Is hyperosmolar and hypertonic the same thing?
Hypertonic vs Hyperosmotic - What's the difference? is that hypertonic is (of a solution) having a greater osmotic pressure than another while hyperosmotic is hypertonic.
Do people recover from a diabetic coma?
People who receive emergency treatment for a diabetic coma usually recover fully. Your doctor may recommend that you wear a medical identification bracelet that explains the nature of your diabetes and other health concerns. This may help ensure you get the proper treatment for future problems quickly.
Can you die from a diabetic coma?
Diabetic coma is a serious complication that can be fatal. And the odds of death increase the longer you wait for treatment. Waiting too long for treatment can also lead to brain damage. This diabetic complication is rare.
What is treatment for diabetic coma?
Treatment options for diabetic coma include:
- ketoacidotic coma – intravenous fluids, insulin and administration of potassium
- hyperosmolar coma – intravenous fluids, insulin, potassium and sodium given as soon as possible
- hypoglycaemic coma – an injection of glucagon (if available) to reverse the effects of insulin or administration of intravenous glucose.

What does it mean to be hyperosmolar?
This is called hyperosmolarity. It is a condition in which the blood has a high concentration of salt (sodium), glucose, and other substances. This draws the water out of the body's other organs, including the brain. Risk factors include: A stressful event such as infection, heart attack, stroke, or recent surgery.
What are the symptoms of hyperosmolar coma?
A serious complication of diabetes mellitus, hyperosmolar hyperglycemic syndrome (HHS) happens when blood sugar levels are very high for a long period of time. Symptoms of HHS can include extreme thirst, frequent urination, changes in your vision and confusion.
What causes hyperosmolar?
Common precipitating causes of HHS include unknown diabetes or inadequate diabetic treatment, infections, myocardial infarction and other vascular events, drugs and medications, and pancreatitis.
What is a hyperosmolar state?
Hyperosmolar hyperglycemic state is a life-threatening emergency manifested by marked elevation of blood glucose and hyperosmolarity with little or no ketosis. Although there are multiple precipitating causes, underlying infections are the most common.
What is the highest blood sugar ever recorded?
2,656 mg/dlMichael Patrick Buonocore (USA) (b. 19 May 2001), survived a blood sugar level of 147.6 mmol/L (2,656 mg/dl) when admitted to the Pocono Emergency Room in East Stroudsburg, Pennsylvania, USA, on 23 March 2008. The normal blood sugar range is between 4.4 to 6.6 mmol/L (80-120 mg/dl).
What happens when you go into a diabetic coma?
If you go into a diabetic coma, you're alive — but you can't wake up or respond purposefully to sights, sounds or other types of stimulation. If it's not treated, a diabetic coma can result in death.
How is hyperosmolar diagnosed?
Hyperosmolar hyperglycemic state is diagnosed by blood tests that show very high levels of glucose and very concentrated blood. Treatment is intravenous fluids and insulin. Complications include coma, seizures, and death.
How does Hyperosmolarity cause altered mental status?
Patients with HHS can present with altered mental status as a result of significant fluid depletion and decreased cerebral perfusion. A good rule of thumb is to secure the airway if the Glasgow coma score is less than 8.
What causes the coma in Nonketotic hyperglycemic hyperosmolar coma?
Causes of hyperglycaemic hyperosmolar non-ketotic coma may include undiagnosed type 2 diabetes that has been developing over a number of years. Alternatively, HONK could be brought on by diabetic medication not being taken or very high blood glucose resulting from a period of illness.
Which symptoms does the nurse observe in a client with hyperosmolar hyperglycemic syndrome?
Patients with hyperglycemia may also exhibit a non-ketotic hyperosmolar state, also known as hyperglycemic hyperosmolar syndrome (HHS)....HyperglycemiaIncreased urination/output (polyuria)Excessive thirst (polydipsia)Increased appetite (polyphagia), followed by lack of appetite.Weakness, fatigue.Headache.
Which condition is seen in a patient with hyperosmolar hyperglycemic syndrome HHS?
