
There are limitations to FAST assessments, including limitations in their ability to detect freefluid in some injured children, patients with mesenteric, diaphragmatic, or hollow viscousinjury, and patients with isolated penetrating injury to the peritoneum. The FAST examinationis also limited in identifying retroperitoneal hemorrhage, although injuries can at times be seen.The potential false-positive diagnosis of free traumatic fluid in the peritoneum may be due tofluid present in patients for physiologic reasons, including ovarian cyst rupture, as well aspathologic reasons, such as patients with ascites or inflammatory processes in the abdomen orpelvis. One must be wary of free fluid typically found intraperitoneally in patients with ven-triculoperitoneal shunts, in those who undergo peritoneal dialysis, and in those after recentperitoneal lavage. It can be difficult to identify free fluid in patients with severe polycystic dis-ease. Ultrasound may also be technically limited in the traumatized patient due to bowel gas,obesity, subcutaneous emphysema, patient positioning, the degree of injury and rate of bleed-ing, adhesions from prior surgery, and often in patients who are either in pain or combative sec-ondary to traumatic injury. The main limitation of the FAST examination is that the operatormust be knowledgeable in its clinical use and be aware that it does not exclude all injuries.
How accurate is the Fast exam?
What is the purpose of a fast exam?
Is the Fast exam good for pediatrics?
Does the Fast exam improve clinical outcomes?
Who is the author of the Fast exam?
Is a fast exam necessary for hemodynamically unstable patients?
See 1 more

What is a major benefit of FAST or eFAST?
eFAST allows for a chest examination of patients with haemodynamic instability, aiding in the identification of the location of bleeding to plan the correct surgical approach and rule out the presence of pneumothorax.
How accurate is a FAST exam?
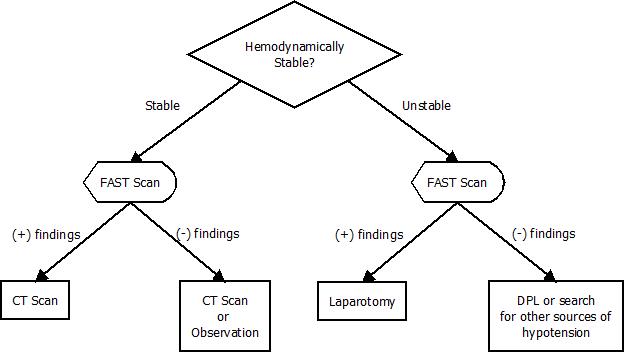
For the hemodynamically unstable patient, a positive FAST is an indication of internal hemorrhage and demands imminent intervention in the operating room. Per ACS TQIP, FAST exam has an acceptable sensitivity of 69–98% for detection of free fluid and 63% for detection of solid organ injury in adults.
Is FAST exam specific or sensitive?
Furthermore, although the FAST exam is very specific, in hemodynamically stable patients, most trauma experts suggest performing a CT after a positive FAST scan to confirm and further delineate injuries.
What is the purpose of a FAST exam?
The purpose of the FAST exam is to: Find free fluid (usually blood) in the pericardial, pleural, or intraperitoneal spaces. Detect a pneumothorax by lack of lung sliding signs.
Are FAST exams reliable in severely injured patients?
Introduction: Highly sensitive and accurate for the detection of injuries requiring intervention in haemodynamically unstable patients, FAST may underestimate intra-abdominal injuries in stable patients with blunt abdominal trauma.
What is a normal FAST exam?
The FAST (Focused Assessment with Sonography in Trauma) examination looks for the presence of fluid—presumed to be blood in the appropriate clinical setting—visualizing 10 structures or spaces in four areas: Pericardial. Perihepatic. Perisplenic. Pelvic.
What is looked at in a FAST exam?
The FAST exam evaluates the pericardium and three potential spaces within the peritoneal cavity for pathologic fluid. The right upper quadrant (RUQ) visualizes the hepatorenal recess, also known as Morrison's pouch, the right paracolic gutter, the hepato-diaphragmatic area, and the caudal edge of the left liver lobe.
Can a test be 100% sensitive and specific?
