What is a SOAP format in massage therapy?
The SOAP format provides clinicians an organized structure to document the most important parts of a client / patient encounter. SOAP notes are a format for medical charting that have been around since the 1960’s and it is currently one of the most widely used methods of documenting massage therapy sessions.
What does soap mean in medical terms?
Patient records A standard format for physician charting of Pt exams on a problem-based Pt record; SOAP combines patient complaints and physician determinations. See Hospital chart, Medical record.
What should a massage therapist write in a SOAP note?
Client’s self-care plan (stretches, exercises, heat or cold recommendations, etc.) A common error that massage therapists make in the plan section of a SOAP note is writing a vague plan like “Continue treatment”. Here is a SOAP note example for a massage session, to further demonstrate what kind of information goes in each section.
What is the objective of a soap test?
In the objective section of the SOAP notes, the therapist records height, weight and body mass index data indicating that the client is obese. They perform some range of motion tests to measure the client’s ability to bend and turn from the waist without pain, recording the results.

What is SOAP notes for massage?
SOAP Notes are a way for massage therapists and other healthcare providers to map where a client has been and where they are going. The unique SOAP format (Subjective, Objective, Assessment, and Plan) of these reports helps you keep track of your client's condition and progress through each treatment session.
What does soap mean in therapy?
Subjective, Objective, Assessment, PlanSOAP is an acronym that stands for Subjective, Objective, Assessment, Plan. Let's unpack each section of the note.
Do massage therapists have to do SOAP notes?
(Updated for 2022) Writing treatment notes is one of the routine activities that massage therapists do every day. The most common form that therapists use to document their client sessions is the SOAP note.
What does SOAP notes stand for?
Subjective, Objective, Assessment and PlanThe Subjective, Objective, Assessment and Plan (SOAP) note is an acronym representing a widely used method of documentation for healthcare providers. The SOAP note is a way for healthcare workers to document in a structured and organized way.[1][2][3]
What does SOAP stand for SLP?
A SOAP note is a written document that a healthcare professional creates to describe a session with a patient/client. The information included is: Subjective, Objective, Assessment, Plan (SOAP).
How do you fill out a SOAP note?
Tips for completing SOAP notes:Consider how the patient is represented: avoid using words like “good” or “bad” or any other words that suggest moral judgments.Avoid using tentative language such as “may” or “seems”Avoid using absolutes such as “always” and “never”Write legibly.More items...
How long do you have to keep SOAP notes?
SOAP NOTE POLICY (b) Maintain these client records for at least 11 years from the date of the last entry or, if the client is less than 18 years old, at least 11 years from the date the client becomes 18 years of age.
How do you write a massage therapy plan?
Start by asking your client what their goal for treatment is.(Describe the client's goal and benchmark indicating success)(Include things like duration of sessions, number of sessions, how far apart sessions will be scheduled, and what modality to use)(Recommendations on what to do in between sessions.
What does Lord ficara mean?
One of the most common tools taught to therapists to help them get the appropriate type and scope of questions asked is the acronym “OL' DR FICARA” which stands for (as one variation has it): Onset, Location, Duration, Radiation, Frequency, Intensity, Character, Aggravation, Relieving, & Associated symptoms.
How do you read SOAP notes?
0:436:33SOAP NOTES - YouTubeYouTubeStart of suggested clipEnd of suggested clipThe subjective section of your soap note should contain information gathered by talking to theMoreThe subjective section of your soap note should contain information gathered by talking to the patient. The family members and the medical record review depending. Upon the nature of the encounter.
What is a good SOAP note?
However, all SOAP notes should include Subjective, Objective, Assessment, and Plan sections, hence the acronym SOAP. A SOAP note should convey information from a session that the writer feels is relevant for other healthcare professionals to provide appropriate treatment.
How do you present a patient's soap?
The SOAP format can help.Subjective Notes. For the subjective segment, lead with a one-sentence reminder of who your patient is. ... Objective Notes. Open this segment by discussing vital signs, including blood pressure, pulse, respirations, temperature, and oxygen saturations. ... Assessment Notes. ... Plan Notes.
