What is a pedicle Flapa?
pedicle flapa flap consisting of the full thickness of the skin and the subcutaneous tissue, attached by tissue through which it receives its blood supply. Called also pedicle graft. random pattern flapa myocutaneous flap with a random pattern of arteries, as opposed to an axial pattern flap.
What is the difference between a free flap and pedicled flap?
A free flap requires the transfer of tissue from one body site to another, with anastomosis of arterial and venous systems to the recipient site using microsurgical techniques. A pedicled flap transposes tissue from a donor site to a recipient site while keeping the tissue partially attached to the donor site.
What is a pedicle flap breast reconstruction?
Pedicle Flaps When surgeons began to use a woman’s own tissue in breast reconstruction, they would move the living tissue from a nearby location, often from the abdomen or back, without detaching it from the body. These flaps are still used today and are collectively called pedicle flaps, which mean they remain connected to the blood supply.
How wide should a pedicle be for a flap?
The narrowest safe pedicle width should be chosen. A 7 to 8 mm margin on either side of the glabellar crease will reliably produce a flap with abundant vascular supply and drainage, and in most cases an overall pedicle width of 1.5 cm is a safe plan.

What is the difference between free flap and pedicle flap?
When the TRAM flap is a pedicle flap, it remains attached to its blood supply, with the tissue surgically tunneled underneath the skin to the breast region. When the TRAM flap is a free flap, the tissue is detached and cut away from its blood supply before being transferred.
How is pedicle flap done?
In a pedicle TRAM flap procedure, the surgeon cuts a section of skin, muscle, fat and blood vessels from your abdomen, tunnels the tissue underneath your skin to its new location, and uses it to form a new breast mound.
What does pedicle mean in surgery?
Spine Anatomy Overview Video. The pedicle is a stub of bone that connects the lamina to the vertebral body to form the vertebral arch. Two short, stout processes extend from the sides of the vertebral body and joins with broad flat plates of bone (laminae) to form a hollow archway that protects the spinal cord.
What is a pedicle skin graft?
Skin graft, pedicle: A graft technique in which a piece of skin from a nearby area remains attached at one of its corners, while the main part of the piece is reattached over the area that needs to be covered.
What is the most common pedicle based flap used for breast reconstruction?
The most common pedicle flap used for breast reconstruction is the latissimus dorsi (LD) flap, where tissue from the back (skin, fat, and muscle) is used to make a new breast. Tissue from the abdominal wall (tummy) can also be used as a pedicle flap (transverse rectus abdominis muscle or TRAM flap).
Which kind of surgery is also known as flap surgery?
Flap surgery is a technique in plastic and reconstructive surgery where any type of tissue is lifted from a donor site and moved to a recipient site with an intact blood supply. This is distinct from a graft, which does not have an intact blood supply and therefore relies on growth of new blood vessels.
Where is the pedicle located?
Pedicle. The pedicle is a short projection of bone that comes directly off the back of the vertebral body. The pedicle lies between the back of the vertebral body and the transverse process. There are two pedicles per vertebra, one on each side.
What is the function of the pedicle?
Pedicles. Each vertebra has two cylinder-shaped projections (pedicles) of hard bone that stick out from the back part of the vertebral body, providing side protection for the spinal cord and nerves. The pedicles also serve as a bridge, joining the front and back parts of the vertebra.
What is the difference between flap and graft?
How does a flap differ from a graft? A flap is transferred with its blood supply intact, and a graft is a transfer of tissue without its own blood supply. Therefore, survival of the graft depends entirely on the blood supply from the recipient site. Flap surgery is a subspecialty of plastic and reconstructive surgery.
Which is better skin graft or skin flap?
Flaps usually heal faster than grafts. A graft is a piece of healthy skin that is removed from one part of the body and used to cover a wound elsewhere. Unlike a skin flap, a graft does not have its own blood supply. At first, the graft survives because nutrients pass (diffuse) from the wound site into the graft.
What are the 4 types of skin grafts?
Autograft or autologous graft: skin obtained from the patient's own donor site. Allograft or heterologous graft: skin obtained from another person. Xenograft or heterograft: skin from other species, such as pigs. Synthetic skin substitutes: manufactured products that work as skin equivalents.
What are the 4 types of grafts?