Tradeoffs between sensitivity and specificity While it is possible to have a test that has both 100% sensitivity and 100% specificity, chances are that in those cases distinguishing between who has disease and who doesn't is so obvious that you didn't need the test in the first place.
Can a test be specific and sensitive?
A highly sensitive test means that there are few false negative results, and thus fewer cases of disease are missed. The specificity of a test is its ability to designate an individual who does not have a disease as negative. A highly specific test means that there are few false positive results.
When is a FAST exam positive?
Positive FAST will have one of the following: Anechoic area within the pericardial space. Anechoic areas between the liver and kidney. Anechoic areas between the diaphragm and spleen.
When was the FAST exam invented?
The term "Focused Abdominal Sonography for Trauma" was coined in 1996 to describe a standard set of ultrasound examinations for the evaluation of injured patients. The meaning of the acronym was changed to Focused Assessment with Sonography for Trauma (FAST) a year later to reflect applications outside the abdomen.
How do you conduct a FAST exam?
0:393:21Place the probe right on the sternum. And then slide off until you see the long axis.MorePlace the probe right on the sternum. And then slide off until you see the long axis.
When is a FAST exam positive?
Positive FAST will have one of the following: Anechoic area within the pericardial space. Anechoic areas between the liver and kidney. Anechoic areas between the diaphragm and spleen.
How much fluid can a FAST scan detect?
In the detection of pleural effusion or hematothorax ultrasound can detect even the smallest amounts of fluid (20 ml) whereas you need 200ml to detect those pathologies with a chest X-Ray. The eFAST exam has largely replaced the peritoneal lavage as the primary method to detect free intraperitoneal fluid.
How do you conduct a FAST exam?
0:393:21Place the probe right on the sternum. And then slide off until you see the long axis.MorePlace the probe right on the sternum. And then slide off until you see the long axis.
What is a positive lavage?
The lavage is positive if there are > 100,000 red blood cells/mL, > 500 white blood cells/mL, or a positive Gram stain test. A negative test does not exclude other solid organ injury, viscus perforation, diaphragmatic tears, or retroperitoneal injury.
What is the pericardial space of a positive fast?
Positive FAST will have one of the following: Anechoic area within the pericardial space. Anechoic areas between the liver and kidney. Anechoic areas between the diaphragm and spleen. Anechoic areas between the spleen and kidney. Anechoic areas between superior and posterior to the posterior wall of the bladder.
What is a bedside fast ultrasound?
A bedside FAST ultrasound was conducted to assess for free fluid with clinical indication of trauma. Cardiac, RUQ, pelvic, and LUQ views were adequately obtained. There was no free fluid identified.
What is the FAST exam?
We know this ultrasound study well. The FAST exam, or Focused Assessment with Sonography in Trauma, is one of the most common applications of point of care ultrasound in the Emergency Department. The goal of the FAST exam is to detect free fluid in the abdomen, typically hemoperitoneum in the unstable trauma patient. The “extended” (E)-FAST exam also looks for pneumothorax, pleural effusion and pericardial fluid. The EFAST exam can quickly evaluate the unstable trauma patient and direct emergent management of hemoperitoneum, hemopericardium, hemothorax, and pneumothorax. [1]
Does a secondary survey show a fractured right forearm?
The secondary survey doesn’t give you any big surprises. You, of course, note the open right distal forearm fracture. The patient has a very minimal amount of diffuse abdominal tenderness with no external evidence of injury. The secondary survey is otherwise unremarkable. Concerned about the patient’s diffuse abdominal tenderness and tachycardia, you decide to do a FAST exam …
Can you perform an EFAST on a patient?
You quickly perform an EFAST on your patient, with the following images obtained below.
Does free intraperitoneal fluid highlight fascial planes?
In contrast, when free intraperitoneal fluid is present, only one echogenic line will be visible bounding the fluid. Pathologic free fluid does not highlight fascial planes, unlike perinephric fat. Compare the two clips below:
How to read a fast exam?
