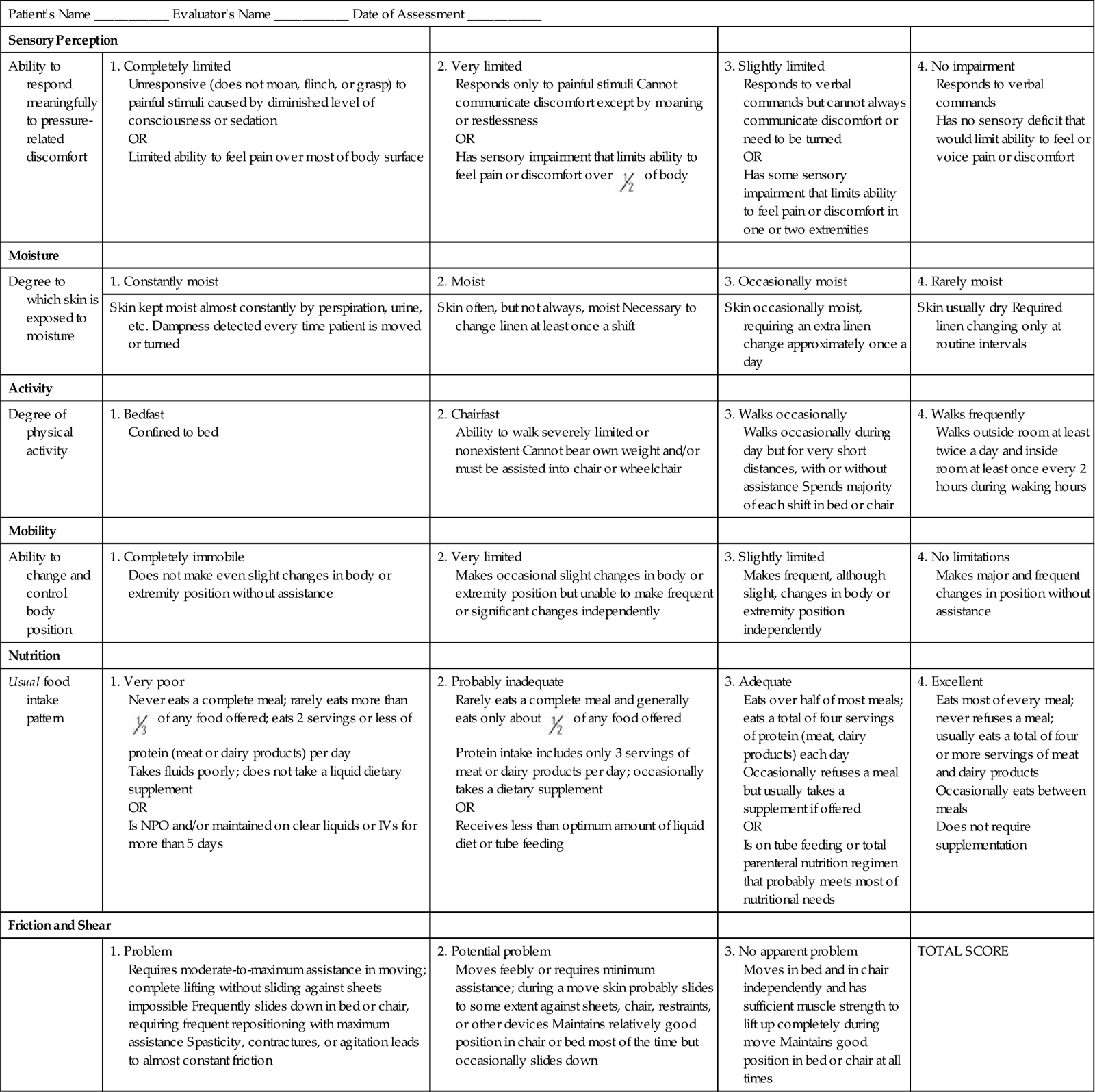
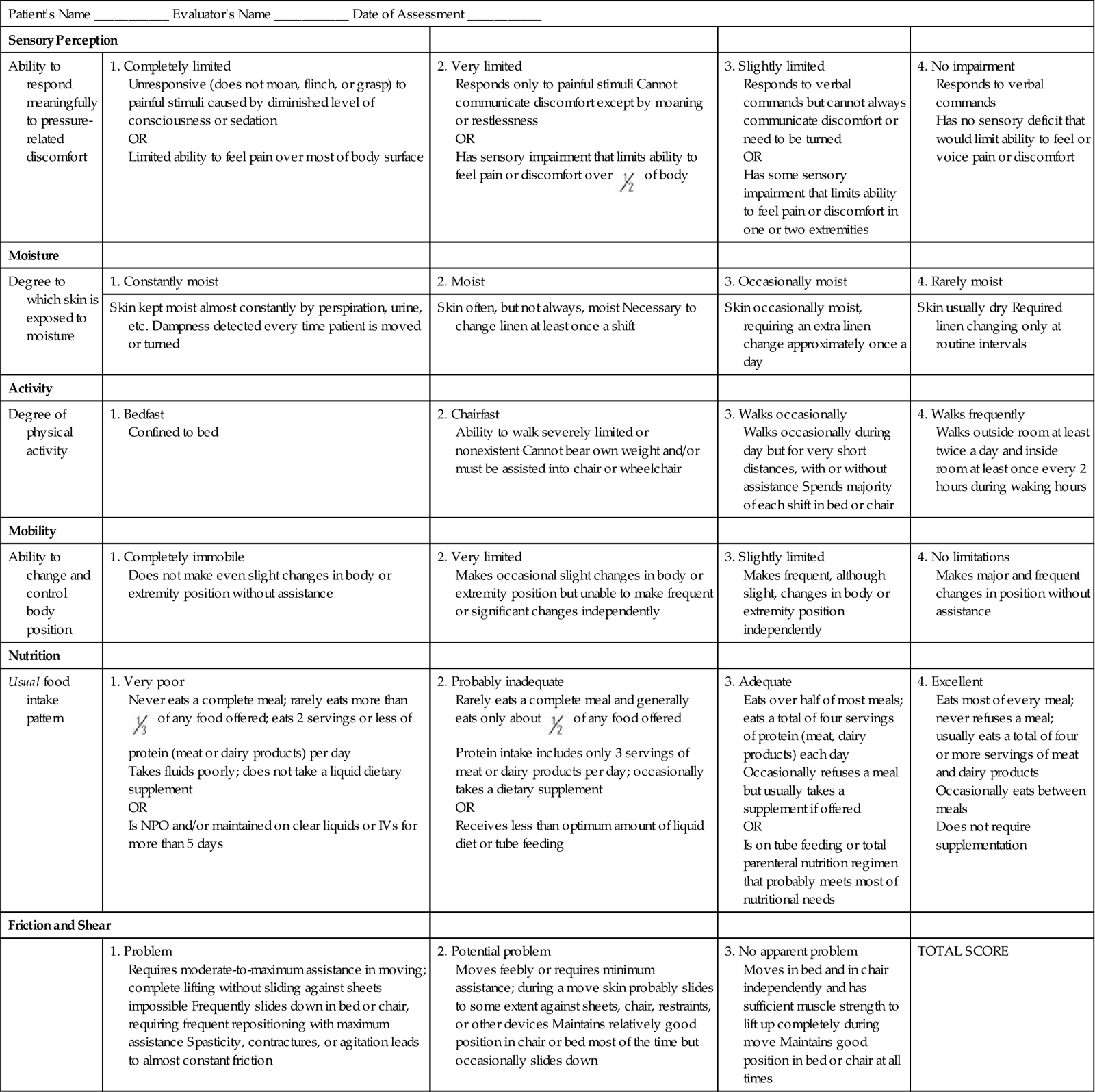
The braden score consists of 6 categories: sensory perception, moisture, activity, mobility, nutrition and friction. The score ranges from 6-23 with lower scores indicating a higher risk. The Braden scores gathered by nurses for every patient in the study will be compared to each patient's Fitbit data to assess for accuracy and consistency.
What is the maximum score on the Braden scale?
The maximum score on the Braden scale is 23. A score of 16 or less indicates a higher risk of pressure ulcers. A risk assessment scale should be completed on admission to a care facility and then on a regular schedule for surveillance. View chapter Purchase book
What is the Braden scale for ulcers?
Simply put, the Braden Scale is a test developed to help professionals, especially nurses and caretakers, asses the patient's risk of developing a pressure ulcer by examining six criteria. The total score can range from six to 23, with the lower score indicating a higher risk.
What is the Braden scale score for pressure injuries?
The Braden Scale can have a score from 6 to 23. The lower the score, the greater the risk for developing a pressure injury. But it’s important to remember that this score is the sum of six subscores from six subscales that measure sensory perception, moisture, activity, mobility, nutrition, and friction and shear.
What are the Norton and Braden scales?
