
What is cathartic colon and what causes it?
Cathartic colon is nerve damage to the colon due to the abuse of laxatives. The colon wall becomes thin and the colon fails to function properly. Cathartic colon occurs with chronic use of stimulant laxatives (> 3 times per week for at least 1 year).
What are the signs and symptoms of cathartic colon?
Cathartic colon occurs with chronic use of stimulant laxatives (> 3 times per week for at least 1 year). Signs and symptoms of cathartic colon include bloating, a feeling of fullness, abdominal pain, and incomplete fecal evacuation.
Can laxatives cause cathartic colon?
Cathartic colon occurs when there is nerve damage in the bowls. This causes the colon wall to thin out, and in time, the colon will stop functioning. Doctors estimate that using laxatives three or more times per week for a year can cause the condition. Laxatives overstimulate the bowels and irritating the nerves.
What is cathartic colon in bulimia?
Cathartic Colon. A possible complication of bulimia is cathartic colon. In fact, severe constipation or a cathartic colon is one of the clues physicians may have in diagnosing bulimia. Cathartic colon is nerve damage to the colon due to the abuse of laxatives. The colon wall becomes thin and the colon fails to function properly.
Is cathartic colon reversible?
Previous reported cases have shown residual roentgen abnormalities on follow-up examinations. A case is presented of cathartic colon caused by more than 70 years of laxative abuse that demonstrated complete reversal of the roentgen changes four months after stopping the medication.
What is the difference between a laxative and a cathartic?
Laxatives and cathartics are medications that increase the passage of stool. Laxatives ease the passage of fully formed fecal matter from the rectum; while cathartics have a stronger effect, and cause the evacuation of the entire colon, usually in the form of watery, unformed stool.
What are examples of cathartics?
Examples of hyperosmotic cathartics include magnesium salts, sodium salts, and sugar alcohols.Magnesium salts are frequently used PO as saline purgatives. ... Sodium salts can be given PO as saline cathartics but are more commonly administered as sodium biphosphate or sodium phosphate enemas.More items...
What is a cathartic drug?
In medicine, a cathartic is a substance that accelerates defecation. This is similar to a laxative, which is a substance that eases defecation, usually by softening feces. It is possible for a substance to be both a laxative and a cathartic. However, agents such as psyllium seed husks increase the bulk of the feces.
Is Milk of Magnesia a cathartic?
Magnesium sulfate, or Epsom salt, is commonly used as an osmotic cathartic in 6% isotonic solution. Other magnesium-containing cathartics include magnesium hydroxide (milk of magnesia), magnesium oxide, and magnesium citrate.
Is lactulose a stool softener or a laxative?
Lactulose is a synthetic sugar used to treat constipation. It is broken down in the colon into products that pull water out from the body and into the colon. This water softens stools. Lactulose is also used to reduce the amount of ammonia in the blood of patients with liver disease.
Does cathartic mean therapeutic?
Sigmund Freud first used catharsis as a therapeutic method of releasing negative emotions to reduce frustration and feelings of aggression.
What do cathartics do to gastrointestinal transit time?
Cathartics increase the speed and transit time of material in the GI tract, thus promoting fecal excretion of the toxin. More importantly, cathartics decrease the time available for systemic toxin absorption in the GI tract.
Is lactulose a cathartic?
Lactulose is a semisynthetic disaccharide that is not hydrolysed by intestinal enzymes. It acts as an osmotic cathartic and retains water and electrolytes in the lumen of the gut. Further metabolism of this unabsorbed sugar is achieved by colonic bacteria, which release organic acids; these acids then act as laxatives.
What are the two types of cathartics?
The two general types of osmotic cathartics used in poisoned patients are saccharide cathartics (sorbitol) and saline cathartics (magnesium citrate, mag- nesium sulfate, sodium sulfate).
What does catharsis feel like?
A catharsis is an emotional release. According to psychoanalytic theory, this emotional release is linked to a need to relieve unconscious conflicts. For example, experiencing stress over a work-related situation may cause feelings of frustration and tension.
What is the synonym for cathartic?
Synonyms & Near Synonyms for cathartic. cleansing, purificatory, purifying.
What are the two types of cathartics?
The two general types of osmotic cathartics used in poisoned patients are saccharide cathartics (sorbitol) and saline cathartics (magnesium citrate, mag- nesium sulfate, sodium sulfate).
What is difference between laxative and purgative?
Purgatives or cathartic: are stronger action resulting in more fluid evacuation. Laxative and cathartics are used for: Relief of acute non dietary constipation. Removal poisons from the gastrointestinal tract.
Which are commonly used cathartics?
Examples of hyperosmotic cathartics include magnesium salts, sodium salts, and sugar alcohols.Magnesium salts are frequently used PO as saline purgatives. ... Sodium salts can be given PO as saline cathartics but are more commonly administered as sodium biphosphate or sodium phosphate enemas.More items...
What are the types of laxatives?
There are 4 main types of laxatives.Bulk-forming laxatives. Bulk-forming laxatives work by increasing the "bulk" or weight of poo, which in turn stimulates your bowel. ... Osmotic laxatives. ... Stimulant laxatives. ... Poo-softener laxatives.