There are four classifications of grafts: (1) autograft (tissue removed from one site and surgically implanted into another on the same individual); (2) isograft (tissue removed from an individual and surgically grafted onto a genetically identical individual, such as an identical twin or another member of the same ...
What is the difference between flap and graft?
How does a flap differ from a graft? A flap is transferred with its blood supply intact, and a graft is a transfer of tissue without its own blood supply. Therefore, survival of the graft depends entirely on the blood supply from the recipient site. Flap surgery is a subspecialty of plastic and reconstructive surgery.
What are flaps in plastic surgery?
The use of skin grafts for reconstruction is reviewed separately. (See "Skin autografting".) A flap is a transfer of tissue with its intrinsic blood supply from one part of the body to another. The blood supply to a flap is persistent and does not depend on the recipient bed.
What is DIEP flap reconstruction surgery?
During a DIEP flap reconstruction, tissue from a woman's lower belly is surgically removed, shaped and attached to the chest to form a new breast. The surgeon takes skin, fat, and blood vessels, but leaves the underlying abdominal muscle (rectus abdominus) intact.
What type of flap is lifted and sutured to another location?
A transposition skin flap is a segment of skin and subcutaneous tissue or panniculus muscle (e.g. cutaneous trunci) that is lifted and has its orientation shifted as it is placed onto a wound. Thus, the flap is transposed to close the wound.
What is a pedicle flap?
in periodontal surgery, a flap used to increase the width of attached gingiva, or to cover a root surface, by moving the attached gingiva, which remains joined at one side, to an adjacent position and suturing the free end. Term is considered obsolete in some disciplines (for example, plastic surgery).
What is attached flap?
Also called an attached flap. A section of tissue, with its blood supply intact, which is maneuvered to another part of the body.
What is a flap in surgery?
periodontal surgery A flap used to increase the width of attached gingiva, or to cover a root surface, by moving the attached gingiva, which remains joined at one side, to an adjacent position and suturing the free end.
What is a random pattern flap?
random pattern flap a myocutaneous flap with a random pattern of arteries, as opposed to an axial pattern flap.
What is a flap in medical terms?
flap. [ flap] 1. a mass of tissue for grafting, usually including skin, only partially removed from one part of the body so that it retains its own blood supply during transfer to another site. 2. an uncontrolled movement. advancement flap sliding flap.
What is a free flap?
free flap an island flap detached from the body and reattached at the distant recipient site by microvascular anastomosis.
