pressure. Early trials were promising, however the risks of auto PEEP and hemodynamic deterioration due to the decreased expiratory time and increased mean airway pressure generally outweight the small potential for improved oxygenation
What is a CMV breath?
Also known as continuous mandatory ventilation (CMV). Each breath is either an assist or control breath, but they are all of the same volume. The larger the volume, the more expiratory time required. If the I:E ratio is less than 1:2, progressive hyperinflation may result.
What is PAV in ventilators?
During PAV, the clinician sets the percentage of work of breathing to be provided by the ventilator. PAV uses a positive feedback loop to accomplish this, which requires knowledge of resistance and elastance to properly attenuate the signal
Should patients who breathe rapidly on ACV switch to SIMV?
Patients who breathe rapidly on ACV should switch to SIMV 2. Patients who have respiratory muscle weakness and/or left-ventricular dysfunction should be switched to ACV
How to calculate minute ventilation?
Minute Ventilation = volume of gas breathed in one minute = tidal volume multiplied by respiratory rate.
What happens to intrapleural pressure during mechanical ventilation?
The fall in intrapleural pressure facilitates movement of gases into and out of the lungs and importantly also improves venous return to the heart. During positive pressure ventilation, which is what occurs during mechanical ventilation, the mean intrathoracic pressure is usually positive. So the pressure increases during inhalation ...
What is a shunt in a lungs?
This occurs in the lungs when the blood passes through from the right side of the heart to the left side without participating in gas exchange. Hypoxemia is the outcome of such a shunt.
What is positive pressure ventilation?
Firstly, during inspiration, it can exceed alveolar opening pressure which helps to recruit otherwise collapsed, and therefore non-functioning, alveoli which in turn will improve oxygenations.
What is mechanical dead space?
Mechanical dead space refers to the ventilator circuit and the rebreathed gases that this causes. The conducting part of the lungs i.e. trachea, bronchus, bronchioles, and terminal bronchioles, play no part in gas exchange and amount to about 150mls. This is the anatomic dead space.
Why is PEEP used in lung ventilation?
Use of PEEP to maintain lung volumes is effective in preventing atelectasis. Ventilator Induced Lung Injury.
Does positive pressure ventilation cause hypoxemia?
Positive pressure ventilation can, however, increase pulmonary vascular resistance which can increase blood flow through an anatomic shunt thereby decreasing blood flow through the lungs and worsening hypoxemia. So one needs to be cautious when there is an anatomic shunt present.
What is the difference between mechanical ventilation and intubation?
Intubation places a tube in the throat to help move air in and out of the lungs. Mechanical ventilation is the use of a machine to move the air in and out of the lungs.
How long does it take to put a ventilator in?
It will take less 5 minutes to put the breathing tube in. How long the ventilator is used depends on the reason why it is needed.
Why do people breathe during surgery?
Reasons for Procedure. This is often done in an emergency to help a person breathe. Breathing problems may be due to an injury or illness. It may also be done during surgery. Anesthesia can cause breathing problems.
How to make sure air is moving to both lungs?
Listen to the lungs to make sure air is moving to both lungs. Do a chest x-ray to make sure the tip of the tube is in the right place. Measure the level of gases in the blood to make sure enough air is moving.
How does a breathing tube work?
The scope will be removed. The tube will be secured. A flexible tube will be attached to the breathing tube and connected to a ventilator machine. The machine will move air in and out of the lungs.
What is pressure controlled ventilation?
Pressure controlled ventilation is when a patient has a pressure setting on the ventilator and when the ventilator cycles a breath the pressure will continue to rise on the ventilator until the pre-set pressure limit is reached then the ventilator will cycle off and the patient will then exhale.
What is the respiration mode on a ventilator?
This mode requires a frequency of respirations per minute to be set. Patients who are attached to the ventilator then can trigger additional breaths that are greater than the set respirations per minute. If these patients cannot meet the trigger criteria, then the machine takes over and triggers all of the breaths.
What happens if a ventilator does not initiate inspiration?
If the patient does not initiate inspiration, the ventilator automatically delivers the preset rate and tidal volume. This is to ensure minimum minute ventilation is achieved. Some ventilator settings are common between conventional modes of ventilation.
When using assist control modes, should the respiratory rate be set at least high enough?
When using assist control modes, the respiratory rate should be set at least high enough so as to achieve a minute ventilation that is predicted for the patient. The respiratory rate can be set even higher if the patient has a known acid base imbalance during the time of intubation.
