What are the long term effects of an uti?
- Confusion
- Disorientation
- Agitation
- Poor motor skills
- Dizziness
- Falling
- Sometimes even depression
What is the treatment for a bacterial infection?
Treatments for Bacterial Skin Infections
- Cellulitis. Mild infections of cellulitis are normally treated with antiobiotic creams or pills at home. ...
- Erysipelas. This form of cellulitis affects the upper layers of the dermis and is often treated using penicillin.
- Folliculitis. Mild folliculitis infections usually run their natural course and clear up in a few weeks. ...
- Furuncles. ...
- Impetigo. ...
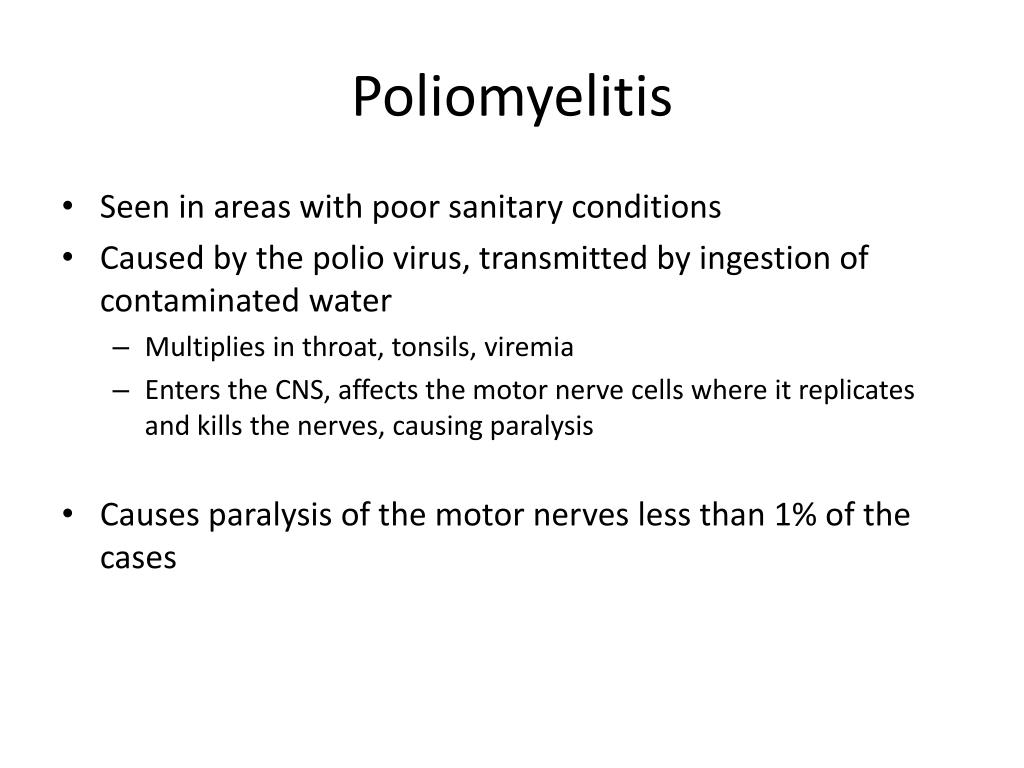
What illnesses are caused by bacteria?
List of diseases caused by bacteria in humans are
- Tuberculosis
- Typhoid
- Cholera
- Dysentery
- Gastric ulcer
- Pneumonia
- Diphtheria
- Plague
- Leprosy
- Gonorrhea. etc. Tuberculosis: One of the most long-standing and widely distributed bacterial disease in human history.
Is there cure for bacterial infections?
Yes, bacterial infections can be cured with antibiotics. There are some strains of bacteria, such as some forms of S. aureus, that are resistant to antibiotics and cannot be cured, so it is important not to overuse antibiotics. Steps can be taken to help prevent bacterial infections in the first place.
