What is the prevalence of Category II fetal heart rate tracing?
Management of the category II fetal heart rate (FHR) tracing presents a common challenge in obstetrics. Up to 80% of women will have a category II FHR tracing at some point during labor.
What are the different types of fetal heart tracing?
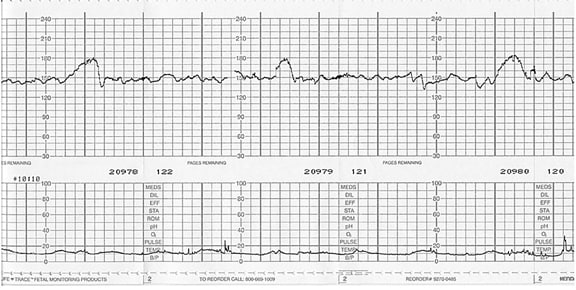
Fetal heart tracings into three broad categories: Category 1, Category 2, Category 3. What Is a Category 1 Fetal Heart Tracing? Category 1 fetal heart tracings are predictive of a normal acid-basis status for the fetus. In other words, a Category 1 fetal heart tracing means the baby is getting enough oxygen.
What is a Category 2 FHR?
In summary, physicians are usually in agreement with FHR tracings that are normal (Category I) and those that demonstrate severe fetal compromise (Category III) (10). It is those tracings in Category II with all the possibilities that exist that pose the problem.
What is the difference between Category I and Category II tracings?
Category I FHR tracings include all of the following: Category II FHR tracings include all FHR tracings not categorized as Category I or Category III. Category II tracings may represent an appreciable fraction of those encountered in clinical care. Examples of Category II FHR tracings include any of the following:
What is a Category 2 strip?
Category II FHR tracings: Indeterminate, require evaluation and continued surveillance and reevaluation. Examples of these tracings include any of the following: – Bradycardia not accompanied by absent variability. – Tachycardia. – Minimal or marked baseline variability.
What is a Category 1 fetal heart rate tracing?
Category I. All of the following criteria must be present. Tracings meeting these criteria are predictive of normal fetal acid-base balance at the time of observation. Baseline rate: 110 to 160 bpm.
What are the categories of fetal heart tracing?
Assigning FHR Patterns to CategoriesBaseline rate: 110-160 beats per minute.Baseline FHR variability: moderate.Late or variable decelrations: absent.Early decelerations: present or absent.Accelerations: present or absent.
What is a Category 3 tracing?
Meanwhile, a Category 3 fetal heart tracing is predictive of an abnormal fetal acid-base status, meaning that the fetus is not getting enough oxygen. Category 3 fetal heart tracings require immediate action and prompt delivery via cesarean section. Category 3: Minimal Variability with Recurrent Decelerations.
What number is a contraction on monitor?
The intensity of Braxton Hicks contractions varies between approximately 5-25 mm Hg (a measure of pressure). For comparison, during true labor the intensity of a contraction is between 40-60 mm Hg in the beginning of the active phase.
What Toco number is a contraction?
Your TOCO number can reach 50-80 mmHg during the second stage of labor, which is when your cervix is fully dilated, and you are ready for childbirth....What TOCO Number is a Contraction?Type of contractionTOCO numberBraxton Hicks contractionsVaries between 5-25 mmHgActive labor contractionsIntensity of a contraction is between 40-60 mmHg1 more row•Mar 28, 2022
Which FHR tracing would be considered reassuring?
The presence of accelerations is considered a reassuring sign of fetal well-being. An acceleration pattern preceding or following a variable deceleration (the “shoulders” of the deceleration) is seen only when the fetus is not hypoxic.
What are the four types of variability?
What are the 4 main measures of variability?Range: the difference between the highest and lowest values.Interquartile range: the range of the middle half of a distribution.Standard deviation: average distance from the mean.Variance: average of squared distances from the mean.
How frequently should a FHR Category I tracing be reviewed in a low risk patient in the second stage of labor?
This is a normal tracing. Intermittent or continuous fetal monitoring based on clinical status and underlying risk factors. Review every 30 minutes in the first stage and every 15 minutes in the second stage of labor.
What is a normal fetal heart rate?
The average fetal heart rate is between 110 and 160 beats per minute. It can vary by 5 to 25 beats per minute.