What is a sliding flap?
sliding flap a flap carried to its new position by a sliding technique; called also advancement flap.
What is a pedicled flap?
Traditional pedicled flaps are the workhorse reconstruction options when a portion or all of a degloving injury is irretrievable. These are many in number, from local flaps such as cross-finger flaps to contralateral upper arm, inframammary, and groin flaps, among others. These serve the purpose of supplying coverage over wounds of any depth and complexity, unlike split-thickness skin grafts. In addition, they can be used to reconstruct damaged veins as a vascularized vein graft carrier. 26 These flaps, in addition, allow subsequent surgery to be performed beneath them, either by raising them from the side or by operating directly through them.
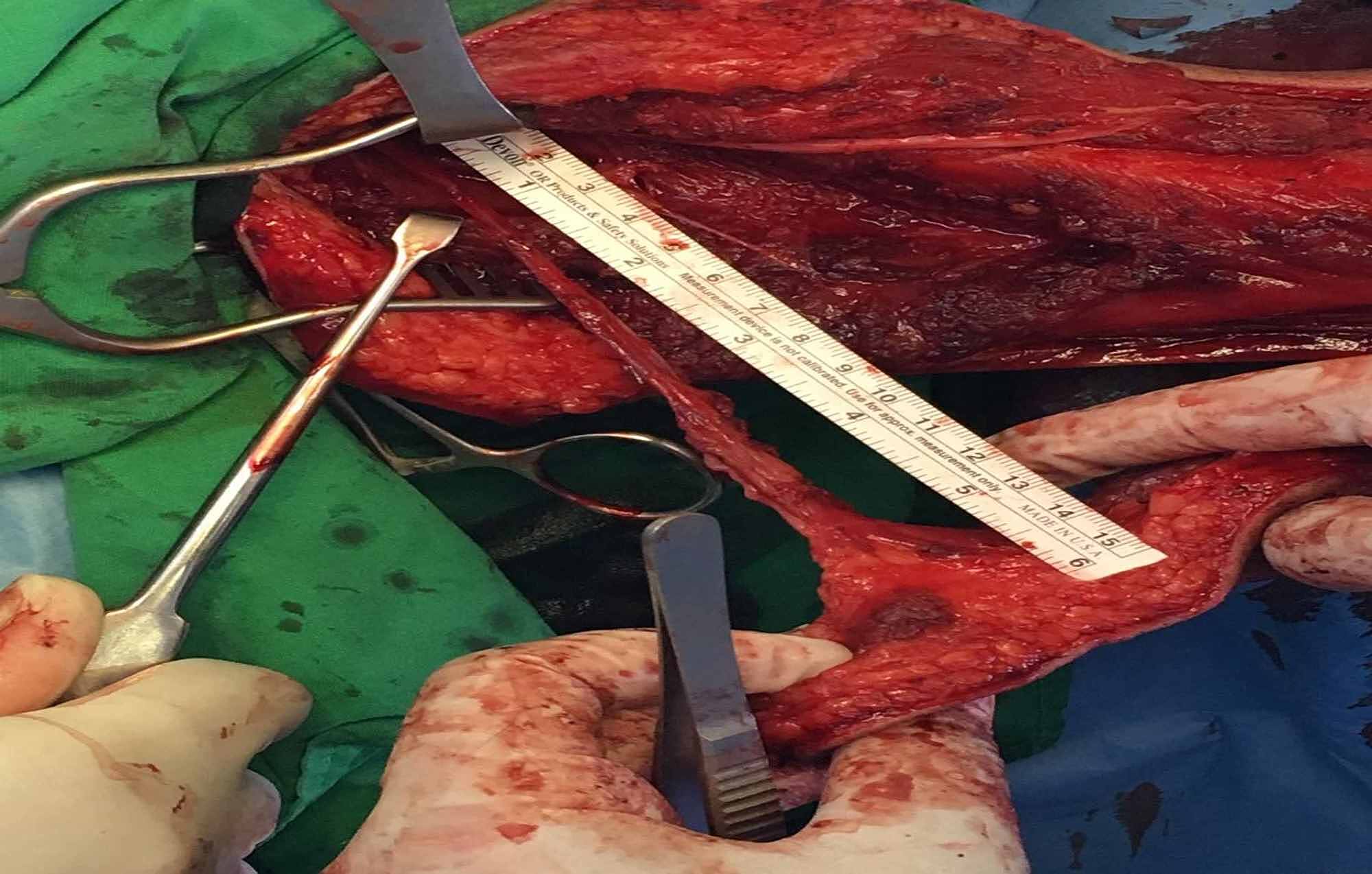
Which flaps are used in the pedicled flap?
Pedicled flaps utilizing the soleus, pero neus brevis, extensor digitorum longus (EDL), and peroneus tertius were elegantly described by Hughes and Mahoney, but there are several caveats one should consider before using them ( Fig. 23.2 ). 23
How long does it take for a pedicle flap to be attached?
Use of such flaps necessitates a delay period (usually 2 to 3 weeks) during which the pedicle flap remains attached to both the recipient and donor sites.
Why is the island pedicle flap so important?
The island pedicle flap is remarkable because the flap can be advanced as far as the motion of the deep pedicle allows . This mobility is frequently much greater than a similarly designed flap would advance if dermal margins that restrain flap motion were retained at the peripheral margins of the flap ( Fig. 21.8 ). In addition, the island pedicle has a rich blood supply from underlying vessels and musculature and is not forced to rely solely upon the anastomotic vascular network of the dermis for perfusion. As such, the island pedicle flap is remarkably impervious to ischemia, even when the flap is inserted under considerable wound closure tensions.
What is the Latissimus Dorsi flap?
43. Latissimus dorsi flaps use the latissimus muscle and overlying tissue supplied by the thoracodorsal artery and vein. This option can also be used for immediate or delayed reconstruction.
How to overcome resistance to flap movement?
Resistance to flap movement may be alleviated by these maneuvers: (1) scoring incision (to dermis) at the proximal triangle (if a myocutaneous design was chosen), which frees proximal skin attachments tethering the flap, (2) closing the donor cheek in a superior oblique vector (northeast for the right cheek and northwest for the left), which progressively brings the flap medially and superiorly ( Figure 8.18 ), and (3) temporary suspension suture lifting the flap to the upper cutaneous lip, which is removed in 1 week.
