Alpha-adrenergic agonists (decrease inflow)
- Decrease aqueous humor production as well as an increase in uveoscleral outflow.
- No tachyphylaxis.
- Brimonidine: no effect on mean heart rate, blood pressure, or pulmonary function.
- Should not be given with oral monoamine oxidase inhibitor antidepressants due to the risk of hypertensive crisis.
Can aqueous humor formation be reduced pharmacologically?
There are many other ways in which aqueous humor formation can be reduced pharmacologically ( Table 11.2 ).
How does long-term topical administration of epinephrine affect aqueous humor formation?
At one time it was generally believed that long-term topical administration of epinephrine, a combined α 1 , α 2, β 1 , β 2 -adrenergic agonist, would decrease the rate of aqueous humor formation. This effect was thought to be mediated by β-adrenergic receptors in the non-pigmented ciliary epithelium, via activation of a membrane adenylate cyclase.
Do cholinomimetics affect aqueous humor formation?
Overall, cholinomimetics have little effect on the volumetric rate of aqueous humor formation. In general, cholinergic drugs cause vasodilation in the anterior segment resulting in increased blood flow to the choroid, iris, ciliary processes, and ciliary muscle (see Chapter 10 ).
What are the effects of aqueous humor suppression on trabecular meshwork?
Long-term suppression of aqueous humor formation and redirection of aqueous drainage from the trabecular to the uveoscleral pathway could lead to underperfusion of the trabecular meshwork with detrimental morphologic and functional effects

Which drug reduces production of aqueous humor?
This type of medication works to lower eye (intraocular) pressure by reducing aqueous humor production and decreasing the rate at which the fluid flows into the eye. Examples include: Timolol (Timoptic XE Ocumeter® and Timoptic®) Levobunolol (Betagan®)
Which medications used in the treatment of glaucoma reduce production of aqueous humor?
Carbonic anhydrase inhibitors: lower the production of aqueous humor.
How do beta blockers reduce aqueous humor production?
Topical beta-blockers reduce the intraocular pressure (IOP) by blockade of sympathetic nerve endings in the ciliary epithelium causing a fall in aqueous humour production.
Which glaucoma drugs decrease intraocular pressure IOP by decreasing the production of aqueous humor?
BETA BLOCKERS Timolol maleate (Timoptic) is the standard agent against which other medications are measured in terms of efficacy, side effects and cost. Beta blockers are thought to lower IOP mainly by decreasing aqueous humor production in the ciliary body of the eye.
How do you reduce aqueous humor?
For example, aqueous humor production is reduced by both topical and systemic carbonic anhydrase inhibitors which decrease the production of aqueous humor by the epithelial cells of the ciliary body.
What medications should be avoided with glaucoma?
Closed-Angle Glaucoma: Medicines to AvoidAntihistamines and decongestants.Asthma medicines.Motion sickness medicines.Some medicines used to treat depression (tricyclic antidepressants).
What are aqueous suppressants?
Medications either decrease the production of aqueous fluid (called “aqueous suppressants”) or facilitate its outflow from the eye (referred to as “outflow drugs”) to lower the IOP. There are two main outflow passages from the eye: the conventional outflow and uveoscleral outflow.
How does timolol decrease aqueous humor?
Timolol This beta adrenoceptor antagonist is applied topically as eye drops. It lowers IOP by blocking beta adrenoceptors in the ciliary body of the eye, which reduces the production rate of aqueous humor.
How does timolol decrease production of aqueous humor?
The results indicate that timolol reduces the rate of aqueous humor formation through reduction of blood flow to the ciliary process rather than via the inhibition of the active transport system or that of prostaglandin biosynthesis.
What is the fastest way to reduce IOP?
How Do I Lower My Intraocular PressureEat a Healthy Diet. Eating a healthy and balanced diet is helpful when managing your eye pressure. ... Exercise. Moving your body is important for your health. ... Reduce Your Caffeine Intake. ... Elevate Your Head While Sleeping. ... Medications.
What glaucoma drop decreases aqueous humor?
a)Timolol- is one of the most popular and prescribed antiglaucoma agents, as a first-line drug in most forms of open angle glaucoma and ocular hypertension [2]. It reduces the production of aqueous humor by acting on the ciliary body, inhibiting beta 1 and beta 2 adrenergic receptors.
What is the first-line drug for glaucoma?
Bimatoprost, based on the efficacy, safety and ease of use, has been approved as a first-line treatment for glaucoma, and well positioned among the first-choices in glaucoma medical therapy.