Hyperosmolar hyperglycemic state is a metabolic complication of diabetes mellitus characterized by severe hyperglycemia, extreme dehydration, hyperosmolar plasma, and altered consciousness. It most often occurs in type 2 diabetes, often in the setting of physiologic stress.
Which is worse DKA or HHS?
DKA typically affects people living with type 1 diabetes, whereas HHS usually occurs in people living with type 2 diabetes. HHS tends to be more dangerous than DKA, but both conditions can be deadly if a person does not receive treatment. Prompt medical attention is necessary in both cases.
Which condition is seen in a patient with hyperosmolar hyperglycemic syndrome HHS?
Hyperosmolar hyperglycemic state is a metabolic complication of diabetes mellitus characterized by severe hyperglycemia, extreme dehydration, hyperosmolar plasma, and altered consciousness. It most often occurs in type 2 diabetes, often in the setting of physiologic stress.
How is hyperosmolar hyperglycemic state diagnosed?
Hyperosmolar hyperglycemic state is diagnosed by blood tests that show very high levels of glucose and very concentrated blood. Treatment is intravenous fluids and insulin. Complications include coma, seizures, and death.
What would one expected assessment finding for hyperglycemic hyperosmolar syndrome?
Physical exam findings and signs related to HHS include the following: Altered mental status, confusion. Lethargy. Ill appearance.
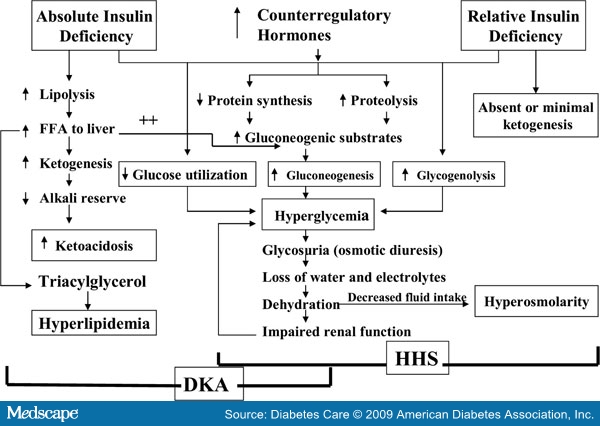
What is the main difference between DKA and HHS?
DKA is characterized by ketoacidosis and hyperglycemia, while HHS usually has more severe hyperglycemia but no ketoacidosis (table 1). Each represents an extreme in the spectrum of hyperglycemia. The precipitating factors, clinical features, evaluation, and diagnosis of DKA and HHS in adults will be reviewed here.
What is hyperosmolar hyperglycemic syndrome?
Hyperosmolar hyperglycemic syndrome (HHS) is a clinical condition that arises from a complication of diabetes mellitus. This problem is most commonly seen in type 2 diabetes. Won Frerichs and Dreschfeld first described the disorder around 1880. They described patients with diabetes mellitus with profound hyperglycemia and glycosuria without the classic Kussmaul breathing or acetone in the urine seen in diabetic ketoacidosis. This clinical condition was formerly called non-ketotic hyperglycemic coma; hyperosmolar hyperglycemic non-ketotic syndrome, and hyperosmolar non-ketotic coma (HONK).[1]
What is the clinical presentation of HHS?
The typical clinical presentation of patients with HHS is increased urination (polyuria) and increase water intake (polydipsia). This is a result of the stimulation of the thirst center in the brain from severe dehydration and increased serum osmolarity. Weakness, malaise, and lethargy can also be part of the complaints.
Is HHS a serious complication?
HHS is a serious and potentially fatal complication of type 2 diabetes.
What is the term for a person who has high blood sugar?
Hyperosmolar hyperglycemic syndrome ( HHS) is a serious complication of diabetes mellitus. HHS occurs when a person’s blood glucose (sugar) levels are too high for a long period, leading to severe dehydration (extreme thirst) and confusion.
What is the name of the condition where blood sugar levels are high for a long period of time?
Hyperosmolar Hyperglycemic Syndrome. A serious complication of diabetes mellitus, hyperosmolar hyperglycemic syndrome (HHS) happens when blood sugar levels are very high for a long period of time. Symptoms of HHS can include extreme thirst, frequent urination, changes in your vision and confusion.