What muscle is used in a tram flap?
The TRAM flap uses the abdominal skin, fat, and rectus muscle to give a reconstructed breast with excellent shape, ptosis, and contour. It offers a more natural look and feel than implant reconstruction ( Fig. 13-6 ).
What are the most common pedicle flaps?
In breast reconstruction, the most common pedicle flaps are TRAM and LD flaps .
What is LD flap?
The LD flap incorporates the latissimus dorsi, the broadest muscle of the back, and is one of the oldest options available for breast reconstruction. The flap’s risk of failure is minimal because of its reliable blood supply, and it may be particularly suited to patients who have undergone past radiation treatments.
What is the flap that attaches to the mastectomy site called?
These flaps usually include a perforating blood vessel and are called perforator flaps.
What are the flaps on the breast called?
Pedicle Flaps. When surgeons began to use a woman’s own tissue in breast reconstruction, they would move the living tissue from a nearby location, often from the abdomen or back, without detaching it from the body. These flaps are still used today and are collectively called pedicle flaps, which mean they remain connected to the blood supply.
How long does it take to get a TRAM pedicle?
The TRAM pedicle procedures take about two hours at MUSC, while the free-flap procedure takes about three hours. Both require a four-day hospital stay. Because muscle is removed from the abdomen via the TRAM flap, the affected area will be weaker than the surrounding tissues.
Where do breast reconstruction flaps draw blood from?
Some of the first efforts to use a woman’s natural tissue for breast reconstruction involved TRAM flaps, which draw much of their blood supply from vessels in the transverse rectus abdominis muscle.
How long does it take to recover from LD flap surgery?
When used to reconstruct one breast, the transfer of the LD flap generally takes 1½ to 2 hours and is followed by a three-day hospital stay. The procedure leaves a diagonal scar, about 10 to 15 cm long, in the middle of the woman’s back, below the shoulder blade and following the course of the ribs.
What are the two types of pedicle flaps?
Two distinct pedicle flaps for nasal reconstruction are described: the interpolated nasolabial flap and the paramedian forehead flap. The flap selection between nasolabial flap and paramedian forehead flap is dictated primarily by surgeon’s preference, but the flaps should not be considered interchangeable. Nasolabial flaps are suitable for patients with a distinct nasolabial fold and cheek redundancy and who have either ala, tip, or soft triangle defects with intact lining. Advantages of the nasolabial flap include technically simpler flap harvest, the ability to harvest under local or intravenous sedation only, and much easier postoperative wound care.
What is the flap treated with?
The flap is dressed with fibrillar collagen immediately postoperatively and the pedicle donor site deliberately packed with either fibrillar collagen or sterile cotton for hemostasis and the patient is instructed to simply shower away the dressings on the third postoperative day and then the flap is treated with just petroleum ointment until it is divided between the third and fourth weeks. 3The patient is allowed to return to full activity and as long as the pedicle is not compressed, the patient can wear a CPAP mask (▶ Fig. 8.15).
What is the flap in Fig. 8.22?
Fig. 8.22 Flap is coated in nitropaste. Following dermabrasion with Bovie scratch pad of cheek scar, it is coated in bacitracin ointment.
How much volume is the flap in Fig. 8.19?
Fig. 8.19 Flap is elevated up to 80% of its maximal volume and inset under slight tension.
Which flap is most suitable for nasal reconstruction?
Summary. Two distinct flaps, the paramidline forehead flap and the nasolabial flap, are most suitable for nasal reconstruction. Although they should not be considered interchangeable, either pedicle flap can be considered for the majority of defects without lining.
Is paramidline forehead flap reliable?
The paramidline forehead flap is exceedingly reliable and predictable and should be the first choice for nasal defects of any significance.
Why do you need a pedicle flap?
A wider or deeper pedicle may be needed in order to assure adequate venous drainage. While the portion of the flap placed in the operative wound may have very little subcutaneous tissue, the same cannot be true of the nourishing stalk or pedicle. Also, pedicle flaps are designed to be sewn into place under little to no tension. Tension and torsion of a pedicle can lead to flap failure and should be avoided.
Why are pedicle flaps left in place?
