Ray amputation of the hallux disrupts the medial column of the foot and should be performed only after careful consideration. The removal of a single metatarsal in the middle of the foot (ie, the second, third, or fourth metatarsal) results in a V-shaped wedge, which again maintains good function.
Full Answer
What is hallux amputation for diabetic osteomyelitis?
Hallux amputation for diabetic osteomyelitis Digital amputation for infection in the diabetic patient requires accurate assessment of wound healing potential as a function of clinical and noninvasive studies of cutaneous blood flow. The diabetic propensity for staphylococcal infection, microangiopathy, and delayed wound healing may be question …
What are the treatment options for left hallux amputation?
Left hallux amputation. Monitored anesthesia care with local consisting of 12 mL of 1:1 mixture of 2% lidocaine plain with 0.5% Marcaine plain injected in a nail block fashion. Left pneumatic ankle tourniquet set at 250 mmHg. Less than 5 mL. None. None. None. Left hallux sent for culture and pathology.
Does amputation of the hallux cause an apropulsive gait?
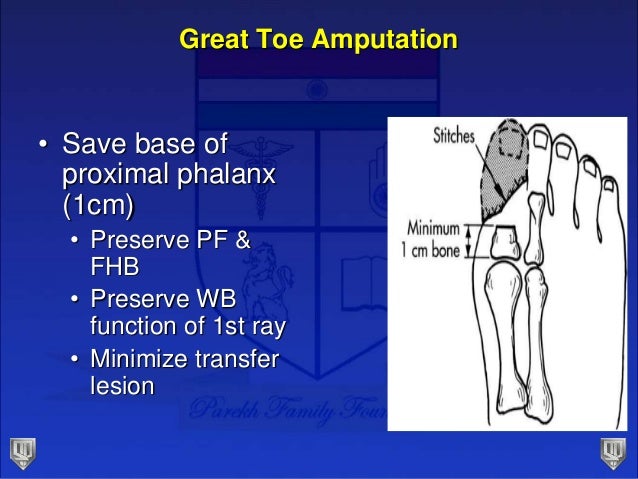
Therefore, amputation of the hallux often causes an apropulsive gait.4 The degree of biomechanical dysfunction depends upon the level of amputation. The anatomy of the hallux is different from the lower toes and should have a fast review.
How much lidocaine is used in left hallux amputation?
Left hallux amputation. Monitored anesthesia care with local consisting of 12 mL of 1:1 mixture of 2% lidocaine plain with 0.5% Marcaine plain injected in a nail block fashion. Left pneumatic ankle tourniquet set at 250 mmHg.

What causes hallux rigidus in big toe?
Injury. Injuries, such as stubbing your toe or spraining the joint in your big toe, can contribute to hallux rigidus. Overuse. Regularly stooping and squatting can cause overuse of the joint in your big toe.
How old do you have to be to get hallux rigidius?
Anyone can develop hallux rigidius, but it tends to affect people between the ages of 30 and 60.
What is joint fusion surgery?
This type of surgery is also known as joint fusion. It’s used to treat advanced hallux rigidus involving severe joint damage.
What is the procedure to remove a spur on the top of your big toe called?
Cheilectomy. This type of surgery is used to treat mild to moderate damage. It involves shaving any bone spurs. A cheilectomy may also be performed in combination with another procedure called osteotomy. This cuts the bone to change the position of your big toe and relieve pressure on top of the joint.
Why do doctors move my big toe?
They may move your big toe around a bit to rule out any other potential causes of your symptoms. Based on what they see during the exam, your doctor might order an X-ray of your foot or toe. This will allow them to see any damage to the joint in your big toe.
What is the procedure to replace a joint?
Arthroplasty. This is joint replacement surgery. It entails replacing one or both sides of your joint with artificial joints made of plastic or metal. The goal of this surgery is to relieve your symptoms while maintaining motion of your joint.
Is hallux rigidus more common in females?
There’s no known cause of hallux rigidus, but several risk factors have been identified. Risk factors include: Being female. Hallux rigidus is more common in females. Of the 110 participants included in a 2009 cross-sectional study on the demographics of hallux rigidus, 66 percent were female. Family history.
What is the role of the hallux in amputation?
Relevant Insights On Performing A Hallux Amputation. The hallux plays an important role in supporting the medial element of the foot and the extensor hallucis longus (EHL) is one of the most essential extrinsic muscles of the foot throughout the swing phase of gait.
What are the advantages of distal amputation?
Distal amputations are more practical and have numerous physiological benefits such as energy preservation throughout ambulation.