What happens when blood sugar is too high?
HHS occurs when the blood sugar of a person with diabetes becomes too high (hyperglycemia) for a long time. The extra sugar is passed into the urine, which causes the person to urinate frequently. As a result, he or she loses a lot of fluid, which can lead to severe dehydration (extreme thirst).
How to prevent HHS?
The best way to prevent HHS is by following a healthy lifestyle and managing your diabetes. You should:
Is HHS a serious condition?
HHS is a very serious medical condition. If it is not treated, it can lead to:
What does it mean when your blood is hyperosmolar?
In simple terms, hyperosmolarity occurs when a loss of fluid (water) causes blood to be more concentrated than normal. Because you are dehydrated, your blood has high concentrations of salt, glucose and other substances.
What is Hyperosmolarity?
The Merriam-Webster dictionary defines hyperosmolarity as a condition, particularly of a bodily fluid, having abnormally high osmolarity. That definition is not very helpful to people who are not doctors or scientists though.
How long does it take for hyperosmolarity to show?
The symptoms of hyperosmolarity usually build slowly over days or weeks, so if you are monitoring your blood sugar according to your diabetes management plan, you can identify the warning signs early and take care of the problem.
What happens when blood sugar is too high?
Hyperosmolarity happens when blood sugar becomes too high for a long period of time. Normally, when someone living with diabetes has high blood sugar, the kidneys try to eliminate the excess sugar through urine. Understandably, this can make you dehydrated if you urinate a lot and don’t replenish the water in your system. The problem is made worse if you drink fluids that contain sugar and continue to eat foods with carbohydrates, because this keeps your blood sugar high and your kidneys working hard to eliminate the extra sugar. Eventually, your kidneys can’t keep up and your blood sugar rises even higher, sometimes more than 10 times the normal amount. In a nutshell, hyperosmolarity is caused by extremely high blood sugar combined with extreme dehydration.
How much blood sugar is considered hyperosmolarity?
There are some clear symptoms of hyperosmolarity, the most obvious being extremely elevated blood sugar defined as 600 milligrams per deciliter (mg/dL), with 400 mg/dL as the threshold for seeking emergency care.
Why does hyperosmolarity occur?
In simple terms, hyperosmolarity occurs when a loss of fluid (water) causes blood to be more concentrated than normal. Because you are dehydrated, your blood has high concentrations of salt, glucose and other substances. The condition draws water out of your body’s other organs, including your brain, to try to rehydrate your blood.
What is the condition that causes a person to be confused?
Confusion, or hallucinations. An altered state of consciousness from unmanaged diabetes is almost always the result of hyperosmolarity.
What Are the Warning Signs?
If you have diabetes and you’ve had a heavy thirst and gone to the bathroom more often than usual for a few weeks, check with your doctor -- especially if your blood sugar isn’t well-controlled. As your body loses more and more water, you may notice:
How Is It Treated?
Once your doctor spots the early signs, they may send you to the hospital. You’ll get an IV to replace lost fluids and electrolytes such as potassium. And you’ll get insulin or other medication to control your blood sugar. The coma can lead to death if left untreated.
Protecting Yourself From the Dangers of a Diabetic Coma
Gary Gilles is a licensed clinical professional counselor (LCPC) who has written about type 1 diabetes and served as a diabetes counselor. He began writing about diabetes after his son's diagnosis as an infant.
Symptoms
The symptoms of HHNS may appear slowly, taking days or even weeks to fully develop. Common symptoms include: 2
Causes
HHNS develops when glucose levels surge (typically above 600 mg/dl), leading to severe dehydration. This dehydration occurs because elevated levels of glucose cause blood to become thicker and result in the body needing to produce more urine in order to lower them. 3
Diagnosis
HHNS is diagnosed based on symptoms and by measuring blood glucose levels, which can be performed with a finger stick.
Treatment
Treatment typically involves starting intravenous (IV) fluids (saline solution delivered through a needle into a vein) to rehydrate the body quickly. It also may require IV insulin to bring down blood sugar levels.