What is the best way to reduce bowel movement?
Fiber adds bulk to your stool. This can reduce the chances for loose stool or alternating bowel movement consistency. Fiber is found in fruits, vegetables, whole grains, beans, and legumes. Cutting back on fat may also reduce colon irritation. These changes may ease colon spasms and prevent contractions in the future.
What causes a spasm in the colon?
IBS is the most common underlying health condition that can cause colon spasms. Other conditions may also cause these contractions. These include: ulcerative colitis. Crohn’s disease . distended, or enlarged, colon.
Why do I have a spasm in my colon?
Colon spasms can also occur for no identifiable reason. A colon’s muscles contract to help move feces along the lower portion of the gastrointestinal (GI) tract. During a colon spasm, the muscles lining the colon tighten or contract in an unorganized way. These contractions are often painful and obvious, while normal contractions are rarely ...
What is the best medicine for colon spasms?
Antispasmodic medication. These medications are designed to calm muscles and reduce the severe contractions from colon spasms.
How to prevent colon spasms?
Manage stress. Learn to manage stress and reduce its impact on your mental and physical health when it occurs. This may help prevent future colon spasms.
What side of the colon does it hurt?
Pain. Sudden severe abdominal pain, especially in the lower abdomen and on the left side, is common with colon spasms. The pain can vary in its intensity with each spasm.
Can you pass stool if you have a colon spasm?
Fluid and stool buildup in your intestines can be a life-threatening condition if it’s not treated properly and quickly. However, if you’re experiencing frequent colon spasms or other symptoms, check in with your doctor. They can look for a possible explanation.
Word History of Catharsis and Cathartic
Catharsis and cathartic both trace to the Greek word kathairein, meaning “to cleanse, purge.” Catharsis entered English as a medical term having to do with purging the body—and especially the bowels—of unwanted material. The adjective cathartic entered English with a meaning descriptive of such a physically cleansing purge.
Examples of cathartic in a Sentence
Adjective There's something cathartic about a punch in the nose. — Michael Farber, Sports Illustrated, 28 Jan. 2002 But Vietnam is hard to sell as a tidy, cathartic morality tale of troubled times overcome. — Jennifer Homans, New Republic, 2 & 9 Dec. 2002
Is tegaserod a laxative?
Tegaserod is the only US FDA-approved treatment for chronic constipation. (ie, most laxatives are only approved for short-term use in the treatment of occasional constipation). For chronic constipation, tegaserod is approved for chronic use (longer than 12 weeks) with periodic reassessment by the physician to confirm the need for ongoing therapy. Unlike the IBS indication which is only for women, tegaserod is approved for the treatment of chronic constipation in men as well, because subgroup analysis in male patients demonstrated superiority of effect for tegaserod-treated patients vs placebo-treated patients. However, efficacy has not been demonstrated in patients 65 years of age and older, and therefore tegaserod is only FDA-approved for the management of chronic constipation in men and women younger than 65 years. RCT data also demonstrated improvements in total spontaneous bowel movements, complete spontaneous bowel movements, straining, and other individual symptoms of chronic constipation.
Is polyethylene glycol better than placebo?
Multiple well-designed RCTs, [14-17] demonstrate that polyethylene glycol appears superior to placebo for improving stool frequency and stool consistency in patients with chronic constipation (Grade A recommendation; Grade A recommendations are supported by 2 or more well-designed RCTs with adequate sample sizes and statistically significant results). Lactulose is also more effective than placebo in improving stool frequency and stool consistency in chronic constipation patients (Grade A recommendation). [18-20] However, only 1 RCT [21] assessed the efficacy of magnesium hydroxide in patients with chronic constipation, and this trial was not placebo-controlled. Therefore, Task Force members stated that there are insufficient data to make a recommendation about the effectiveness of magnesium hydroxide in patients with chronic constipation.
Does psyllium help with constipation?
Findings from 3 placebo-controlled randomized controlled trials (RCTs) showed that psyllium improves stool frequency and stool consistency compared with placebo. [4-6] These trials were suboptimally designed, which led to a grade B recommendation (ie, recommendations based on evidence from RCTs with inadequate sample sizes, inappropriate methodology, or nonsignificant results). There are insufficient data to make a recommendation about the efficacy of calcium polycarbophil, methylcellulose, and wheat bran in patients with chronic constipation. Specifically, there are 3 RCTs of wheat bran in patients with chronic constipation, [7-9] but only 1 is placebo-controlled. [7] This trial did not demonstrate a significant improvement in stool frequency or consistency when compared with placebo -- neither did 2 trials [8,9] that compared wheat bran with corn biscuit or corn bran. There are no placebo-controlled RCTs of methylcellulose or calcium polycarbophil, although poorly designed RCTs involving fewer than 100 patients do not demonstrate differences between calcium polycarbophil or methylcellulose compared with psyllium.
Does psyllium cause bloating?
Data on adverse events are quite limited, although taking 10-20 g/day of psyllium has been associated with bloating, which may be a bothersome event in these patients. Psyllium has also been associated with mechanical obstruction of the esophagus and colon and anaphylactic reactions in case reports.