Why do we resect the distal phalanx?
Commonly, we are forced to resect more of the phalanges in order to obtain tension totally free closure. However, this usually happens in patients who have osteomyelitis of the distal phalanx or those in whom the dorsal and/or plantar skin has necrosis that extends to the level of the proximal interphalangeal joint. This circumstance forces us to resect the non-infected bone in order to get to the sensible dorsal and plantar skin of the toe. Surgeons should prevent stress at the cut website to prevent dehiscence.
Why do you leave a stump of the 2nd, 3rd, or 4th toe undamaged?
Leaving a stump of the 2nd, third or 4th toe undamaged enables the stump to function as a buttress, avoiding the nearby toes from establishing a shift in the transverse aircraft . Amputations of minimal numbers generally result in a gait with very little to no disruption.
What is the best cut for a partial toe amputation?
The preferred cut for a partial toe amputation is a transverse fish-mouth cut, which tends to give the best outcome both cosmetically and functionally.
Can a patient with a toe pressure of 40 mmHg heal?
So does this mean that patients with pressures of 40 mmHg and below will not be able to heal? The basic response is that some patients will be able to heal and some patients will not. It is our suggestion that anyone with toe pressures of less than 40 mmHg should undergo a vascular workup for a possible revascularization. Nevertheless, we all see patients who are too frail or too old, and are not prospects for revascularization. It is these patients– whose toe pressures are less than 40 mmHg and who are not candidates for revascularization — whom we have to evaluate and figure out whether their digital amputation will recover.
Can diabetics have amputations?
In specific patients, an optional partial toe amputation with diabetes might be suggested. These patients who do not have an active infection might suffer from a stiff hammertoe deformity with a non-healing ulcer on the pointer of their toe. In these situations, partial digital amputation would deal with the hammertoe deformity and the non-healing ulcer at the exact same time. A candidate for this type of a procedure would be a patient who is senior, someone who has multiple comorbidities or a specific with very little mobility who would gain from a fast and simple procedure with minimal postoperative healing time.
What is amputation treatment?
Amputation should be considered a treatment. It is a method of increasing the patient's ability to ambulate. If the patient has no chance of ambulating with a par- tial amputation, then a more proximal amputation should be considered. Every consideration should be given to maximizing the function of the remaining portion of the extremity while considering, at the same time, its viability. The level of the foot amputa- tion is dependent upon many variables. Invasive and noninvasive vascular testing along with the surgeon's subjective and objective clinical evaluation of other factors such as neuropathy, infection, necrosis, malig- nancy, function, and rehabilitation determine the most appropriate level of amputation and necessary modifi- cations. All amputations should be approached with the knowledge that a more proximal amputation may be necessary once the surgical intervention begins. Sur- prises are not uncommon. Devitalized necrotic tissue may be hidden by a superficial flap that appears viable. At this point, the surgical experience and creativity of the surgeon is put to a test. All nonviable tissue must be removed. As the surgery proceeds, modifications and various plastic revisions are designed to over- come problems of atypical anatomy. In the following descriptions of various types of am- putations, certain rules are common to all. In general, the more distal the site of amputation the more func- tional the foot remains. Skin flaps should not be undermined layer by layer. They should be dissected from the bone as one thick combination layer of skin, subcutaneous tissue, and muscle. Nonviable tissue obviously has to be dissected from the flap. Flaps should be as broad based as possi- ble to avoid compromising the blood supply. Al- though they are full thickness, the edges should not be bulky or redundant.2
Why are partial amputations used?
In addition to the causes just noted, amputation is also used to treat trauma, malignancies, congenital and acquired deformities, and even cosmesis.1
What is the best technique for amputation of a lesser toe?