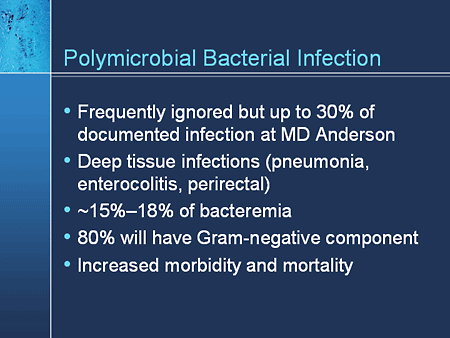
What causes polymicrobial infection?
Polymicrobial infections may be caused by dysbiosis of the urobiome in the urinary tract. Studies have also shown that the urobiome changes constituents in response to host interaction and exogenous factors, such as antibiotics (8,9).
What is the meaning of Polymicrobial?
Medical Definition of polymicrobial : of, relating to, or caused by several types of microorganisms polymicrobial infections.
What does Polymicrobial growth mean?
Polymicrobial growth was defined as mixed flora of more than 100,000 colony forming units per milliliter. Admissions for pyelonephritis were identified by ICD-9 codes, and gestational age at delivery was determined from a research registry.
How are polymicrobial infections treated?
Empirical treatment of polymicrobial infections requires an agent active against both anaerobic and aerobic/facultative bacteria. An aminoglycoside used in combination with an anti-anaerobe agent is commonly used to treat polymicrobial infections.
What does it mean when multiple organisms present in urine culture?
Urine cultures that contain more than one organism are usually considered contaminated. The frequency with which such growth truly represents mixed infection is unknown. Surprisingly few studies have evaluated the clinical significance of polymicrobial growth from urine.
How microorganisms attach themselves to the host tissue?
Bacteria can typically make a variety of different adhesive tips enabling them to attach to different host cell receptors. Cell wall adhesins are surface proteins found in the cell wall of various bacteria that bind tightly to specific receptor molecules on the surface of host cells.
Why does my urine test keep coming back contaminated?
If the urine is not collected in a sterile manner the urine sample may be 'contaminated' by bacteria that originate from the skin or genital area, and not from the urinary tract. This is often described by the clinical laboratory as 'mixed growth bacteria'.
What is polymicrobial growth in urine culture?
Abstract. Urine growing more than one organism is usually considered contaminated. During 1980-1984, among 198 episodes of urosepsis with at least one identical organism in blood and urine, there were 62 with polymicrobial growth from urine.
What is a high bacteria count in urine?
Bacterial colonization in urine is high when the level of bacterial counts is elevated— meaning the number of colonies of a single organism is higher than 100,000 per mL. If the bacteria level in your urine is high and it's causing physical symptoms, you have a symptomatic urinary tract infection (UTI).
What is polymicrobial sepsis?
Polymicrobial sepsis is associated with immunosuppression caused by the predominance of anti-inflammatory mediators and profound loss of lymphocytes through apoptosis, and so deaths directly related to sepsis are twofold higher in polymycrobial sepsis.
What is polymicrobial necrotizing fasciitis?
Necrotizing fasciitis is a rare but potentially fatal disease; it can occur in all parts of the body, including the oral cavity and the perineum. Typically, patients who develop type 1 (polymicrobial) necrotizing fasciitis are immunocompromised in some way.
How does Fournier's gangrene start?
Fournier's gangrene usually happens because of an infection in, or near, your genitals. Sources of the infection can include: Urinary tract infections. Bladder infections.
Is mixed growth in urine an infection?
"Mixed Growth" is used to indicate contamination with vaginal, skin or bowel organisms. The presence of epithelial cells on microscopy also indicates contamination. If pyuria (> 40 WBC) is present, and the specimen culture suggests contamination a repeat sample is advisable, if clinically indicated.
What is polymicrobial BSI?
A polymicrobial BSI was defined as the isolation of more than one pathogen from the same blood sample or from two consecutive blood samples within 24 h.
Is mixed flora a UTI?
The isolation of more than one microorganism from a single urine specimen; mixed flora is known as polymicrobial bacteriuria and the associated condition is polymicrobial UTI.
What is mixed normal urogenital flora?