Which of the following medications used in the treatment of glaucoma works by constricting the pupils to open the angle and allow aqueous fluid to escape?
Miotics to Treat Glaucoma Miotics are parasympathomimetic agents. These drugs work by constricting the pupil as well as other internal muscles of the eye; as a result there is an increased drainage of aqueous humor through the trabecular meshwork, reducing intraocular pressure.
How do prostaglandin analogues work in glaucoma?
Prostaglandin analogues are the front-line medications for the treatment of glaucoma, a condition resulting in blindness due to the death of retinal ganglion cells. These drugs act by lowering intraocular pressure (IOP), a major risk factor for glaucoma.
What medications increase eye pressure?
Steroids. Corticosteroids, or steroids, can raise eye pressure, especially in those persons who have open-angle glaucoma, first-degree relatives of those with open-angle glaucoma, elderly and young (<6 years) persons, those with type 1 diabetes and those with high myopia (short-sightedness).
Does pilocarpine cause Miosis?
Pilocarpine will also cause constriction of the pupillary sphincter muscle, resulting in miosis. The allowable daily dose is 30 mg.
How to reduce aqueous humor?
There are many other ways in which aqueous humor formation can be reduced pharmacologically ( Table 11.2 ). Effective compounds include: the guanylate cyclase activators atrial natriuretic factor , and the nitrovasodilators sodium nitroprusside, , sodium azide, and nitroglycerin. 8-Bromo cyclic GMP also reduces the aqueous humor formation rate by 15–20 percent in the monkey. Atrial natriuretic factor injected intravitreally reduces IOP and aqueous humor formation in rabbits and monkeys. However, intracameral and intravenous administration of atrial natriuretic factor to monkeys increases aqueous humor formation. Atrial natriuretic factor levels are elevated in aqueous humor of rabbits following topical treatment with kappa opioid agonists, which results in IOP reduction and aqueous humor formation suppression. However, non-kappa opioid mechanisms are responsible for aqueous humor formation and IOP reductions in monkeys. Nitric oxide may be involved in mediating the IOP lowering response to mu3 opioid agonists in rabbits.
Which mechanism plays a major role in aqueous humor formation and drainage?
Due to the autonomic innervation and receptors of the relevant structures, adrenergic and cholinergic mechanisms play major roles in aqueous humor formation and drainage in terms of both normal physiology and glaucoma therapeutics, while evidence for other mechanisms, including serotonergic, dopaminergic, adenosinergic, nitrergic, cannabinergic, prostaglandin (PG)ergic, , and cytoskeletal (see review ), has been established.
How do cholinomimetics affect the blood-aqueous barrier?
The effects of cholinergic drugs on aqueous humor formation and composition and on the blood–aqueous barrier are unclear. Overall, cholinomimetics have little effect on the volumetric rate of aqueous humor formation. In general, cholinergic drugs cause vasodilation in the anterior segment resulting in increased blood flow to the choroid, iris, ciliary processes, and ciliary muscle (see Chapter 10 ). However cholinergic drugs may also promote vasoconstriction in the rabbit eye. Congestion in the iris and ciliary body is a well-recognized clinical side-effect of topical cholinomimetics, especially the anticholinesterases. The presence of flare and cells in the aqueous humor by biomicroscopy indicates that these agents can cause breakdown of the blood–aqueous barrier and perhaps frank inflammation. Pilocarpine increases blood–aqueous barrier permeability to iodide and inulin. Cholinergic drugs may alter the aqueous humor concentration of inorganic ions and the movement of certain amino acids from the blood into the aqueous humor and may also influence the outward-directed transport systems of the ciliary processes. , Cholinergic agents can disrupt the coupling and Na + currents between pigmented and non-pigmented epithelial cells in vitro, suggesting a possible inhibitory effect on aqueous secretion , although this is likely to be minimal as stated below.
How does aqueous humor differ from plasma?
The composition of aqueous humor differs from that of plasma as a result of two important physiological characteristics of the anterior segment: a mechanical epithelial/endothelial blood–aqueous barrier, and active transport of various organic and inorganic substances by the ciliary epithelium . The greatest differences are the low protein and high ascorbate concentrations in the aqueous relative to plasma (200 times less and 20 times greater, respectively).
What are the three processes that contribute to the formation of aqueous humor?