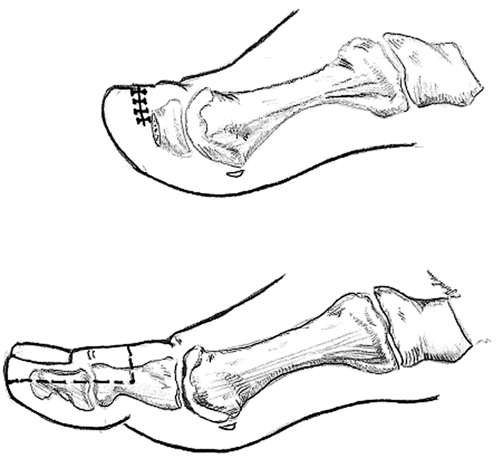
When lesser toes are individually amputated, several techniques may be applied. The significant fact to re- member is that any closure of the amputated stump should be tension free. Whether one uses a plantar flap, a dorsal flap, variations of side flaps, or elliptical incisions, lack of tension is the most significant techni- cal requirement for success in an amputation where all other preoperative criteria were fulfilled. The technical approach to the amputation varies with the incision line. The optimal site for a digital amputation is at the level of the metatarsophalangeal joint. The choice of incision depends on the anatomy of the forefoot. Whether the incision is elliptical or flap, the surgical approach after the incision is basi- cally the same. My preference is to perform this amputation with a tear-shaped incision in the web around the toe (Fig. 32-2). The apex of the incision is dorsal. The dorsal part of the incision is carried proximally over the metatarsophalangeal joint. With sharp and blunt dis- section, the surrounding skin and subcutaneous tissue are reflected aside. All bleeders are cauterized. The extensor and flexor tendons are pulled distally and severed at their most proximal portion in the wound. The capsule is then incised, allowing the surgeon to remove the toe in toto. If dead space is a concern, the base of the proximal phalanx may be left intact. If there is redundant subcutaneous tissue, it is dis- sected out of the wound. However, in most cases this is not the fact. Nonviable tissue isremoved. If it is determined that the nonviable tissue continues proxi- mally, a more radical amputation (i.e., ray amputation or possibly transmetatarsal amputation) should be considered at this time. If all nonviable tissue is ade- quately removed from the wound, the subcutaneous tissue can be approximated over the metatarsal head with absorbable sutures. This acts as a cushion. It is my preference to leave the cartilage on the metatarsal head intact; I only remove the cartilage when it shows signs of nonviability. The skin is approximated with a nonabsorbable suture (i.e., prolene or ethilon). Verti- cal mattress sutures interspersed withsimple inter- rupted sutures allow for an adequate closure without tension. The wound is then dressed with betadine-soaked sterile dressings followed by dry sterile fluff and mild
How to amputation a cuboid?
AMPUTATION OF THE FOOT 479 the cuboid should be beveled in such a manner as to avoid friction on ambulation. All nerves should be severed proximal to the inci- sion. Tendons should be pulled distally and severed at their most proximal exposure and then allowed to retract out of the amputation site. Ulcers and nonvia ble tissue should be removed from the surgical site. The dorsal and plantar flap can then be revised in the best possible manner allowing for the final repair to be performed dorsally. As before, dog ears are avoided by bringing the dorsal and plantar incisions together on the medial and lateral aspect in a sharp corner. No tension should be allowed at the incision site. Number 2-0 nonabsorbable (ethilon, prolene) vertical mattress sutures should be used to approximate the skin and subcutaneous tissue. All sutures should be placed approximately 1 cm. apart. As before, I use drains only when I judge that it is necessary for the removal of exudate and blood. The 1 cm. gapping be- tween sutures allows for most drainage to be elimi- nated throughout the incision line. The wound is dressed with betadine-soaked sterile dressings fol- lowed by dry sterile fluff and mild compression. Early ambulation is prohibited. The sutures remain intact for at least 4 weeks. Ambulation is allowed only after the sutures are removed and the incision line is intact. Exercises are permitted for range of motion at the ankle level while the extremity is elevated. Postoperatively, complications have occurred with this type of disarticulation. Equinovarus is a common post-operative problem leading to ulcers and tyloma on the distal aspect of the foot and the incision line.7
What should be done after amputation?
Early weight-bearing will negate the best surgical technique. However, range-of-motion exercises and muscle strengthening can be started at an early stage. It should be noted that not all amputations can be finished with primary closure. At times, the wound must be packed open and a second or third surgery will be necessary to debride infected and nonviable tissue before closure. When this is the case, the origi- nal flaps should be approximately 20 percent longer than would be used to cover the stump in primary closure; this allows for shrinkage of the flaps.3
What is a Syme terminal amputation?
The Syme terminal amputation has been used by many surgeons to overcome an onychauxic or mycotic and ingrown nail. The procedure includes the radical exci-sion of the matrix, nail, and nailbed along with the distal half of the distal phalanx (Fig. 32-1).
Can you have a partial foot amputation?
With the increasing success rate of various treatments for dysvascular limbs, partial amputations of the foot are becoming much more frequent. Peripheral vascu- lar disease, neuropathy, severe infection, diabetes, and trauma do not require a patient to undergo a below- knee or above-knee amputation as often as in the past. More aggressive vascular surgery, plastic reconstruc- tive surgery (i.e., flaps), and medication allow the phy- sician to improve the chance of success for a partial amputation of the foot.