Because “mixed flora”* implies that at least 2 organisms are present in addition to the identified organism, the urine culture does not meet the criteria for a positive urine culture with 2 organisms or less. Such a urine culture cannot be used to meet the NHSN UTI criteria.
What are polymicrobial diseases?
Polymicrobial diseases involve multiple infectious agents and are referred to as complex, complicated, mixed, dual, secondary, synergistic, concurrent, polymicrobial, coinfections. This new book, a collection of 21 chapters written by a variety of authors, reviews mixed infections in animals and humans. The chapters are gathered into sections on polyviral diseases, polybacterial diseases, viral and bacterial infections, fungal infections, infections resulting from microbe-induced immunosuppression, and a concluding perspective. Polymicrobial diseases described include abscesses, AIDS-related opportunistic infections, conjunctivitis, gastroenteritis, hepatitis, multiple sclerosis, otitis media, periodontal diseases, respiratory diseases, and genital infections. Approximately two-thirds of the chapters deal with human diseases; the others discuss infections in cattle, goats, and pigs.
Does growing two or more microbes in the laboratory prove that a polymicrobial infection is the cause of the?
Growing two or more microbes in the laboratory in a clinical situation does not prove that a polymicrobial infection is the cause of the disease. The editors and authors do not provide a framework similar to that of Robert Koch or Bradford Hill, which one can use to decipher the role (s) of each candidate agent in a polymicrobial infection. An limited discussion is provided on the role of noninfectious factors, such as genetics of the host, retained “hardware”, alcohol in hepatitis, or tobacco use in respiratory diseases. How each of the chapters was selected for inclusion and what other topics were considered is not clear.
What is polymicrobial disease?
Polymicrobial diseases represent the clinical and pathologic manifestations induced by the presence of multiple microorganisms. These are serious diseases whose etiologic agents are sometimes difficult to diagnose and treat.
What are the underlying mechanisms of polymicrobial disease?
First, physical, physiologic, or metabolic abnormalities including stress can predispose the host to polymicrobial disease ( 17, 41, 65 ). Second, alterations induced in the mucosa by one organism favor the colonization of others ( 79 ). Third, synergistic triggering of proinflammatory cytokines increases severity of disease, reactivates latent infections, or favors the colonization of other microorganisms. Fourth, sharing of determinants among organisms allows activities that neither organism possesses individually ( 161 ). Finally, obliteration of the immune system by one organism allows the colonization of others.
How to reproduce polymicrobial disease?
Reproducing polymicrobial disease is often difficult. In some cases, polymicrobial disease can be induced by simply administering comixtures of microorganisms. This approach was successful in inducing experimental chronic nonprogressive pneumonia ( 40, 91, 92 ). In other cases, disease can only be induced by sequential administration of causative agents. This approach was successful in inducing respiratory disease in sheep ( 26, 51, 52, 105) and swine ( 25 ). In swine, P. multocida could not be isolated from pigs challenged with P. multocida alone or after inoculation with porcine reproductive and respiratory syndrome virus. However, P. multocida could be isolated from pigs challenged sequentially with porcine reproductive and respiratory syndrome virus, B. bronchiseptica, and P. multocida. Finally, physical stress may be required. In cattle, abrupt changes in temperature ( 56, 90) and exercise ( 6) increase the numbers of M. haemolytica in the nasopharynx, thus increasing the susceptibility of cattle to respiratory infection.
What diseases were first identified in the 20th century?
Polymicrobial diseases are not new, and infections involving numerous pathogens were recognized early in the 20th century ( 87, 161 ). In animals, foot rot ( 160) and chronic nonprogressive pneumonia ( 40, 91, 92) in sheep were among the first diseases found to have multiple etiologies. Respiratory disease in cattle was also shown early to have multiple etiologies ( 66, 161 ), which are still being characterized ( 67, 164, 165 ). More recently, atrophic rhinitis in swine ( 128) and porcine respiratory disease complex ( 25, 68, 163, 168) have been included, the latter because of the emergence of porcine reproductive and respiratory syndrome virus ( 57, 180 ).
When did the polymicrobial etiology of respiratory disease become established?