The FAST exam most commonly uses the subxiphoid (AKA subcostal) view to assess the pericardial space. To obtain this view, place the transducer just inferior and to the patient’s right of the xiphoid process. Yes, you read that correctly – to the right of the xiphoid process. While it sounds counterintuitive, this placement uses the liver as an acoustic window allowing better visualization of the heart. The indicator marker on the probe should point towards the patient’s right. Aim the beam toward the patient’s left shoulder. Your scanning plane should be closer to a coronal plane than a transverse plane (i.e. point the probe more towards the patient’s head than their spine). Your depth will need to be set deeper than for abdominal windows, often 20-25cm depending on the size of your patient. If you’re having trouble, set the depth very deep and (usually) the motion of the heart will be easy to see. You can then adjust the depth as needed once you find the heart. Having the patient take and hold a deep breath may also help with visualization.
How many windows are typically imaged in a fast examination?
10 structures or spaces are typically imaged via 4 windows in a FAST examination; other views may be included and other structures evaluated. The windows and what is evaluated include
What is a fast exam?
The FAST exam evaluates the pericardium and three potential spaces within the peritoneal cavity for pathologic fluid. The right upper quadrant (RUQ) visualizes the hepatorenal recess, also known as Morrison’s pouch, the right paracolic gutter, the hepato-diaphragmatic area, and the caudal edge of the left liver lobe. Position the probe in the sagittal orientation along the patient’s flank at the level of the 8 to 11 rib spaces. Start with your hand against the bed to ensure visualization of the retroperitoneal kidney. The RUQ view is the most likely to detect free fluid with an overall sensitivity of 66% [11] [12]. Recent retrospective evidence suggests the area along the caudal edge of the left lobe of the liver has the highest sensitivity, exceeding 93% [11]. Most importantly, remember to assess each of these areas while scanning the RUQ.
What is efast protocol?
Recently, many institutions have introduced the Extended FAST (eFAST) protocol into their trauma algorithms. The eFAST examines each hemithorax for the presence of hemothoraces and pneumothoraces.
Is eFAST contraindicated?
There are no absolute contraindications to the eFAST. However, eFAST should not delay resuscitative efforts for patients in extremis.
Is efast ultrasound sensitive?
There are no known complications from the eFAST exam. However, ultrasound has several limitations. It is only 85% sensitive requiri ng the presence of more than 150 cc to 200 cc of intra-peritoneal fluid to detect [19]. Serial FAST exams can help prevent false-negative studies [7]. Other false negatives include patients with delayed presentations whose hemorrhage has clotted causing a mixed echogenicity rather than the anechoic or black appearance of fresh blood or fluid. False positives include ascites, peritoneal dialysate, ruptured ovarian cysts, and ruptured ectopic pregnancies. Additionally, ultrasound cannot distinguish between blood and urine in severe pelvic trauma and cannot evaluate retroperitoneal hemorrhages.
Is Fast ultrasound good for trauma patients?
While FAST is useful in trauma patients, it has limitations. Clinicians should be aware that the point of care ultrasound image acquisition and interpretation is limited by the provider’s experience; the patient’s body habitus; and the presence of bowel gas, pneumoperitoneum, or pneumomediastinum.
Is efast a standard of care?
The EAST (Eastern Association for the Surgery of Trauma) guidelines, Western Trauma Association, and ATLS recommend the eFAST as the standard of care in trauma resuscitation protocols. The eFAST has been shown to decrease time to operative intervention; patient length of stay; cost; and the rates of complications, CTs, and DPLs performed [1]. As with any imaging modality though, recognize and understand its limitations.
What is fast examination?
The FAST examination was originally intended to detect intraperitoneal free fluid. However, US is well suited to depict abnormalities of solid organ parenchyma indicative of injury, especially during serial studies. In 1983, vanSonnenberg and colleagues first reported the US appearance of blood as linear echogenic foci in solid organs after fine-needle aspiration biopsy ( 73 ). Since then, studies specific for blunt abdominal trauma have been published. The sensitivity for detection of solid organ injury with US has been shown to be limited, with two studies reporting sensitivities of 41% (24 of 58) and 44% (11 of 25) ( 74, 75 ). During the first few hours after injury, fresh blood clots in the injured organ may have echogenicity similar to that of the parenchyma organs ( 76 ). Richards and McGahan and colleagues reported US findings of the parenchyma in solid organ injuries. A diffuse heterogeneous pattern is most commonly detected in splenic lacerations ( Movie 4 [online]), whereas a discrete hyperechoic pattern ( Movie 2 [online]) is seen most often in hepatic lacerations ( 77, 78 ). Subcapsular splenic hematomas are detected as either hyperechoic or hypoechoic rims surrounding the parenchyma ( Figs 14, 15; Movie 4 [online]), and splenic lacerations tend to become hypoechoic over a few days. For urological trauma, high-grade renal injuries have mixed echogenicity with a disorganized pattern, and bladder hematomas frequently appear echogenic ( 79 ).