The Norton and Braden scales are validated tools to assess pressure ulcer risk.6 Each scale quantifies risk factors and sums the risk factors to assign an overall risk score for pressure ulcer development. The Norton scale evaluates physical condition, metal condition, activity, mobility, and incontinence as risk factors.

What is the normal range for Braden Scale?
Braden total scores range from 6 to 23 points with lower scores indicating a higher risk for presses ulcers.
What does a Braden score of 7 mean?
13-14 – moderate risk. 10-12 – high risk. 6-9 – very high risk. Page 14. Braden Score 15-18 Preventative.
What does Braden score of 11 mean?
Any use of the form in publications (other than internal policy manuals and training material) or for profit-making ventures requires additional permission and/or negotiation. SEVERE RISK: Total score 9 HIGH RISK: Total score 10-12. MODERATE RISK: Total score 13-14 MILD RISK: Total score 15-18.
What is high risk on Braden Scale?
Mild risk: 15-18. Moderate risk: 13-14. High risk: 10-12. Severe risk: less than 9.
What does a Braden score of 19 mean?
The Braden Scale uses a scores from less than or equal to 9 to as high as 23. The lower the number, the higher the risk is for developing an acquired ulcer or injury. 19-23 = no risk. 15-18 = mild risk. 13-14 = moderate risk.
What is a high fall risk score?
A patient who scores under 25 points is considered to be at low risk of falling, a patient who scores between 25–45 points is considered to be at moderate risk of falling, and a patient who scores higher than 45 points is considered to be at high risk of falling.
What is the Braden Scale in nursing?
The Braden Scale for Predicting Pressure Sore Risk was developed to foster early identification of patients at risk for forming pressure sores. The scale is composed of six subscales that reflect sensory perception, skin moisture, activity, mobility, friction and shear, and nutritional status.
What is the lowest Braden score?
Each subscale within the Braden Scale contains a numerical range of scores, with 1 being the lowest score possible. The friction/shear subscale ranges from 1 to 3; the other subscales range from 1 to 4.
How do you calculate bed sores?
Just count patients, not the number of ulcers. Even if a patient has four Stage II ulcers, he or she is only counted once. The denominator is the number of patients on your unit or in your facility during that month. Divide the numerator by the denominator and multiply by 100 to get the percentage.
What Is a Stage 2 wound?
At stage 2, the skin breaks open, wears away, or forms an ulcer, which is usually tender and painful. The sore expands into deeper layers of the skin. It can look like a scrape (abrasion), blister, or a shallow crater in the skin. Sometimes this stage looks like a blister filled with clear fluid.
What is the Braden Scale in nursing?
The Braden Scale for Predicting Pressure Sore Risk was developed to foster early identification of patients at risk for forming pressure sores. The scale is composed of six subscales that reflect sensory perception, skin moisture, activity, mobility, friction and shear, and nutritional status.
How do you calculate bed sores?
Just count patients, not the number of ulcers. Even if a patient has four Stage II ulcers, he or she is only counted once. The denominator is the number of patients on your unit or in your facility during that month. Divide the numerator by the denominator and multiply by 100 to get the percentage.
How are bed sores measured?
Pressure ulcer areas were measured using 3 techniques: measurement with a ruler (wound area was calculated by measuring and multiplying the greatest length by the greatest width perpendicular to the greatest length), wound tracing using graduated acetate paper, and digital planimetry.
What is a pressure ulcer?
Listen to pronunciation. (PREH-sher UL-ser) Damage to an area of the skin caused by constant pressure on the area for a long time. This pressure can lessen blood flow to the affected area, which may lead to tissue damage and tissue death.
What is Braden scale?
What is the Braden Scale? If you or someone you are caring for is temporarily or permanently confined to a bed or wheelchair, pressure sores are a real possibility you want to avoid at all costs . Pressure sores, also known as pressure ulcers, pressure injuries, bedsores or decubitus ulcers, occur due to pressure applied to soft tissues, ...
What does a score of 23 mean?
A score of 23 means there is no risk for developing a pressure ulcer, while a lower score signifies a possible problem. The Braden Scale assessment score scale is as follows:
How to Score the Braden Scale
Each risk factor on the Braden Scale is rated from 1 to 4 based on the patient’s assessment findings. When using the Braden Scale, start with the first category and review each description listed across the row for each of the ratings from 1 to 4, and choose the one that best describes the patient’s current status.