What is a normal baseline fetal heart rate?
Introduction. A baseline fetal heart rate between 110 and 160 bpm is considered normal. However, among normal fetuses the average baseline heart rate has been shown to diminish progressively and the 90th centile of the fetal heart rate at 40 weeks of gestation has been consistently found at around 150 bpm.
What category is late deceleration?
Category III is defined as fetal heart rate pattern with absent variability, recurrent variable, and late decelerations, bradycardia, or sinusoidal pattern.
Which FHR tracing would be considered reassuring?
The presence of accelerations is considered a reassuring sign of fetal well-being. An acceleration pattern preceding or following a variable deceleration (the “shoulders” of the deceleration) is seen only when the fetus is not hypoxic.
How frequently should a FHR Category I tracing be reviewed in a low risk patient in the second stage of labor?
This is a normal tracing. Intermittent or continuous fetal monitoring based on clinical status and underlying risk factors. Review every 30 minutes in the first stage and every 15 minutes in the second stage of labor.
How do I read my NST results?
Interpreting an NST ResultPositive = Good Acid Base Status.Fetal Baseline = 110 to 160 BPM.Baseline Variability = Moderate.2+ Accelerations in 20 minutes.Early Decelerations.
What is a normal fetal heart rate?
The average fetal heart rate is between 110 and 160 beats per minute. It can vary by 5 to 25 beats per minute.
Background for Management of Category II Fetal Heart Tracings (FHTs)
2020 OBI workstation data shows that abnormal or indeterminate fetal heart rate tracings was the second most common indication for cesarean delivery. Since this represents such a large portion of primary cesarean births in Michigan, quality improvement efforts will need to focus on effectively managing this common clinical finding.
QI Implementation Requirements for Management of Category II Fetal Heart Tracings (FHTs)
For NTSV patients with category II fetal heart rate tracings (including those that are indeterminate) that proceed to cesarean delivery, this project will focus on the implementation of standardized, evidence-based guidance for the management of category II fetal heart tracings through the use of a checklist or algorithm that guides clinical decision making.
Is there a national standard for FHR monitoring?
There is currently no standard national approach to the management of category II fetal heart rate (FHR) patterns, yet such patterns occur in the majority of fetuses in labor. Under such circumstances, it would be difficult to demonstrate the clinical efficacy of FHR monitoring even if this technique had immense intrinsic value, ...
Is there a national approach to FHR?
There is currently no standard national approach to the management of category II fetal heart rate (FHR) patterns, yet such patterns occur in the majority of fetuses in labor. Under such circumstances, it would be difficult to demonstrate the clinical efficacy of FHR monitoring even if this techniqu …
What is a Category II FHR tracing?
Category II FHR tracings include all FHR tracings not categorized as Category I or Category III. Category II tracings may represent an appreciable fraction of those encountered in clinical care. Examples of Category II FHR tracings include any of the following:
How many contractions are normal in 10 minutes?
Normal: five contractions or less in 10 minutes, averaged over a 30-minute window. Tachysystole: more than five contractions in 10 minutes, averaged over a 30-minute window. Always include presence or absence of associated FHR decelerations. Applies to both spontaneous and stimulated labor.
Does FHR tracing provide information?
It is important to recognize that FHR tracing patterns provide information only on the current acid–base status of the fetus. Tracing patterns can and will change! For more information on the use, interpretation and management of patients based on Fetal Heart Tracings check out the resources below.
Is EFM a common tool?
While EFM use may be common and widespread, there is controversy about its efficacy, interobserver and intraobserver variability, and management algorithms. While it can be an important tool to assess fetal wellbeing, it is also limited by its high false-positive rate.
When does the nadir and recovery of the deceleration occur?
Onset, nadir, and recovery of the deceleration occur after the beginning, peak, and ending of the contraction, respectively.
Is acid-base status predictive of fetal acid-base status?
Not predictive of abnormal fetal acid–base status, yet presently there is not adequate evidence to classify these as Category I or Category III.
What does minimal variability mean?
Minimal variability is a troubling sign. It indicates that oxygen reserves are being depleted. Similarly, repetitive and persistent late decelerations are a reliable sign of oxygen deprivation.
