
What is a buccal lesion? White mucosal lesions may result from thickening of one or several layers of the oral epithelium. They vary in size and depth, generally have an irregular outline, and may be solitary or multifocal. Common sites are the buccal mucosa
Oral mucosa
The oral mucosa is the mucous membrane lining the inside of the mouth. It comprises stratified squamous epithelium, termed "oral epithelium", and an underlying connective tissue termed lamina propria. The oral cavity has sometimes been described as a mirror that reflects the health of the individual. Changes indicative of disease are seen as alterations in the oral mucosa lining the mouth, which ca…
What are the most common oral lesions?
The most common treatments, after oral hygiene, are:
- Use of local and oral steroids that have effect on T-lymphocytes and reduce inflammation.
- Use of local antibiotics, for example, chlorohexidine, benzidamine.
- Solving vitamin and mineral deficiency, such as B12, iron, folic acid, and avoidance of food allergens.
What is buccal used for?
Common buccal medications include Suboxone, or buprenorphine-naloxone, used to treat opioid addiction. Fentanyl is used for pain, antipsychotics for schizophrenia and bipolar, and nitroglycerin for chest pains related to heart problems. Other buccal medicines prescribed include anti-seizure, testosterone, nicotine, and antibiotics.
How to pronounce buccal in English?
Pronunciation of buccal with 3 audio pronunciations. 1 rating. 0 rating. 0 rating. International Phonetic Alphabet (IPA) IPA : ˈbʌk (ə)l. Record the pronunciation of this word in your own voice and play it to listen to how you have pronounced it. Can you pronounce this word better.
What is the function of the buccal mucosa?
The Anatomy of the Buccal Nerve
- Anatomy. The buccal nerve sits high up in the corner of your cheek. ...
- Function. The buccal nerve innervates the mucous membrane, vestibular gingiva, and gum area that begins behind the first and second premolars. ...
- Associated Conditions. ...
- Rehabilitation. ...
What causes a lesion in the mouth?
The most common causes of oral lesions are localised trauma (i.e. rubbing from a sharp edge on a broken filling), infections, systemic conditions, associated dermatological diseases and recurrent aphthous ulcers (canker sores). Oral lesions may form individually or multiple lesions may appear at the same time.
Are oral lesions serious?
Precancerous oral lesions are abnormal cell growths in or around the mouth. They may become cancer. Cancerous oral lesions are life-threatening cell changes in the mouth. These lesions need to be found early to give you a better chance for a cure.
What are the most common oral lesions?
The most common oral lesions are leukoplakia, tori, inflammatory lesions, fibromas, Fordyce's granules, hemangiomas, ulcers, papillomas, epuli and varicosities.
What does a lesion in the mouth look like?
Canker sores may look like small oval-shaped ulcers in your mouth that appear white, gray, or yellow. They may be surrounded by a red “halo” of irritation. They may also appear as a painful red area. Canker sores are also called aphthous stomatitis or aphthous ulcers.
When should I be concerned about oral lesions?
A sore in the mouth that doesn't heal within two weeks. White or red lesions or ulcers on the tongue, gums, or lining of the mouth that do not go away. Soreness or pain in the mouth that persists. A lump or thickening in the cheek area.
How do you treat oral lesions?
What are some ways to treat mouth ulcers?using a rinse of saltwater and baking soda.placing milk of magnesia on the mouth ulcer.covering mouth ulcers with baking soda paste.using over-the-counter benzocaine (topical anesthetic) products like Orajel or Anbesol.applying ice to canker sores.More items...
Do oral lesions go away?
A: Many lesions do improve and in some cases may even disappear. It is certainly desirable to stop smoking for many health reasons. Even after you stop smoking, you are still at risk for oral premalignant lesions, although your risk will decrease over time.
What doctor treats oral lesions?
Oral lesions can be benign or malignant; referral to a dentist or an otolaryngologist is appropriate if any lesion persists for more than two weeks.
Are most oral lesions benign?
Most oral growths are benign. Warts, candidal infections, and repeated trauma are common causes of benign growths. Use of alcohol and tobacco and oral HPV infection are risk factors for cancer.
How long does it take for mouth lesions to heal?
Mouth sores often go away in 10 to 14 days, even if you do not do anything. They sometimes last up to 6 weeks. The following steps can make you feel better: Avoid hot beverages and foods, spicy and salty foods, and citrus.
How long do mouth lesions take to heal?