Sensory Perception
The sensory perception risk factor is defined as the ability to respond meaningfully to pressure-related discomfort. If a patient is unable to feel pressure-related discomfort and respond to it appropriately by moving or reporting pain, they are at high risk of developing a pressure injury.
Moisture
The moisture risk factor is defined as the degree to which skin is exposed to moisture. Prolonged exposure to moisture increases the probability of skin breakdown. Moisture can come from several sources, such as perspiration, urine incontinence, stool incontinence, or wound drainage.
Activity
The activity risk factor is defined as the degree of physical activity. For example, walking or moving from a bed to a chair reduces a patient’s risk of developing a pressure injury by redistributing pressure points and increasing blood and oxygen flow to areas at risk.
Mobility
The mobility risk factor is defined as the patient’s ability to change or control their body position. For example, healthy people frequently change body position by rolling over in bed, shifting weight in a chair after sitting too long, or by moving their extremities.
Nutrition
Adequate nutrition and fluid intake are vital for maintaining healthy skin. Protein intake, in particular, is very important for healthy skin and wound healing. The nutrition risk factor is defined by two categories of descriptions. The first category measures the amount and type of oral intake.
Team Member Roles to Prevent Pressure Injuries
Each member of the health care team has an important role in preventing the development of pressure injuries in at-risk patients. A registered nurse can delegate many interventions for preventing and treating a pressure injury to a licensed practical nurse (LPN) or to unlicensed assistive personnel such as a certified nursing assistant (CNA).
Why elevating the Braden Scale from routine task to top tool helps nurses better understand and prevent pressure injuries
You have a variety of tools for helping to prevent, assess and treat pressure injuries. The focus of this story: the Braden Scale for Predicting Pressure Sore Risk.
5 Ways to elevate the Braden Scale
Use the subscales The Braden Scale can have a score from 6 to 23. The lower the score, the greater the risk for developing a pressure injury. But it’s important to remember that this score is the sum of six subscores from six subscales that measure sensory perception, moisture, activity, mobility, nutrition, and friction and shear.
Make the most of the Braden Scale
The Braden Scale is a staple of wound assessment; knowing how to make the most of it can help frontline nurses make the right decisions on preventing and treating pressure injuries. For more best practices, tools and education surrounding wound care, visit Medline University.
How to Score The Braden Scale
Sensory Perception
- The sensory perception risk factor is defined as the ability to respond meaningfully to pressure-related discomfort. If a patient is unable to feel pressure-related discomfort and respond to it appropriately by moving or reporting pain, they are at high risk of developing a pressure injury. This risk category describes two different issues that affect sensory perception. The first descri…
Moisture
- The moisture risk factor is defined as the degree to which skin is exposed to moisture. Prolonged exposure to moisture increases the probability of skin breakdown. Moisture can come from several sources, such as perspiration, urine incontinence, stool incontinence, or wound drainage. Frequent surveillance, removal of wet or soiled linens, and use of protective skin barriers greatly …
Activity
- The activity risk factor is defined as the degree of physical activity. For example, walking or moving from a bed to a chair reduces a patient’s risk of developing a pressure injury by redistributing pressure points and increasing blood and oxygen flow to areas at risk. Level of activity is defined by how frequently the patient is able to get out of bed, move into a chair, or am…
Mobility
- The mobility risk factor is defined as the patient’s ability to change or control their body position. For example, healthy people frequently change body position by rolling over in bed, shifting weight in a chair after sitting too long, or by moving their extremities. However, tissue damage will occur if a patient is unable to reposition on their own power unless caregivers frequently change their …
Nutrition
- Adequate nutrition and fluid intake are vital for maintaining healthy skin. Protein intake, in particular, is very important for healthy skin and wound healing. The nutrition risk factor is defined by two categories of descriptions. The first category measures the amount and type of oral intake. The second category is used for patients receiving tube feeding, total parenteral nutrition (TPN), …
Friction/Shear
- Friction and shear are significant risk factors for producing pressure injuries. This category only has three ratings, unlike the other categories that have four ratings, and is rated by whether the patient has a problem, potential problem, or no apparent problem in this area. See Table 10.5f for interventions for each level of risk. Table 10.5f Descriptions and Interventions by Level of Risk fo…
Team Member Roles to Prevent Pressure Injuries
- Each member of the health care team has an important role in preventing the development of pressure injuries in at-risk patients. A registered nurse can delegate many interventions for preventing and treating a pressure injury to a licensed practical nurse (LPN) or to unlicensed assistive personnel such as a certified nursing assistant (CNA). See Table 10.5g for an explanati…