The flap is left in place for a defined period of time in order to vascularize from the recipient bed, and then the pedicle is severed. Interpolated pedicle flaps allow for the reconstruction of challenging operative wounds, in particular wounds of the nose, ear, and lip. The history of pedicle flaps dates to ancient India ...
How long do you have to live with an interpolated pedicle flap?
Because interpolated pedicle flaps require patients to live for at least several weeks with a deformed appearance, appropriate preoperative consultation is essential. All pedicle flaps require at the very least one revision (the flap takedown), and patients should be counseled that further revisions and modifications may be needed. While pedicle flaps can be accomplished in smokers, flap failure is more likely in this subgroup of patients and appropriate counseling is needed.
What is interpolation flap?
Interpolation flaps are delayed pedicle flap reconstructions in which a flap of tissue is elevated at one location and transposed over intervening skin to an operative wound. The flap is left in place for a defined period of time in order to vascularize from the recipient bed, and then the pedicle is severed. Interpolated pedicle flaps allow for the reconstruction of challenging operative wounds, in particular wounds of the nose, ear, and lip.
What is the Abbe-Estlander flap?
The Abbe-Estlander flap contains the labial artery. The inclusion of a single larger caliber vessel in such pedicles increases the blood supply to the flap by a factor of 625, and it is usual for a very long, narrow pedicle flap to have arterial bleeding from its distal tip after complete elevation.
Where is the pedicle in Figure 6.3A?
Figure 6.3A pedicle is created on the forehead based on the supratrochlear vessels and frontalis. The flap must be long enough to reach the distal nose easily
How to use a template for a contralateral pedicle?
This can be done with the sterile foil of a suture packet or with sterile gauze. For a contralateral pedicle, the template is inverted, rotated, and moved to the forehead. In obtaining a template over a convex surface, it is important to use a form that will take into account the curvature of the underlying structure. A common error is to undersize the flap by basing the template size on only the horizontal dimension of the wound. On the other hand, if a subunit repair is to be undertaken, the template should be created prior to excision of the remaining subunit in order not to overestimate the operative wound secondary to peripheral wound contraction.
What is a pedicle flap?
pedicle flapa flap consisting of the full thickness of the skin and the subcutaneous tissue, attached by tissue through which it receives its blood supply. Called also pedicle graft.
What is an island flap?
island flapa flap consisting of skin and subcutaneous tissue, with a pedicle made up of only the nutrient vessels.
What is a tube flap?
tube flap(tubed pedicle flap) a bipedicle flap made by elevating a long strip of tissue from its bed except at the two extremities, the cut edges then being sutured together to form a tube.
What is a rotation flap?
rotation flapa local pedicle flap whose width is increased by having the edge distal to the defect form a curved line; the flap is then rotated and a counterincision is made at the base of the curved line, which increases the mobility of the flap.
How wide is the flap?
The maximum width of the flap that can be primarily closed in most patients is 10 cm.
What is a free flap?
A free flap requires the transfer of tissue from one body site to another, with anastomosis of arterial and venous systems to the recipient site using microsurgical techniques.
How big is a SCIA flap?
Flap size is limited to about 13 × 10 cm ( FIG 2 ). The axis of the SCIA is marked by palpating the femoral pulse, marking the origin 2 to 3 cm distal to the inguinal ligament and then drawing a line to the ASIS. The flap will follow this axis.
Why is the lateral limit of the flap 10 cm?
This is because the portion of the flap lateral to the ASIS has a random pattern of vascularization. Therefore, because the width of the flap is limited to 10 cm, the lateral limit of the flap is then 10 cm lateral to the ASIS.
Which artery is the groin flap?
FIG 1 • Vascular and regional anatomy of the groin flap, which follows the axis of the superficial circumflex iliac artery.
What nerve pierces the internal and external oblique muscles and courses distally over the iliac?
The 12th thoracic nerv e pierces the internal and external oblique muscles and courses distally over the iliac crest, 5 cm posterior to the ASIS. Do not confuse the lateral femoral cutaneous nerve, which supplies sensation to the lateral thigh, for the 12th thoracic nerve.
When was the groin flap invented?
The groin flap was described in 1972 by McGregor and Jackson 1 for reconstruction of soft tissue defects of the hand. This was once a “workhorse” flap for hand reconstruction; however, with the introduction and advancement of microsurgery, it has fallen out of favor for many indications. Nevertheless, there are still many indications for its use.