In the 1920s , the polymicrobial etiology of respiratory disease was firmly established, and Haemophilus influenzaeor Streptococcus pneumoniaewere routinely found in individuals with viral respiratory disease (79). A similar relationship was seen during the influenza pandemics in 1918, 1957, and 1968–1969.
How do viruses affect the mucosal surface?
Similarly, viral infections of mucosal surfaces contribute to increased incidence of secondary bacterial infections ( 79 ). First, viruses physically damage respiratory epithelium and impair ciliary clearance of bacteria. This is seen in respiratory syncytial virus ( 170) and influenza virus infections ( 178 ). Second, viruses alter epithelial cell surfaces thus creating receptors for bacterial adherence ( 38, 79, 121 ). For example, during replication of influenza virus, neuraminidase and hemagglutinin are inserted into the host cell membranes serving as receptors for S. pneumoniae. Pneumococcal adherence can be blocked by treating influenza A virus-infected cells with antiviral antibodies ( 150) or neuraminidase ( 54 ). Similarly, during replication of respiratory syncytial virus (RSV), glycoproteins F and G are inserted into the host cell membranes serving as receptors for Neisseria meningitidis ( 142 ). Increased amounts of CD14, CD15, and CD18 are also produced which enhance the adherence of nonpiliated N. meningitidis ( 143 ). H. influenzae and S. pneumoniae adhere more readily to RSV-infected cells via P5 fimbriae-binding and platelet-activating factor, respectively. In the latter, RSV infection induces the production of TNF-αand IL-1α ( 48, 49 ), which activates production of platelet-activating factor on endothelial surfaces.
Is polymicrobial disease a neglected concept?
Polymicrobial disease is a rapidly emerging and highly researched area, yet it represents a neglected concept. For example, in recent reviews of host-pathogen interactions, the basic concepts of virulence and pathogenicity were redefined ( 36, 37 ), and new definitions were based on a pathogen's ability to cause damage as a function of the host's immune response ( 37 ). Virulence was defined as a property of the pathogen, which is modulated by host susceptibility and resistance, and disease was defined as a complex outcome, which can arise because of pathogen-mediated damage, hostmediated damage, or both ( 37 ). Unfortunately, these were "single etiologic agent" concepts not seriously addressing polymicrobial infections and diseases.
What is the name of the bacterial infection that occurs before or during labor?
Chorioamnionitis is a bacterial infection that occurs before or during labor. The name refers to the membranes surrounding the fetus: the “chorion” (outer membrane) and the “amnion” (fluid-filled sac). The condition occurs when bacteria infect the chorion, amnion, and amniotic fluid around the fetus. It can lead to a preterm birth ...
What causes chorioamnionitis?
E. coli, group B streptococci, and anaerobic bacteria are the most common causes of chorioamnionitis.
What percentage of women with chorioamnionitis have bacteremia?
About 3 to 12 percent of women with chorioamnionitis have bacteremia. This condition also increases the need for a cesarean delivery. Of those who have a cesarean delivery, up to 8 percent develop a wound infection and approximately 1 percent develop a pelvic abscess (collection of pus ).
What are the risk factors for a baby to have a ruptured membrane?
The most common risk factors for this condition include: young maternal age (less than 21 years old) low socioeconomic status. first pregnancy. long labor. membranes that are ruptured (water has broken) for an extended period of time. premature birth.
Can chorioamnionitis cause preterm birth?
It can lead to a preterm birth or serious infection in the mother and the baby. It’s most commonly seen in preterm births; it’s also seen in approximately 2 to 4 percent of full-term deliveries. Chorioamnionitis is also known as “amnionitis” or “intra-amniotic infection.”.
Can amniotic fluid infected babies?
The amniotic fluid and placenta — and baby — can become infected.
Is chorioamnionitis a medical emergency?
Chorioamnionitis is usually considered a medical emergency. The condition can lead to serious complications, including: bacteremia (infection in the bloodstream) endometritis (infection in the lining of the uterus) need for cesarean delivery. heavy blood loss with delivery. blood clots in the lungs and pelvis.