What does "fast" mean in medical terms?
It was not widely adopted in North America until the 1990s, during which time the FAST acronym was defined as “focused abdominal sonography for trauma” ( 4 – 6 ). As FAST evolved into a more comprehensive examination, the acronym was changed to “focused assessment with sonography for trauma” ( 7 ).
What is a fast ultrasound?
Focused assessment with sonography in trauma (FAST) has been extensively utilized and studied in blunt and penetrating trauma for the past 3 decades. Prior to FAST, invasive procedures such as diagnostic peritoneal lavage and exploratory laparotomy were commonly utilized to diagnose intraabdominal injury. Today the FAST examination has evolved into a more comprehensive study of the abdomen, heart, chest, and inferior vena cava, and many variations in technique, protocols, and interpretation exist. Trauma management strategies such as laparotomy, laparoscopy, endoscopy, computed tomographic angiography, angiographic intervention, serial imaging, and clinical observation have also changed over the years. This state of the art review will discuss the evolution of the FAST examination to its current state in 2017 and evaluate its evolving role in the acute management of the trauma patient. The authors also report on the utility of FAST in special patient populations, such as pediatric and pregnant trauma patients, and the potential for future research, applications, and portions of this examination that may be applicable to radiology-based practice.
Is fast used in trauma?
There have been several studies of FAST utilization in pediatric trauma patients. Several studies have shown sensitivities, specificities, and accuracies similar to those in adults ( 93 – 96 ). However, a similar number have shown lower sensitivity. Fox et al studied FAST in 357 children with blunt abdominal trauma ( 97 ). Sensitivity for hemoperitoneum was 52% and specificity was 96%. The authors concluded a positive FAST examination suggests hemoperitoneum, but a negative FAST examination does not help in clinical decision making. A meta-analysis of the question determined pediatric FAST had an overall sensitivity of 66% and specificity of 95% for detection of hemoperitoneum ( 98 ). A survey of level 1 trauma centers and dedicated children’s hospitals showed that FAST was used in 96% adult-only, 85% combined adult and pediatric, and 15% children’s hospitals ( 99 ). The authors concluded the greatest impediment to the use of FAST in children’s hospitals was the perception of its limited sensitivity and higher proportion of IAI without accompanying free fluid in injured children. The use of FAST in pediatric trauma patients has been used to decrease radiation exposure from CT. In one pediatric trauma study, the need for CT was determined by surgeons trained in FAST ( 100 ). In 48% (42 of 88) of patients, the surgeon did not order CT based on the FAST and physical examination. Menaker et al studied 887 hemodynamically stable children with blunt torso trauma and queried their treating clinicians regarding suspicion of injury ( 101 ). They determined use of FAST increased as suspicion for IAI increased. Children with low or moderate suspicion of IAI were less likely to undergo CT if they had a negative FAST examination. Figure 17 demonstrates FAST of an infant.
Is a serial fast sonogram good for blunt trauma?
As the initial FAST sonogram represents a snapshot in time, serial examinations performed in stable blunt trauma patients may be useful. Examination after stabilization gives the sonographer more time for a comprehensive scan. With active intraperitoneal hemorrhage, the amount of free fluid should theoretically increase with time. The value of serial US has not been fully investigated. Nunes et al reported that serial FAST examinations decreased the false-negative rate by 50% and increased sensitivity for free fluid detection from 69% (nine of 13) to 85% (11 of 13) ( 70 ). Other studies have confirmed this trend ( 71, 72 ). One study group included an additional view of the “interloop” space, a triangular hypoechoic area between bowel, which improved the sensitivity of FAST in both primary and secondary examinations ( 72 ). We believe a baseline CT, with high sensitivity in the detection of IAI, could be augmented by FAST performed at the bedside if a patient becomes unstable ( Fig 14 ). Serial FAST examinations may be a logical alternative for stable trauma patients, patients with sudden change in hemodynamic status or physical examination, and pregnant patients to mitigate radiation exposure.