Mouth ulcers are common and should clear up on their own within a week or 2. But see a GP or dentist if you have a mouth ulcer that lasts longer than 3 weeks.
Can stress cause mouth lesions?
Mouth ulcers are referred to in the medical community as “aphthous ulcers.” Stress is a common cause of mouth ulcers, and a recent study points to the relationship between mental health and oral health. “The researchers found a significant correlation between experiencing mouth ulcers and depressive symptoms.”
buccal
adjective Referring to side of a tooth or gingiva facing the cheek or lip.
buccal
relating to the mouth cavity. For example, buccal epithelium lines the inside of the cheeks.
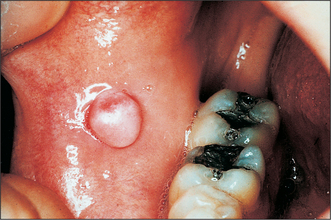
What are the signs of a Buccal Exostosis?
Signs and symptoms. Buccal exostoses are bony hamartomas, which are non- malignant, exophytic nodular outgrowths of dense cortical bone that are relatively avascular.’. Symptoms: Buccal exostoses generally tend to be asymptomatic and are usually painless.
How often should you clean your mouth for buccal exostosis?
Patients are given oral hygiene advice and are advised to cleanse above and below the growth with a mouthwash once a day to remove any food debris.
How long does it take to get a patient recalled after a suture removal?
Routine post-operative instructions are given to the patient and occasionally antibiotics may be prescribed. The patient will then be recalled after 1 week in order to remove the sutures and often after a few months for post-operative follow up.
What is the prevalence rate of maxilla?
The maxilla is shown to display a higher prevalence rate of 5.1:1 in comparison to mandible. Males also are afflicted more than females with a prevalence rate of 1.66:1, in all intraoral locations. The overlying mucosa appears to be stretched but intact and normal in colour.
Is a bony prominence malignant?
Initial presentation usually occurs in early adolescence and the lesions may slowly enlarge up to 3-4cm in diameter with time, however there is no malignant potential.
Can you get a dental tomography for exostosis?
Dental panoramic tomography and cone beam tomography can be used to confirm diagnosis. An additional biopsy for diagnosis of buccal exostosis is not usually recommended, however it is important to rule out the possibility of early osseosarcomas and chondrosarcomas.
What is the name of the cancer that starts when the cells that make up the inner cheek grow out of control?
Inner Cheek Cancer (Buccal Mucosa Cancer) Share. Print. Share. Print. Inner cheek cancer (also called buccal mucosa cancer) is a type of head and neck cancer that begins when the cells that make up the inner cheek grow out of control and form lesions or tumors.
What is the treatment for inner cheek cancer?
If the cancer is more advanced, radiation, chemotherapy, or both may be used to shrink the tumor before or after surgery to reduce the risk of the cancer coming back.
How do you know if you have inner cheek cancer?
Signs of inner cheek cancer may include the following: white, red, or dark patches in the mouth. a lump in your mouth. mouth pain or numbness. soreness or a feeling that something is caught in your throat. difficulty moving your jaw. severe ear pain. hoarseness.

Overview
Diagnosis
The presence of buccal exostosis can be diagnosed by both clinical examination and radiological interpretation of the oral cavity.
Clinically, buccal exostoses appear as single, broad-based masses, usually situated bilaterally in the premolar and molar region on the facial surface of the maxillary alveolar bone. The mass is generally smooth although in some cases a sharp, bony prominence may be present resulting in …
Signs and symptoms
Buccal exostoses are bony hamartomas, which are non- malignant, exophytic nodular outgrowths of dense cortical bone that are relatively avascular.’
Symptoms:
Buccal exostoses generally tend to be asymptomatic and are usually painless. However, they may increase patient concern about poor aesthetics, inability to perform oral hygiene procedures du…
Causes
Why buccal exostoses form is unclear, but it may involve bruxism (tooth clenching and grinding), and genetic factors. Typically they first appear in early adulthood.
Management
Currently, buccal exostoses do not commonly require treatment. If there is neither pain nor sensitivity, the buccal exostosis simply needs to be monitored with routine dental check-ups. Patients are given oral hygiene advice and are advised to cleanse above and below the growth with a mouthwash once a day to remove any food debris. Due to it being difficult to clean around the exostosis, periodontal disease can often occur as a result, and so this should be treated by t…
Epidemiology
They are more common in males than females, occurring in a ratio of about 5:1. They are strongly associated with the presence of torus mandibularis and torus palatinus.