Three physiologic processes contribute to the formation and chemical composition of the aqueous humor: diffusion, ultrafiltration (and the related dialysis), and active secretion . Diffusion and ultrafiltration are responsible for the formation of the “reservoir” of the plasma ultrafiltrate in the stroma, from which the posterior chamber aqueous is derived, via active secretion across the ciliary epithelium. Energy-dependent active transport of sodium into the posterior chamber by the non-pigmented ciliary epithelium ( Fig. 11.3 ) results in water movement from the stromal pool into the posterior chamber. It seems fairly certain that under normal conditions active secretion accounts for perhaps 80–90 percent of total aqueous humor formation. The observation that moderate alterations in systemic blood pressure and ciliary process blood flow have little effect on aqueous formation rate supports this notion. ,
What is the IOP of aqueous humor?
In the healthy eye, flow of aqueous humor against resistance generates an intraocular pressure (IOP) of approximately 15 mmHg, necessary for the proper shape and optical properties of the globe. The circulating aqueous nourishes the cornea and lens, structures which must be transparent and therefore devoid of blood vessels as well as the trabecular meshwork (TM). The aqueous also provides a transparent and colorless medium of refractive index 1.33332 between the cornea and lens, thus constituting an important component of the eye’s optical system. The basic anatomy of the primate anterior ocular segment and the normal pathways of aqueous humor flow are illustrated schematically in Figures 11.1 and 11.2 .
Where does aqueous humor enter the ciliary process?
Aqueous humor is secreted by the ciliary epithelium lining the ciliary processes (as a consequence of active ionic transport across the ciliary epithelium and hydrostatic and osmotic gradients between the posterior chamber and the ciliary process vasculature and stroma), and enters the posterior chamber.
How much aqueous humour is produced in the ciliary body?
On average, the ciliary body produces around 2.5 μl of aqueous humour per minute . The 3 processes that play a part in this production include: Diffusion.
Where is aqueous humor located?
Aqueous humour is a transparent fluid located inside the eye, specifically within the anterior and posterior chambers. It has several key functions, and plays an important role in disease states such as glaucoma.
Why should monoamine oxidase inhibitors not be given with oral monoamine oxidase answer?
Should not be given with oral monoamine oxidase inhibitor antidepressants due to the risk of hypertensive crisis.
Is apriclonidine a base or a suppressant?
The addition of Apraclonidine Ophthalmic Solution, USP 0.5% as base to patients already using two aqueous suppressing drugs (i.e., beta-blocker plus carbonic anhydrase inhibitor) as part of their maximally tolerated medical therapy may not provide additional benefit. This is because Apraclonidine Ophthalmic Solution, USP 0.5% as base is an aqueous suppressing drug and the addition of a third aqueous suppressant may not significantly reduce IOP.
Does brimonidine tartrate increase uveoscleral outflow?
Fluorophotometric studies in animals and humans suggest that brimonidine tartrate has a dual mechanism of action by reducing aqueous humor production and increasing uveoscleral outflow.
Can apraclonidine be used for glaucoma?
The clinical utili ty of apraclonidine ophthalmic solution is most apparent for those glaucoma patients on maximally tolerated medical therapy. Patients on maximally tolerated medical therapy with uncontrolled IOP and scheduled to undergo laser trabeculoplasty or trabeculectomy surgery were enrolled into a double-masked, placebo-controlled, multi-center clinical trial to determine if apraclonidine ophthalmic solution, dosed three times daily, could delay the need for surgery for up to three months.
Is apraclonidine a selective agonist?
Pharmacology : Apraclonidine hydrochloride is a relatively selective alpha-2-adrenergic agonist. When instilled in the eye, apraclonidine ophthalmic solution has the action of reducing elevated, as well as normal, intraocular pressure (IOP), whether or not accompanied by glaucoma. Ophthalmic apraclonidine has minimal effect on cardiovascular parameters.
Is alphagan ophthalmic a lowering solution?
A clinical study was conducted to evaluate the safety, efficacy, and acceptability of ALPHAGAN® P (brimonidine tartrate ophthalmic solution) 0.1% compared with ALPHAGAN® administered three-times-daily in patients with open-angle glaucoma or ocular hypertension. Those results indicated that ALPHAGAN® P (brimonidine tartrate ophthalmic solution) 0.1% is equivalent in IOP lowering effect to ALPHAGAN® (brimonidine tartrate ophthalmic solution) 0.2%, and effectively lowers IOP in patients with open-angle glaucoma or ocular hypertension by approximately 2-6 mmHg.
Does apraclonidine ophthalmic solution decrease IOP?