Is Efast a good protocol?
As eFAST is a relatively new protocol, there are fewer studies evaluating its accuracy in detecting pneumothorax. The diagnosis of small-to-moderate size pneumothoraces with physical examination and supine chest radiography is challenging, and these occult injuries may be missed in up to 76% (81 of 107) of blunt trauma patients ( 54 ). In studies using CT as the reference standard, the sensitivity of eFAST is better than that of supine chest radiography. Kirkpatrick and colleagues performed a prospective blinded study of 225 trauma patients with eFAST and reported a sensitivity of 48.8% (21 of 43) for chest US versus 20.9% (nine of 43) for chest radiography ( 31 ). Ianniello and co-workers investigated 368 unstable trauma patients with eFAST and reported a sensitivity of 77% (67 of 87) for detection of pneumothorax ( 55 ). Another study of 305 trauma patients concluded eFAST had a sensitivity of 43% (32 of 75) compared with chest radiography (11%, eight of 75) ( 56 ).
What is a fast exam?
With respect to trauma resuscitation, FAST exam offers the opportunity for quick, serial exams to identify potentially fatal conditions, including peritoneal free fluid and pericardial tamponade (1). It is indicated for the triage of blunt trauma patients (7) to direct decision making (1). In penetrating abdominal trauma FAST selects for patients requiring emergent exploratory laparotomy (5).
What is a fast ultrasound?
Focused Assessment with Sonography for Trauma (FAST) is an integral adjunct to primary survey in trauma patients (1-4) and is incorporated into Advanced Trauma Life Support (ATLS) algorithms (4). A collection of four discrete ultrasound probe examinations (pericardial sac, hepatorenal fossa (Morison’s pouch), splenorenal fossa, and pelvis/pouch of Douglas), it has been shown to be highly sensitive for detection of as little as 100cm3 of intraabdominal fluid (4,5), with a sensitivity quoted between 60-98%, specificity of 84-98%, and negative predictive value of 97-99% (3). Further increasing sensitivity, ATLS recommends a repeat FAST exam in 30 minutes to increase sensitivity in slow bleeds, or early post-trauma presentations in the case that the first exam was negative (4). Recently, the Extended FAST (E-FAST) exam has become standard and includes assessment for post-traumatic pneumothoraces (6).
Is E-fast fluid a blood?
As portrayed in this case report, E-FAST offers little ability to discern the specific fluid identified (8). Free fluid on E-FAST could be blood, but could also be urine, ascites, bile, pus, peritoneal dialysate fluid, or bowel contents . In the setting of trauma, peritoneal free fluid must be considered blood, and the trauma patient resuscitated appropriately, with CT imaging as tolerated versus emergent exploratory laparotomy. This case illustrates an interesting example of a trauma patient’s E-FAST exam that was falsely positive for blood in the peritoneum.
Is E-fast a good tool for trauma resuscitation?
E-FAST exam has become an integral adjunct to trauma resuscitation. In skilled hands it is a powerful tool with ability to drastically improve patient outcomes. Although fast, non-invasive, and sensitive, E-FAST examination should be interpreted skilfully. An appreciation for E-FAST limitations and sensitivity is required for successful trauma resuscitation.#N#Of note, decreased sensitivity for intra-abdominal injury has been linked to specific patient populations, including those with higher Injury Severity Scores (3), and hemodynamically stable patients with blunt abdominal injury (7). Negative FAST exams in these cohorts should be interpreted with caution, and consideration of further investigations or serial exams considered. Further recognized limitations include failure to identify retroperitoneal or solid organ injuries, failure to recognize clotted blood as hematoma, and difficult patient groups including those that are obese (8).
How accurate is the Fast exam?