What happens if a child has a period of minimal variability?
If the doctors and nurses ignore that warning or fail to recognize that periods of minimal variability accompanied by recurrent decelerations are indicative of abnormal fetal acid-base status and hypoxia, the child runs the risk of a serious birth injury or death.
What is the normal heart rate for a fetus?
A normal fetal heart rate is 110 - 160 beats per minute. An elevated heart rate by itself does not make this a Category 3 fetal heart tracing.
Why does my fetus' heart pump faster?
However, the fact that it is present with the decelerations most likely indicates that the fetus’ heart is pumping faster to supply more oxygen to the rest of its’ body. Unfortunately for this patient, the fetus’ conditioned worsened over time as is seen in the below strip.
When do variable decelerations become recurrent?
However, variable decelerations become “recurrent” when it is occurring with greater than 50 percent of contractions. This is an example of a Category 3 fetal heart tracing with recurrent variable decelerations.
How long does a variable deceleration last?
The decrease is greater than or equal to 15 beats per minute, lasting greater than or equal to 15 seconds and less than 2 minutes from onset to return to baseline . The onset, depth, and duration of variable decelerations commonly vary with successive uterine contractions.
What are the categories of heart tracings?
Fetal heart tracings into three broad categories: Category 1, Category 2, Category 3.
What is the gray area of ACOG?
While ACOG guidelines for evaluating fetal heart rate tracings exist, there is still a gray area present in the Class II fetal heart tracings and how to manage the fetal heart tracings in the context of the patient. For those who are aware of the recommendations, this gray area of management still leads to variability in how delivery may ensue. This variability is only increased for those who are unaware of ACOG's recommendations and classification guidelines. This, in turn, leads to differences in fetal outcomes and cost of management of the delivery and care of the mother and child after delivery.
How often should a FHR be monitored?
ACOG suggests that these patients be monitored every 30 minutes during the first stage of labor and every 15 minutes during the second stage of labor and changes in management are only necessary if the category of the FHR changes.
What is a Category I FHR?
Category I FHR tracings are normal tracings which are not associated with fetal asphyxia (1). They include a baseline heart rate between 110-160, moderate variability defined as "fluctuations in the baseline heart rate that are irregular in amplitude and frequency of 6-25 bpm", no late or variable decelerations, possible early decelerations, and possible accelerations (1).
Why is FHR tracing so difficult?
Interpretation of fetal heart rate (FHR) tracings has been difficult because of the lack of agreement in definitions and nomenclature. Studies have shown that the interpretation of FHR tracings is unreliable. The American College of Obstetricians and Gynecologists (ACOG) developed a new three-tiered classification system of fetal heart rate abnormalities and a system for interpreting these abnormalities. ACOG published classifications and recommendations based on the appearance of the fetal heart tracing to provide some basis of decision making. Difficulty may exist because the guidelines are not clear-cut and there is room for subjectivity when labeling tracings as a specific category and implementing further medical management. The ACOG guidelines for categorization of fetal heart rate tracings still leave some question as how to definitely label each tracing.
When was the fetal heart rate first measured?
The detection of the fetal heart beat dates back to 1650 with the French physician Marsac (20). Fetal heart rate monitoring during labor was first described by Evory Kennedy, a British physician in 1833 (20). The fetoscope to detect the fetal heart beat was invented by David Hillis in 1917 and Joseph DeLee in 1922 (20). Phonocardiography to detect the fetal heart rate was developed in 1931 (20). In 1958 Edward Hon introduced continuous fetal heart rate (FHR) monitoring to identify heart rate patterns associated with hypoxic changes during labor that caused cerebral palsy and stillbirths so that the baby could be delivered expeditiously when these patterns were present (1, 2, 5, 6). Continuous FMR monitoring was proposed as a screening test for asphyxia to reduce perinatal morbidity and mortality (2, 3, 8, 10). Fetal heart rate monitoring has increased the number of cesarean sections and operative vaginal deliveries but has made no impact on the incidence of cerebral palsy (4, 5, 6). In 1970, intrapartum asphyxia was demonstrated not to be a major cause of cerebral palsy and only accounts for 10% of the cases (3, 5). The incidence of cerebral palsy has remained stable over time at an incidence of 2 in 1,000 live births (3).