The IOP lowering efficacy of Apraclonidine Ophthalmic Solution, USP 0.5% as base diminishes over time in some patients. This loss of effect, or tachyphylaxis, appears to be an individual occurrence with a variable time of onset and should be closely monitored. The benefit for most patients is less than one month.
What is the treatment for aqueous humor formation?
Suppression of aqueous humor formation is the mainstay of therapy. Therapeutic options include topical therapy with β-adrenergic antagonists, carbonic anhyd rase inhibitors, or α-adrenergic agonists. Systemic carbonic anhydrase inhibitors can be very effective, particularly in eyes with an acute attack. Topical carbonic anhydrase inhibitors can aggravate corneal edema and should be avoided during the acute attack.
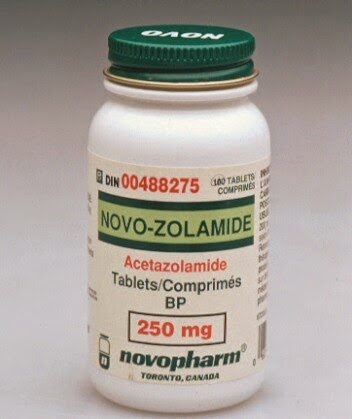
How does acetazolamide affect aqueous humor secretion?
All CAIs inhibit the active aqueous humor secretion by blocking CA in the nonpigmented ciliary epithelial cells in the ciliary processes. Systemic acetazolamide decreases aqueous humor secretion by 30%. 2 When given orally, the IOP decrease is already detectable at 30 minutes after administration, reaches its peak at 2 hours, and lasts at least for 6–8 hours. The washout time of the systemic CAIs is 3 days. 7 Acetazolamide binds to plasma proteins to the extent of 93%, and it is removed from the body via renal excretion without metabolism. The renal excretion of methazolamide is only 25%, and therefore its clinical use is less limited by impaired renal function. 1,3
How do CAIs lower IOP?
The best evidence suggests that they lower IOP by reducing bicarbonate (and possibly chloride ion) movement and aqueous humor formation via a direct effect on ciliary epithelial CA. All of the CAIs share a common structure of the organic anion SO 2 NH2 ( Fig. 26-1 ). This suggests that CAIs may compete with the OH2 ion at the active site on the enzyme. 36,55 The ocular hypotensive response is probably augmented by the induced systemic acidosis, which would explain the small increase in effect of systemic over topical agents in humans. 56
What are the inflow drugs for glaucoma?
Several classes of inflow drugs are prescribed for glaucoma therapy, including β-blockers, CAIs, α 2 adrenergic agonists, and other sympathomimetics. Each class reduces aqueous flow by different mechanisms. β-Blockers block cAMP and reduce the autonomic tone needed to produce aqueous humor. CAIs block carbonic anhydrase which prevents the synthesis of bicarbonate, a key step in aqueous secretion. Sympathomimetics have mixed effects on aqueous production, depending on which receptor subtype is stimulated and to what degree.
What is pilocarpine used for?
Pilocarpine is used to constrict the pupil and draw the peripheral iris away from the trabecular meshwork. Eyes in which angle closure has an element of pupillary block are often improved by pilocarpine; however, for eyes in which angle closure is caused by forward lens movement, ciliary block, or an intumescent lens, copious pilocarpine may contract the ciliary circular muscles resulting in anterior lens movement and paradoxical worsening of the angle closure. Pilocarpine is frequently ineffective during the acute high IOP period and in eyes with extensive synechial closure.
Why is aqueous flow not a preferred therapy for glaucoma?
Suppression of aqueous flow is not the preferred therapy for glaucoma because disturbing the production and flow of this essential fluid could potentially stress the eye in other ways. New classes of drugs under development for the treatment of elevated IOP are designed to target the outflow tissues rather than the inflow tissues because abnormalities in the outflow pathways are usually the source of the IOP elevation.
How does aqueous humor change with age?
Aqueous humor formation gradually slows with age by about 4% per decade of life. One might expect this decrease to diminish the efficiency of the circulatory function, but the reduction in flow is accompanied by a reduction in the volume of the anterior chamber by approximately 14–24 μl per decade. The smaller anterior chamber requires less flow to maintain the same clearance. From age 20 to 80 years, aqueous humor flow rate decreases by approximately 25%, while anterior chamber volume decreases by 40%, and this combined change provides a 20% faster turnover rate of aqueous humor over a lifetime.