The FAST exam has not been well validated in a pediatric population, but appears to be even less accurate than in adults. 5 A 2007 meta-analysis found that the sensitivity of ultrasound for intra-peritoneal fluid in children was only 66%. 6 Almost all of the included studies involved formal ultrasounds read by radiologists, so the sensitivity is likely to be much worse in the hands of a community emergency physician. Studies of the FAST exam performed by emergency physicians in a pediatric population reveal a sensitivity between 28% and 52%. 7–9 Furthermore, it is not clear that identifying free fluid is helpful in the pediatric population, as children can have free fluid without any injury, and also frequently present with injury in the absence of free fluid. 10
What is the purpose of a fast exam?
The official role of the FAST exam in trauma is to identify patients with hemorrhagic shock who require immediate transfer to the operating room. 1,2 “The aim is to identify life-threatening intra-abdominal bleeding or cardiac tamponade with a view to expediting definitive surgical management. It does not aim to exclude abdominal or thoracic injury.” 1
Is the Fast exam good for pediatrics?
In keeping with the poor diagnostic accuracy of the FAST exam in a pediatric population, the clinical evidence does not support a benefit. There is a randomized clinical trial looking at the use of the FAST exam in a pediatric population, and they conclude that “among hemodynamically stable children treated in an ED following blunt torso trauma, the use of FAST compared with standard care only did not improve clinical care, including use of resources; ED length of stay; missed intra-abdominal injuries; or hospital charges. These findings do not support the routine use of FAST in this setting.” 9
Does the Fast exam improve clinical outcomes?
In keeping with its poor diagnostic characteristics, there is no evidence that the FAST exam improves clinical outcomes. A Cochranre review identified 4 studies, and the FAST exam was not associated with any improvement in mortality (RR 1.00; 95% confidence interval 0.5 to 2.0). They conclude that “the experimental evidence justifying FAST‐based clinical pathways in diagnosing patients with suspected abdominal or multiple blunt trauma remains poor.” 4
Who is the author of the Fast exam?
Justin Morgenstern. The FAST exam: overused and overrated?, First10EM, 2021. Available at:
Is a fast exam necessary for hemodynamically unstable patients?
The evidence of benefit is non-existent, but I think there is clearly a role for the FAST exam in hemodynamically unstable patients. However, even among the hemodynamically unstable, the role may be more limited than you think. It is essential to consider your resources, and how the test will change your management. In a trauma center, when you are deciding between the operating room and interventional radiology, the FAST exam may provide invaluable information. In the community, where most of us work, such treatment options don’t exist, and the FAST exam may just be delaying the transfer the patient needs.
Background
Indications
Technique
Images
- Normal
1. Normal subxiphoid view 2. RUQ with no free fluid 3. Normal saggital bladder - Abnormal
1. Pericardial effusion 2. Positive FAST (RUQ) 3. Positive FAST (RUQ) 4. Free fluid superior to the bladder 5. Positive FAST (LUQ)
Pearls and Pitfalls
- The area between the liver and kidney in the RUQ view is called Morison’s pouch
- In the LUQ view, fluid is most likely to accumulate between the diaphragm and spleen, not between the spleen and kidney
- Scans must scan through the inferior poles of the kidneys as this can contain small quantities of fluid
- The area between the liver and kidney in the RUQ view is called Morison’s pouch
- In the LUQ view, fluid is most likely to accumulate between the diaphragm and spleen, not between the spleen and kidney
- Scans must scan through the inferior poles of the kidneys as this can contain small quantities of fluid
- Serial exam may be needed
Documentation
- Normal Exam
A bedside FAST ultrasound was conducted to assess for free fluid with clinical indication of trauma. Cardiac, RUQ, pelvic, and LUQ views were adequately obtained. There was no free fluid identified. - Abnormal Exam
A bedside FAST ultrasound was conducted to assess for free fluid with clinical indication of trauma. Cardiac, RUQ, pelvic, and LUQ views were adequately obtained. There was free fluid identified in the RUQ suggesting intraabdominal hemorrhage.
Clips
- Normal
1. Normal subxiphoid view 2. Normal pelvic view - Abnormal
1. Free fluid located at the liver tip
External Links
See Also