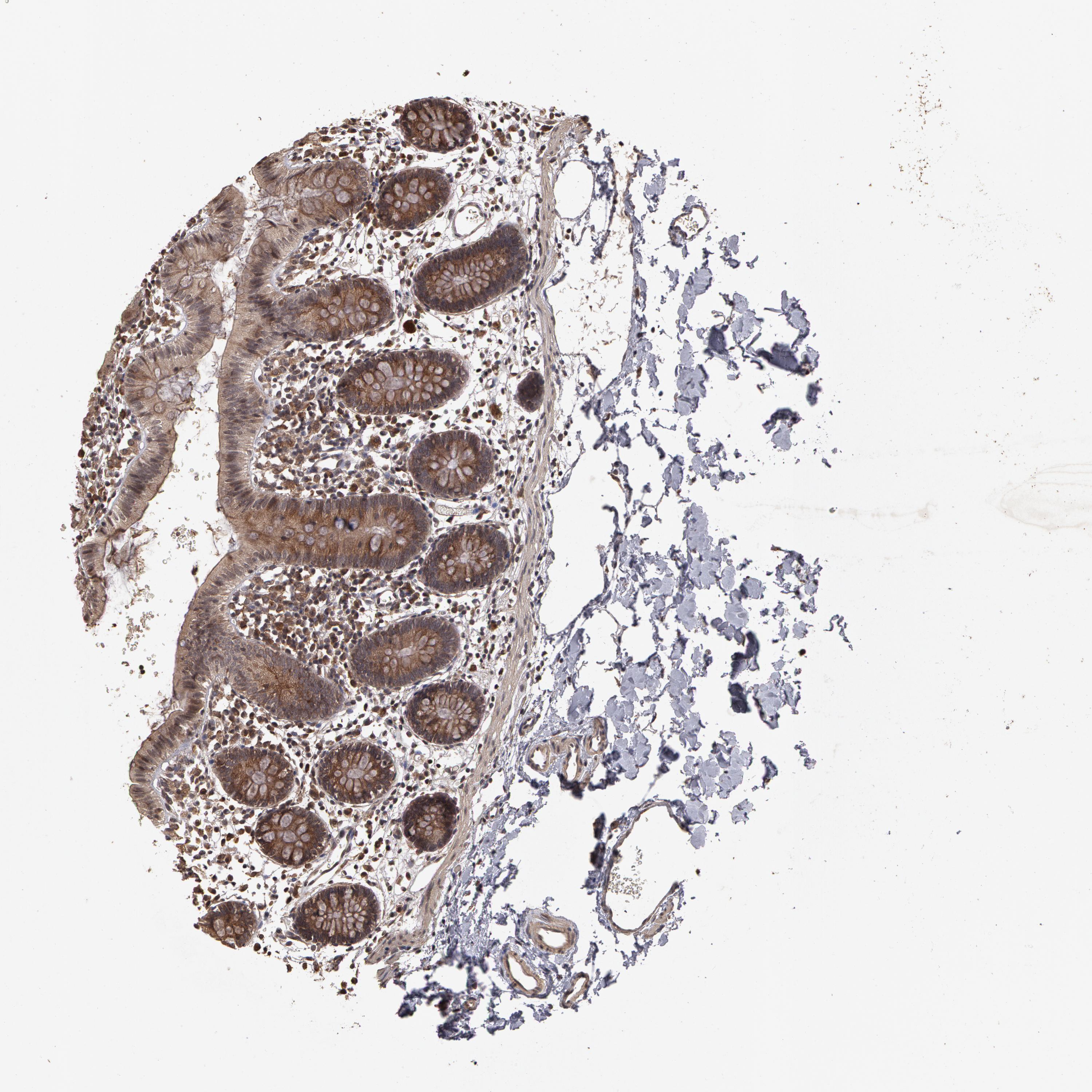
Can stimulant laxatives cause melanosis?
Senna-containing stimulant laxatives have been associated with melanosis coli. However, available evidence does not indicate that melanosis coli is associated with defects in colon physiology. Although cathartic colon (a syndrome characterized by colonic dilatation and loss of haustration) has been reported in patients using stimulant laxatives, this entity has not been reported in long-term users of currently available stimulant laxatives. Thus, it is unlikely that the long-term use of stimulant laxatives induces a permanent injury to colonic mucosa or to the enteric nervous system.
Does lactulose cause diarrhea?
Data on adverse events were not adequately reported for most of these trials. However, lactulose-treated patients demonstrated a significant increase in bloating/abdominal discomfort compared with placebo-treated patients. Polyethylene glycol was associated with diarrhea. Review of available adverse event data indicates that the prevalence of diarrhea in polyethylene glycol-treated patients ranged from 2% to 40% in clinical trials.
Is Dipalma a placebo controlled study?
DiPa lma JA, DeRidder JH, Orlando RC, Kolts BE, Cleveland MB. A randomized, placebo-controlled, multicenter study of the safety and efficacy of a new polyethylene glycol laxative. Am J Gastroenterol. 2000;95:446-450. Abstract