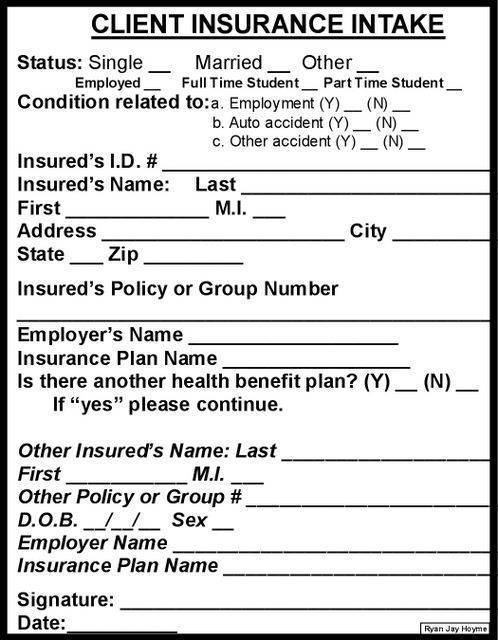
Free SOAP Notes Form
SOAP (Subjective, Objective, Assessment and Plan) notes are used at intake and ongoing to document a client's condition and progress. They are also useful when communicating with insurance companies.
Prefer Digital SOAP Notes?
If you're ready to take your client documentation off the page and into the cloud, check out ClinicSense, a complete practice management software package — AMTA members save 25%.
Why Are SOAP Notes Important?
SOAP Notes can be time-consuming to complete. But don’t underestimate the importance of this record-keeping method. Well-written, detailed SOAP Notes enable you and your staff to quickly memorialize and communicate essential information about a person’s current health status and their ongoing treatment plan.
SOAP: What Does It Stand For?
Subjective: information about the client’s own description of their chief complaint
A Massage Therapy SOAP Notes Example
To illustrate the entire note-taking process in action, let’s take another massage therapy SOAP notes example. In this case, the subjective phase of the SOAP process begins by noting that the client’s chief complaint is pain in the lower back and upper leg.
Tips for Writing Good SOAP Notes
How can you create well-written SOAP Notes that help keep everyone on the same page?
Speed up Your Note-taking and Streamline Your Filing by Going Digital with Help from ClinicSense
Taking handwritten notes using a printed form can get the job done. But, if manually recording and filing your SOAP notes seems like too much of a drag on your time, there is an alternative.
Make Taking SOAP Notes Easy with ClinicSense
With ClinicSense, taking SOAP notes is as easy as pointing and clicking to answer a few key questions. No more writing, typing or trying to figure out what to say. Transform your responses into finalized notes quickly, easily and professionally.
What is soap made of?
Soap is detergent and used as a cleanser. green soap ( medicinal soap) ( soft soap) a soap made from vegetable oils other than coconut oil or palm kernel oil, potassium hydroxide as an alkali, and glycerin.
What does S stand for in a clinical setting?
Acronym for the conceptual device used by clinicians to organize the progress notes in the problem-oriented record; S stands for subjective data provided by the patient, O for objective data gathered by health care professionals in the clinical setting, A for the assessment of the patient's condition, and P for the plan for the patient's care.
What Are SOAP Notes?
Professionals in the medical and psychological fields often use SOAP notes while working with patients or clients. They are an easy-to-understand process of capturing the critical points during an interaction. Coaches also can make use of SOAP notes, with some adaptations.
Why Are SOAP Notes Important?
Cynthia Moreno Tuohy, executive director of the Association for Addiction Professionals, has highlighted the importance of quality SOAP notes for more than 40 years.
Writing Your SOAP Notes
The primary thing to keep in mind is that SOAP notes are meant to be detailed, but not lengthy. They are a clear and concise record of each interaction with the patient or client.
2 SOAP Note Examples
Your client Tom Peters met with you this morning. Your notes are as follows:
3 Useful Templates
Numerous websites offer free SOAP templates. Most are designed for use in the medical professions, including client-centered therapy and counseling. Here are three templates you can use for a medical visit, therapy, or coaching session.
A Take-Home Message
Whether you are in the medical, therapy, counseling, or coaching profession, SOAP notes are an excellent way to document interactions with patients or clients. SOAP notes are easy to use and designed to communicate the most relevant information about the individual. They can also provide documentation of progress.
